Neuroanatomy and Lesion Localization
Aaron D. Boes
Verne S. Caviness
SKULL ANATOMY
Description
The brain is protected by bony encasement of the skull. See Figure 2.1 for anatomy of bones, sutures, and fontanelles. Sphenoid bone is major component of middle cranial fossa (not visible in figure) and surrounds anterior temporal lobes and houses pituitary gland.
Craniosynostosis
Premature closure of a suture: sagittal → scaphocephaly, unilateral coronal → anterior plagiocephaly, unilateral lambdoid → posterior plagiocephaly, metopic → trigonocephaly, bilateral coronal → brachycephaly.
MENINGES, VENTRICLES, AND CEREBROSPINAL FLUID (CSF)
Meninges
The brain is protected by 3 layers of meninges (Fig. 2.2): (1) Dura mater (“tough mother”): outermost layer, tough connective tissue adherent to skull. Separates into outer periosteal and inner meningeal layers around dural venous sinuses. Inner projections form falx cerebri and tentorium cerebelli. (2) Arachnoid: middle layer, surrounds CSF-filled subarachnoid space. (3) Pia mater: innermost layer, closely adherent to the brain.
Pachymeninges (thick meninges) = dura. Leptomeninges (thin meninges) = arachnoid + pia.
Meningeal Spaces
EPIDURAL SPACE: Potential space between skull periosteum and dura. Contains middle meningeal artery; laceration → epidural hematoma (arterial, convex, not cross suture lines, often overlying skull fracture). SUBDURAL SPACE: Potential space between dura and arachnoid. Traversed by bridging veins from subarachnoid space to dural venous sinuses; rupture → SDH (venous, concave, can cross suture lines). SUBARACHNOID SPACE: actual space between arachnoid and pia. Contains CSF and vessels. SAH often from spontaneous aneurysm rupture or trauma; classic symptom is “thunderclap” headache.
Ventricular System and CSF Flow (Fig. 2.3)
CSF PRODUCTION: Produced by choroid plexus: a modified capillary network lying mostly within the lateral ventricles.
CSF FLOW: From 2 lateral ventricles → interventricular foramina of Monro → 3rd ventricle → cerebral aqueduct of Sylvius (within midbrain) → 4th ventricle (at pontomedullary junction on posterior surface of
brainstem) → exits ventricular system via foramen of Magendie (midline) and 2 foramina of Luschka (lateral) → subarachnoid space.
brainstem) → exits ventricular system via foramen of Magendie (midline) and 2 foramina of Luschka (lateral) → subarachnoid space.
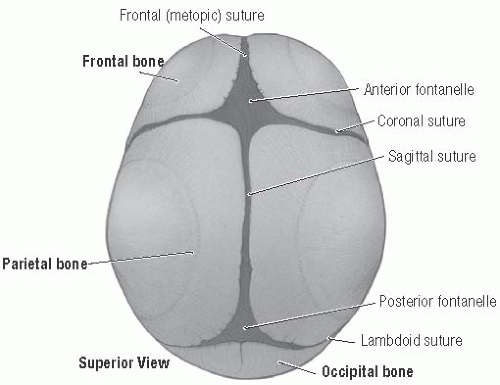 FIGURE 2.1 Skull Anatomy. (From Agur AM, Dalley AF. Grant’s Atlas of Anatomy, 13th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2012.) |
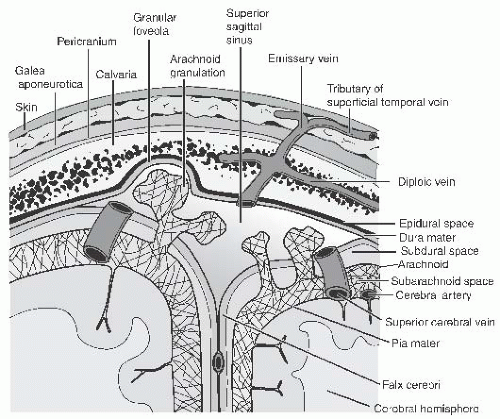 FIGURE 2.2 Scalp, Meninges, and Associated Structures. (From Chung KW, Chung HM. Gross Anatomy, 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2011.) |
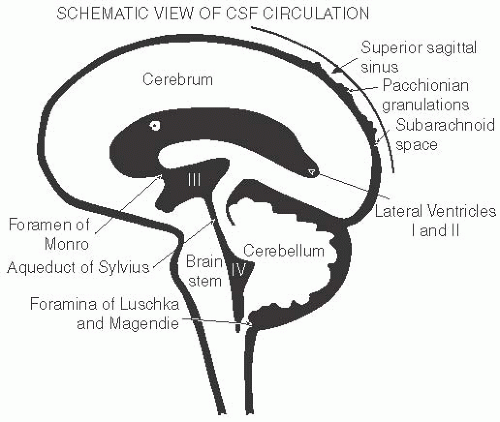 FIGURE 2.3 Ventricles and CSF Flow. (From Cohen ME, Duffner PK. Weiner & Levitt’s Pediatric Neurology, 4th ed. Philadelphia: Lippincott Williams & Wilkins; 2003.) |
CSF REABSORPTION: Reabsorbed into venous system at arachnoid granulations penetrating into dural sinuses.
