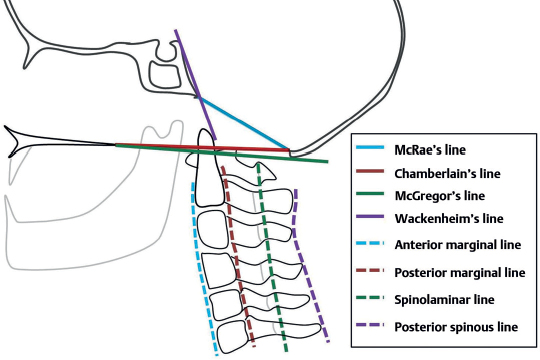
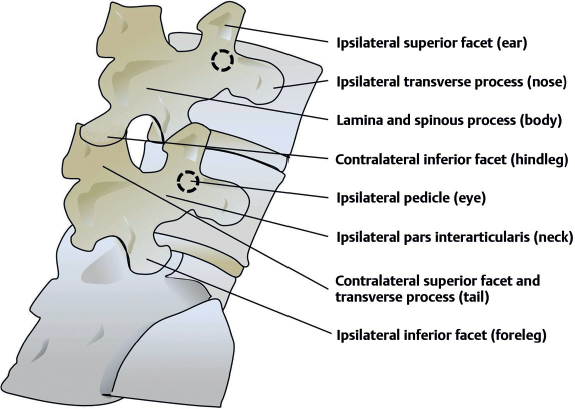
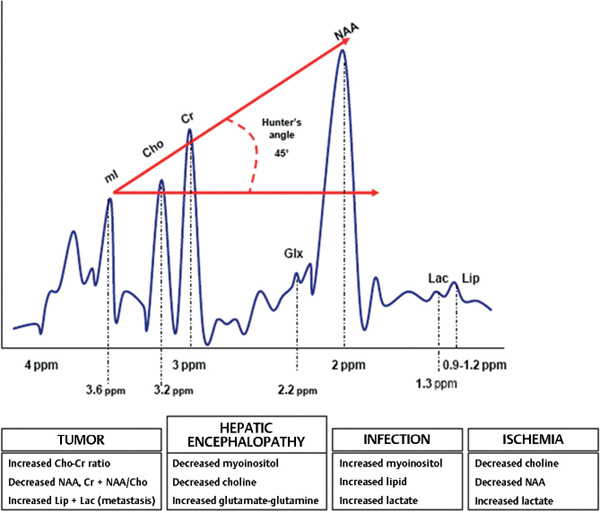
23 What are the four main contour lines of the cervical spine on plain film? 1. Anterior marginal line: adjacent to anterior cortical surfaces of vertebral bodies; follows the anterior longitudinal ligament 2. Posterior marginal line: adjacent to posterior cortical surfaces of the vertebral bodies; follows the posterior longitudinal ligament; marks anterior margin of spinal canal 3. Spinolaminar line: follows the base of each spinal process 4. Posterior spinous line: follows the spinous process tips What are the four main basilar lines? 1. McRae’s line1: line drawn from tip of basion to tip of opisthion; marks the foramen magnum; odontoid should not pass above this line on plain film 2. McGregor’s baseline2: line drawn from posterior tip of hard palate to inferior edge of opisthion (most caudal portion of occiput); the dens should not be more than 4.5 mm above this line on plain film 3. Chamberlain’s line3: line drawn from tip of opisthion to posterior tip of hard palate; no more than 3 mm of dens should be above this line 4. Wackenheim’s clivus-canal line4: line connecting basion to posterior clinoids; follows the course of the clivus; odontoid should be tangential to or below this line Fig. 23.1 Cervical spine plain film contour and basilar lines. What is basilar invagination? Superior displacement of the cervical spine and odontoid process through the foramen magnum What clinical conditions are often associated with basilar invagination? Down syndrome, Klippel-Feil syndrome, Chiari malformation, syringomyelia, rheumatoid arthritis What is the basion-axial interval (BAI)? Distance between the posterior tip of the basion and a line extending rostrally/superiorly from the posterior cortical surface of C2 (i.e., the posterior axial line or Harris line) on lateral C-spine plain film What is the basion-dental interval (BDI)? The distance from the inferior tip of the basion to the superior tip of the dens on lateral C-spine plain film What are the normal values for BAI and BDI in adults? In children? Adults: BAI and BDI both <12 mm (BAI may be negative in adults) Children: BAI <13 mm (BDI unreliable in children) The distance between the superior articular surface of the atlas and the inferior articular surface of the occipital condyle on lateral C-spine plain film; also known as the atlanto-occipital interval (AOI). In adults the AOI is normally ≤2 mm (≤5 mm in children) on plain film. What conditions should be suspected with an elevated BAI, BDI, or AOI? Atlanto-occipital dislocation What deficits may be seen with atlanto-occipital dislocation? The most common presentation is death. Surviving patients may be neurologically intact or may have lower cranial nerve deficits and/or cord injury. What is the rule of Spence?5 If the lateral overhang of C1 on C2 is >7 mm on open-mouth odontoid x-ray, the transverse atlantal ligament is likely to be disrupted. What imaging modality may be ordered to directly assess the integrity of the transverse atlantal ligament (TAL)? MRI (CT may also reveal bony injuries in the region of TAL insertion on the C1 tubercles, in which case TAL disruption may be inferred.) What is the atlantodental interval (ADI)? The distance between the anterior surface of the dens and the posterior cortical surface of the anterior arch of C1 on lateral plain-film; normally ≤3 mm in males, ≤2.5 mm in females, and ≤4 mm in children What is the normal average bony spinal canal diameter between C3 and C7? Measured from the posterior marginal line to the spinolaminar line is normally around 13 to 15 mm. Measurements less than 12 mm are considered stenotic in adults. What is the “bow-tie” sign? On lateral plain film or CT/MRI, visualization of bilateral facets at a given level (facets are normally superimposed on lateral film so that only one set of facets can be seen) may suggest unilateral locked facets.6 What is the “Scotty dog” on lumbar x-rays? A characteristic dog-shaped image seen on oblique x-rays of the lumbosacral spine often used to assess the pars interarticularis (formed by the neck of the dog). • Nose = transverse process • Eye = pedicle • Ear = superior facet • Neck = pars interarticularis • Foreleg = ipsilateral inferior facet • Body = lamina • Hind leg = contralateral inferior facet or spinous process • Tail = contralateral superior facet or transverse process Pars defects may be seen as a break in the neck of the Scotty dog or as a “dog collar.” Fig. 23.2 Lumbosacral spine plain film: “Scotty dog.” CT is best for visualizing which tissues? Bone (especially fine bony detail) Acute parenchymal hemorrhage or hemorrhagic infarction (MRI may be useful as well), subarachnoid hemorrhage (CTA may be useful as well), headache/migraine (MRI may be useful as well), first-time seizure, conductive hearing loss (visualization of bony detail is required), focal neurological deficits What features of CT make it ideal for evaluating acute mental status changes, suspected acute hemorrhage or stroke, or intracranial or spinal trauma? It can be obtained rapidly and is available widely. Why does contrast highlight intracranial pathology? The normal blood–brain barrier (BBB) is not permeable to ionic contrast media. Thus, any contrast in the brain represents a defect in the BBB caused by neoplasm, stroke, infection, etc. What is the typical radiation dose received from a head CT? 3 to 5 mSv (millisieverts) or 0.3 to 0.5 rem (Roentgen-equivalent man units). This range may vary widely across institutions. In comparison, a long airline flight results in 0.005 rem to the body, a chest x-ray results in 0.04 rem to the chest, a spine CT results in 5 rem, and a cerebral arteriogram results in 20 rem. What is the most frequent complication of CT? Pathology associated with IV contrast agents, particularly ionic agents (allergic reactions, contrast nephropathy) How is contrast nephropathy diagnosed? A rise in serum creatinine of at least 1 mg/dL within 48 hours of contrast administration What are some of the risk factors for contrast nephropathy? Age >80 years, serum creatinine >2.0 mg/dL, diabetes mellitus, dehydration, paraproteinemia (e.g., multiple myeloma), single kidney, use of nephrotoxic medications What agents may be given to diabetics or those with mild renal insufficiency to mitigate the harmful effects of IV contrast media? N-acetylcysteine (Mucomyst) in addition to IV hydration What is the differential for an intracranial hyperdensity on noncontrast CT? Acute blood, calcium Which structures are often physiologically calcified and may appear hyperdense on noncontrast CT? Basal ganglia, choroid plexus, pineal gland What is Xe-CT? Xenon-assisted CT. Patients inhale xenon during image acquisition, which may be used to assess changes in cerebral blood flow (e.g., to monitor for vasospasm in SAH patients) What is CTA? CT angiography, in which IV contrast is rapidly injected immediately prior to image acquisition, allowing for imaging of cerebral (and other) blood vessels What are some limitations of CTA? Vessels coursing perpendicular to the CT plane are less visible. What is CTP? CT perfusion, in which several slices of interest are selected from a noncontrast CT scan. These regions are scanned while IV contrast is injected before and after a bolus of acetazolamide (ACZ) for 10 to 15 minutes. What abnormalities may be revealed by CTP? Flow-significant stenosis (decreased cerebral blood volume and flow will be seen prior to ACZ injection), steal phenomenon (after ACZ injection, cerebral blood volume [CBV], and cerebral blood flow [CBF] will decrease with or without increases in contralateral territory) What is the differential diagnosis for a ring-enhancing lesion on CT/MRI? Tumor (astrocytoma, metastasis, ring will typically be irregular and inconsistent), stroke, abscess (ring is usually regular and complete), lymphoma, radiation necrosis, toxoplasmosis, neurocysticercosis How may vasogenic and cytotoxic edema be differentiated on CT/MRI? In vasogenic edema, the BBB is compromised, leading to extravasation of proteins that may enhance. In cytotoxic edema, the BBB is intact, and thus no enhancement is seen on CT/MRI. When is myelography indicated? When spinal cord or nerve root compression is suspected (e.g., by herniated disks, tumors, trauma); may reveal medullary abnormalities as well as intradural and