HYDROCEPHALUS: Noncommunicating/obstructive: Blockage within ventricular system preventing outflow (commonly at cerebral aqueduct). Communicating: Blockage of CSF after it exits ventricles; disruption of reabsorption in subarachnoid space. Symptoms: HA, irritability/lethargy, N/V, bulging fontanelle (in infants), papilledema, ophthalmoplegia (commonly CN VI palsy, vertical gaze palsy/“sunsetting” from pressure on dorsal midbrain).
VASCULAR ANATOMY
See Figure 2.4 for overview of vascular anatomy. Stroke syndromes are described in subsequent sections.
OVERVIEW OF CNS TOPOGRAPHY
Major divisions of the CNS (Fig. 2.5) include the spinal cord, brainstem, diencephalon (thalamus and hypothalamus), cerebellum, basal ganglia (BG), and cerebral cortex. The cerebral cortex, forming the surface of the forebrain, is characterized by a species-typical pattern of gyral elevations (protrusions) and sulci (valleys) between the gyri. The interhemispheric fissure divides the right and left hemispheres, which are connected by the corpus callosum, a massive white matter commisural tract seen in the midline brain. The central sulcus (“Rolandic fissure”) separates the frontal and parietal lobes. The lateral sulcus (“Sylvian fissure”) forms superior boundary of the temporal lobe.
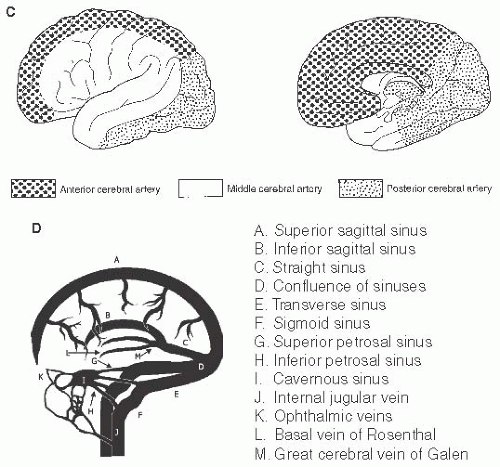
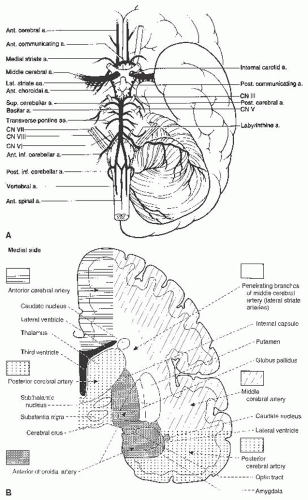 FIGURE 2.4 A: Arteries of the base of the brain and brainstem, including the arterial circle of Willis. B: Coronal section through the cerebral hemisphere at the level of the internal capsule and thalamus showing the major vascular territories. C: Cortical territories of the 3 major cerebral arteries. (A-C from Fix JD . High-Yield Neuroanatomy, 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2009.) D: Venous anatomy. (From Greer DM, et al. Pocket Neurology. Philadelphia, PA: Lippincott Williams & Wilkins; 2010.) |
Cerebral Cortex
Frontal Lobe (Fig. 2.6A)
PRIMARY MOTOR CX (BA 4): Lesion causes contralateral UMN deficits most prominent in distal muscles/fine motor skills. Legs represented on medial surface. Moving inferiorly along lateral surface: trunk/UE/face. PREMOTOR CX (BA 6): Involved in motor planning. Lesion causes apraxia ± contralateral weakness. INFERIOR FRONTAL GYRUS: Dominant side
lesion causes Broca’s aphasia (BA 44, 45), nondominant side involved in prosody, nonverbal communication. MIDDLE FRONTAL GYRUS: Includes frontal eye fields (FEF, BA 8). FEF directs gaze toward contralateral side (e.g., left FEF directs gaze to right). Lesion = gaze directed toward lesion. Stimulation = gaze directed away (e.g., look away from seizure focus). SUPERIOR FRONTAL GYRUS: Involved in working memory, attention. ORBITOFRONTAL AND MEDIAL PREFRONTAL/ANTERIOR CINGULATE: Localization often difficult; may cause disinhibition, emotional dysregulation, lack of empathy, lack of planning/myopia for the future. Posterior lesions may cause akinetic mutism, abulia.
lesion causes Broca’s aphasia (BA 44, 45), nondominant side involved in prosody, nonverbal communication. MIDDLE FRONTAL GYRUS: Includes frontal eye fields (FEF, BA 8). FEF directs gaze toward contralateral side (e.g., left FEF directs gaze to right). Lesion = gaze directed toward lesion. Stimulation = gaze directed away (e.g., look away from seizure focus). SUPERIOR FRONTAL GYRUS: Involved in working memory, attention. ORBITOFRONTAL AND MEDIAL PREFRONTAL/ANTERIOR CINGULATE: Localization often difficult; may cause disinhibition, emotional dysregulation, lack of empathy, lack of planning/myopia for the future. Posterior lesions may cause akinetic mutism, abulia.