extradural lesions; especially useful in patients with contraindications to MRI Where is the radiopaque dye injected in a myelogram? Into the subarachnoid space. Typically injected into the lumbar subarachnoid space via lumbar puncture but C1–2 puncture may be used for cervical myelogram. What complications/risks are associated with myelography? Approximately 40% of patients experience either headache or nausea/vomiting. Other complications include back pain, confusion, arachnoiditis (more common with oil-based contrast such as iophendylate [Pantopaque™]), inadvertent IV injection of contrast, damage to nerve roots or blood vessels (rare), or seizures (rare). What are some contraindications to myelography? Current anticoagulation, allergy to iodinated contrast Why is a CT scan sometimes performed following the myelogram? Postmyelogram CT increases the sensitivity and specificity of a myelogram.7 Describe how a magnetic resonance image is acquired. The patient is placed within a large magnetic field that polarizes the protons within the patient’s body (mostly contained within water and adipose tissue). A radiofrequency is then imparted on the body, which excites the protons, elevating their energy state. As the protons “relax” back to their initial state, they release radiofrequency energy (the “echo”), which is detected and transformed by Fourier analysis into an MR image. MRI is best for visualizing which tissues? Soft tissues, including the CNS and PNS For what symptoms or suspected diagnoses is MRI an appropriate initial workup? Acute parenchymal hemorrhage, subacute/chronic hemorrhage, ischemic infarction, carotid or vertebral dissection or vertebral basilar insufficiency (MRA may be useful as well), suspected mass lesion (neoplastic, infectious, etc., with contrast), vascular malformation (with or without angiography), white matter disorders, demyelinating disease, shear injury, partial complex or refractory seizures, cranial neuropathy, spine disorders (back pain with focal deficits, suspected stenosis, spondylosis, infection, myelopathy, AVM) What are some contraindications to MRI? Relative: pregnancy (contrast administration should be avoided in pregnant women), programmable-shunt valve Absolute: implants or fragments of non-MRI compatible metal, cardiac pacemaker/defibrillator, cochlear implants, infusion pumps, Swan-Ganz catheter, spinal cord stimulator, older aneurysm clips What is nephrogenic systemic fibrosis (NSF)? A systemic fibrotic reaction seen rarely as a complication of gadolinium IV administration in patients with renal insufficiency (mean delay to symptom onset 2 weeks)8 How does the intensity of moving blood vary on T1- and T2-weighted MRI? Fast-moving blood (e.g., most arterial blood) returns no signal and appears dark on normal T1-weighted imaging (T1WI) or T2-weighted imaging (T2WI) (known as a “flow void”). Slow-moving blood (e.g., venous blood, blood immediately distal to arterial stenosis) may appear bright. What is MRA? Magnetic resonance angiography. It is a technique that makes use of the flow phenomena seen in MRI to highlight the vessels as in a conventional angiogram. What are some limitations of MRA compared with conventional angiography? MRA has a lower spatial resolution than conventional angiography, and thus may make diagnosis of abnormalities (particularly small-vessel abnormalities) more difficult. MRA does not account for flow patterns and timing that a dynamic conventional angiogram can demonstrate. What structures are better visualized by T1-weighted MR images? Fat, subacute hemorrhage (>48 hours old), onyx, melanin. T1WI is usually considered best for imaging anatomy as opposed to pathology. White matter contains more fat than gray matter and is thus hyperintense to gray matter on T1WI. What structures are better visualized by T2-weighted MR images? Water (CSF, edema). T2WI is usually considered best for imaging pathology. Gray matter typically contains more water than white matter and is thus hyperintense to white matter on T2WI. What is a FLAIR MRI? Fluid-attenuated inversion recovery image. Similar to T2WI except CSF is dark. Periventricular lesions (e.g., MS plaques) may appear more prominent. What is a STIR MRI? Short tau inversion recovery image. Known as a “fat-suppression image” due to the fact that fat is hypointense. May be useful in spine for showing bone edema. How does the appearance of intraparenchymal brain hemorrhage change over time on T1WI versus T2WI? Mnemonic for acute to chronic appearance is “Itty bitty baby daddy” or “ID BD BB DD.” T1 T2 Hyperacute (4–6 h) Isointense Bright Acute (7–72 h) Isointense Dark Subacute (4–7 d) Bright Dark Subacute 2 (1–4 wks) Bright Bright Chronic (months) Dark Dark What is DWI? Diffusion-weighted imaging. The image is sensitive to brownian motion (diffusion) of water molecules. Actively diffusing water appears dark on DWI, whereas nondiffusing (or diffusion-restricted) water appears bright. What is T2 “shine-through”? DWI is based on a T2WI, and any structures appearing bright on T2 may also appear bright on DWI; thus, a bright signal on DWI may be due to restricted diffusion or T2 shine-through. How is T2 shine-through differentiated from areas of true restricted diffusion? The ADC (apparent diffusion coefficient) map: areas of true restricted diffusion will be dark on the ADC, whereas T2 shine-through will be bright. What is the differential diagnosis of an area of bright signal on DWI? Acute ischemia or infarct (DWI changes may be seen within minutes of ischemia; TIAs often produce DWI abnormalities), abscess, active MS plaques, certain tumors (e.g., epidermoid cysts, some meningiomas) What is a FIESTA protocol MRI? Fast imaging employing steady-state acquisition. A high-resolution, thin-slice T2 MRI using CSF as a contrast medium. Often used to evaluate inner ear structure, the auditory nerve, vestibular schwannoma, and posterior fossa vasculature (vascular compression of trigeminal nerve in trigeminal neuralgia). What is an MP-RAGE MRI? Magnetization-prepared rapid gradient with echo, a high-resolution three-dimensional T1 image What can magnetic resonance spectroscopy (MRS) distinguish? Mnemonic is T-PRIDE: Tumors from nontumoral lesions including edema Predicting tumoral grade Residual tumor versus radiation necrosis Infections (abscess)/Ischemia (stroke) Diagnosis of gliomatosis cerebri Encephalopathies (HIV, hepatic, etc.)/Edema What is MRS based on? The detection of metabolites that have a concentration of at least 0.5 to 1.0 mM (millimolar) How does MRS work? By placement of a voxel in the region of interest and comparing the relative concentration of metabolites in that region How many milliliters of brain tissue are included in single-voxel MRS? Approximately 8 cc Does contrast affect the metabolic results? No, but it allows better positioning of the voxel. How long does it extend standard MRI time? By about 15 to 30 minutes Is it reimbursed by Medicare and Medicaid (in the U.S.)? No, not currently Why is it not covered? In part due to the lack of studies of its cost-effectiveness or studies based on the effect on patient health to support the test What are the main peaks in 1H-MRS (hydrogen MRS) and their meaning? Myoinositol: membrane precursor/glial marker Choline (Cho): cellular and membrane turnover/density Creatinine (Cr): cell metabolism and energy store N-acetyl-aspartate (NAA): Neuronal viability and density Glutamate–Glutamine (Glu-Gln or Glx): neuronal amino acids Lactate (Lac): cell anaerobic metabolism Lipid (Lip): cell necrosis (increase in tumor/infections) Which peaks are considered physiologic? Choline, creatinine, and NAA Which two peaks are undetected in normal brain? Lactate and lipid peaks Which two peaks appear both in tumors and in nonneoplastic diseases? The same two peaks: lactate and lipids! Metastases usually have elevation of which peak? Lipids and lactate are usually identified more frequently than normal tissue. Fig. 23.3 Normal MRS peaks.
Neuroimaging
23.1 Plain Films
23.1.1 Important Lines and Planes
23.1.2 Important Measurements and Indexes
23.2 CT, Xenon (Xe)-CT, CT Angiography (CTA)
23.3 Myelography
23.4 MRI/MR Angiography (MRA)/Functional MRI (fMRI)
23.5 MRI Sequences (T1, T2, FLAIR, DWI, ADC, EG, SWI)
23.6 Magnetic Resonance Spectroscopy (MRS)
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Neuroimaging
Only gold members can continue reading. Log In or Register to continue