Temporal Lobe
ANTEROMEDIAL: Includes hippocampus (lesion = anterograde memory deficit), amygdala (lesion = fearlessness). SUPERIOR TEMPORAL/WERNICKE’S AREA (BA 22): Lesion = verbal comprehension impairment on dominant side (Wernicke aphasia), sensory dysprosody on nondominant side. White matter lesion deep to temporal lobe may cause contralateral
superior quadrantanopia. INFERIOR TEMPORAL LOBE: “What” visual pathway involved in visual recognition. Occipitotemporal junction lesion may cause prosopagnosia (inability to identify faces).
superior quadrantanopia. INFERIOR TEMPORAL LOBE: “What” visual pathway involved in visual recognition. Occipitotemporal junction lesion may cause prosopagnosia (inability to identify faces).
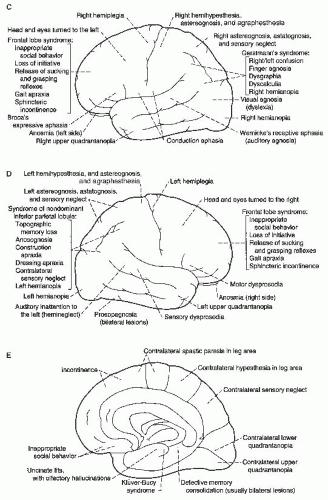
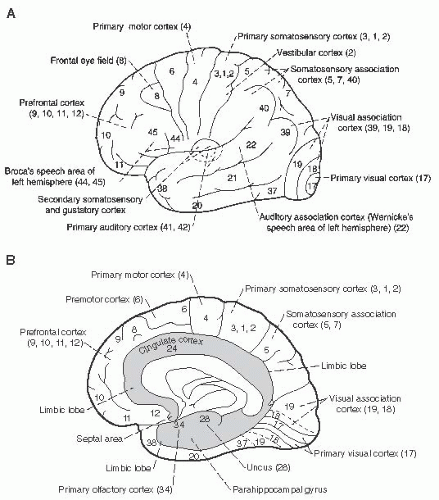 FIGURE 2.6 Cerebral Cortex Anatomy and Syndromes of Cortical Lesions. A, B: Surface of the cerebral cortex: Lateral and medial surface of the cerebral cortex with Brodmann’s areas. C, D, E: Focal destructive hemispheric lesions and the resulting syndromes. (From Fix JD. High-Yield Neuroanatomy, 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2009.) |
Parietal Lobe
PRIMARY SOMATOSENSORY CX (BA 3, 1, 2): Lesion = hemihypesthesia and astereognosis of contralateral face/body. Homunculus parallels motor cortex: Legs on medial surface; trunk/UE/face moving inferiorly along lateral surface. SUPERIOR PARIETAL (BA 5, 7): Lesion = contralateral neglect (particularly nondominant side), contralateral astereognosis, astatognosis
(inability to recognize body position in space). INFERIOR PARIETAL: Angular gyrus (BA 39) caps the superior temporal sulcus. Supramarginal gyrus (BA 40) caps Sylvian fissure. Inferior parietal lesion on dominant side may cause Gerstmann syndrome: L-R confusion, acalculia, alexia, finger agnosia, agraphia. Nondominant lesion: anosognosia, construction apraxia, neglect, apraxia for dressing, topographic memory problems. BL parieto-occipital infarcts cause Balint syndrome: simultagnosia (inability to perceive visual world in coherent fashion, often as single objects without Gestalt view), optic ataxia, ocular apraxia. CL lower quadrantanopsia: may result from underlying optic radiations en route to cuneate gyrus. POSTEROMEDIAL CX: Includes medial parietal cortex and posterior cingulate. Bilateral injury severely impairs consciousness. Region is active in self-referential tasks.
(inability to recognize body position in space). INFERIOR PARIETAL: Angular gyrus (BA 39) caps the superior temporal sulcus. Supramarginal gyrus (BA 40) caps Sylvian fissure. Inferior parietal lesion on dominant side may cause Gerstmann syndrome: L-R confusion, acalculia, alexia, finger agnosia, agraphia. Nondominant lesion: anosognosia, construction apraxia, neglect, apraxia for dressing, topographic memory problems. BL parieto-occipital infarcts cause Balint syndrome: simultagnosia (inability to perceive visual world in coherent fashion, often as single objects without Gestalt view), optic ataxia, ocular apraxia. CL lower quadrantanopsia: may result from underlying optic radiations en route to cuneate gyrus. POSTEROMEDIAL CX: Includes medial parietal cortex and posterior cingulate. Bilateral injury severely impairs consciousness. Region is active in self-referential tasks.
Occipital Lobe
Primarily visual. CUNEUS (above calcarine sulcus) represents lower visual field. LINGUAL GYRUS (below calcarine sulcus) represents superior visual field. Fovea represented on OCCIPITAL POLE. Anton syndrome: cortical blindness without awareness of deficit, often seen with lesion of association visual cortices; Alexia without agraphia may result from dominant occipital lesion and splenium of CC.
Major Stroke Syndromes Involving Cerebral Cortex
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree