Neuroimaging of Common Neurologic Conditions
Jordan Rosenblum
Most common neurologic conditions are imaged using CT, MRI, or both. In the emergent setting, CT is still the most commonly utilized modality. Patients with trauma or a suggestion of acute intracranial hemorrhage are routinely imaged with CT scans, whereas those with findings suggestive of ischemic stroke may be triaged to either CT or MRI. Frequently, the decision rests on the availability of the modality and the time needed to obtain the study. Advances in neuroimaging allow greater specificity in identifying metabolic and physiologic differences between normal tissue and pathology. Some of the most exciting advances include the use of diffusion-weighted imaging (DWI) with MRI that can demonstrate physiologic change within minutes of ischemic change, MR spectroscopy that can identify abnormal metabolites and help in differentiating pathology such as recurrent tumor versus radiation necrosis, and functional MRI (fMRI) that can be used to localize specific functional areas in the brain. The choice of most appropriate imaging modality is presented according to clinical presentation. The information available with medical imaging carry with it specific risks that must be balanced against diagnostic gain. Ionizing radiation from CT may result in significant radiation dose, especially when multisequence scans are performed. Although the actual risk of cancer induction is still an open debate, it is clear that scans should only be ordered that are absolutely necessary and that will affect patient management. Other risks to consider from imaging have been described from contrast use in both CT and MRI. Iodinated contrast can lead to a contrast-induced nephropathy in patients with preexisting renal insufficiency. Recently, gadolinium contrast has been linked to nephrogenic systemic fibrosis (NSF), a rare scleroderma-like systemic disease in patients with renal insufficiency. Current recommendations are to either forgo gadolinium contrast in patients in moderate renal in sufficiency, or if medically indicated, reduce the dose and use one of the agents believed to be associated with less risk of NSF. Patients with severe renal failure should in most cases not receive gadolinium contrast.
I. TRAUMA
CT is the primary imaging modality in trauma because of ready availability, speed, ability to detect bony abnormalities, and superior accuracy in detecting acute intracranial blood. High-resolution, fast CT scanners are routinely installed either within emergency departments or in close proximity. CT is performed routinely in trauma patients, often including those without focal neurologic signs to screen for occult injury. Widely accepted standards for patient selection in this setting are still controversial.
MRI in the setting of acute trauma is still a secondary modality. The most important indication is in evaluating for diffuse axonal injury in which diffuse brain injury may be seen in the presence of a normal head CT. MRI may also demonstrate small extra-axial hemorrhages not seen by CT, particularly in the subtemporal and subfrontal regions.
A. Closed head injury.
CT imaging parameters in trauma should include a narrow window (for acute blood), an intermediate window (for subacute blood), and a wide (bone) window. Acute blood may be present in the form of intracerebral (contusion), epidural, or subdural hematomas and subarachnoid hemorrhage (SAH). Fractures are well-evaluated on bone windows and from coronal and sagittal reconstruction images. Patients with acute trauma and favorable initial coma scores usually fare well and do not require extensive follow-up imaging. In patients with moderate or severe trauma, or low initial Glasgow Coma Score, sequential CTs allow evaluating the course of the initial trauma and the effects of therapy, including extension of initial hemorrhage, rehemorrhage, cerebral edema, herniation,
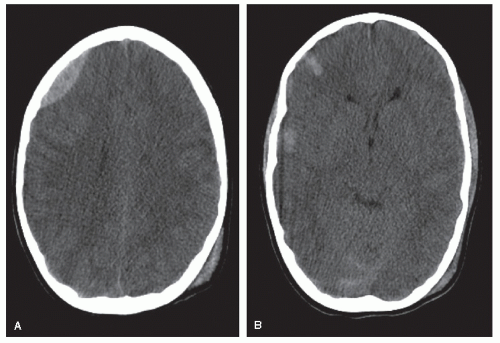
response to external ventricular drainage, and intracranial pressure monitors. Diffuse cerebral edema, more common in younger patients, causes effacement of CSF spaces and may result in herniation (tonsillar, transtentorial, and subfalcine). In patients who come to medical attention several days or weeks after head trauma, with worsening headaches or seizures, MRI may be preferred because subacute hematomas may be isodense on CT, and therefore difficult to see. MRI is superior in evaluating for the presence of blood products in the brain parenchyma (Fig. 32.1A and B).
response to external ventricular drainage, and intracranial pressure monitors. Diffuse cerebral edema, more common in younger patients, causes effacement of CSF spaces and may result in herniation (tonsillar, transtentorial, and subfalcine). In patients who come to medical attention several days or weeks after head trauma, with worsening headaches or seizures, MRI may be preferred because subacute hematomas may be isodense on CT, and therefore difficult to see. MRI is superior in evaluating for the presence of blood products in the brain parenchyma (Fig. 32.1A and B).
B. Penetrating head injury.
CT is the modality of choice in patients with penetrating head injuries. Metallic objects (shrapnel) and glass appear hyperdense on CT, whereas wood objects appear hypodense (air-containing). CT permits an excellent evaluation of the extent of bone damage, and that of the underlying parenchyma, including hemato mas, edema, infarction, and herniation.
C. Cervical spine injury.
Plain X-rays remain the first-line imaging method in patients with cervical spine trauma and should include at least anteroposterior, lateral, and openmouth (odontoid) views. Cervical spine CT offers submillimeter resolution allowing the detection of subtle fractures not seen on plain films. MRI is used to evaluate for spinal cord injury, which appears bright on T2 pulse sequences and dark on gradient echo sequences because of the magnetic susceptibility effect of acute blood.
D. Vascular injury.
Blunt injury to the neck may result in traumatic arterial dissections, pseudo-aneurysms, or occlusions. In stable patients, magnetic resonance angiography (MRA) or CT angiography (CTA) are excellent imaging methods. Unstable patients may go directly to angiography, particularly if endovascular management is contem plated. Penetrating injuries may result in similar lesions, in addition to significant bleed ing from both arterial and venous (jugular vein) injuries. CTA is the imaging method of choice in these patients because current fast scanners allow the evaluation of large anatomical areas with high-resolution and limited-contrast administration. Unstable patients may also require emergency angiography and possibly lifesaving endovascular occlusion of a bleeding artery.
II. HEADACHES
Headache is one of the most common indications for neurologic consultation, with 50% of adults being seen for a severe headache at least once in their life. Fortunately, the vast majority have a benign origin. Pain sensitive structures in the cranial area include the scalp, the scalp blood vessels, head and neck muscles, dural sinuses, the dura and large cerebral arteries at the skull base, meningeal arteries, and pain sensitive fibers of the fifth, ninth, and tenth cranial nerves. Serious conditions that cause headaches include hemorrhage (subarachnoid, subdural, and intracerebral), infections (meningitis and brain abscess), tumors (primary or metastatic), hydrocephalus, and hypertensive crises. Patients at higher risk for significant pathology include those with (1) severe headache of sudden onset; (2) mental status changes, fever, focal neurologic deficits, or seizures; and (3) onset after the age of 50.
A. Acute headaches.
Acute headache associated with nausea, vomiting, nuchal rigidity, and transient alteration in mental status is suggestive of SAH and should prompt immediate evaluation. CT is currently the preferred neuroimaging method for SAH, with reported accuracy rates in the 98% to 99% range.
1. SAH and aneurysms.
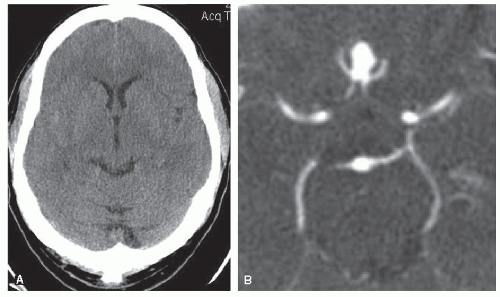
Nontraumatic SAH is caused by a ruptured intracranial aneurysm in 80% to 85% of adult patients (Fig. 32.2A and B). About 10% of patients with SAH, usually in the younger age group, have a nonaneurymal perimesencephalic hemorrhage, a benign and self-limiting venous hemorrhage. Catheter angiography remains the gold standard to evaluate SAH, followed by endovascular or surgical aneurysm obliteration if an aneurysm is identified. CTA is increasingly used as a reliable replacement for cerebral angiography, including for the surgical planning of ruptured and unruptured aneurysms. Uncommon causes of SAH include cerebral and dural arteriovenous malformations (AVMs), arterial dissections, cerebral tumors, vasculitides, and moyamoya disease.
2. Intracerebral hemorrhage and other causes of acute headache.
Intracerebral hemorrhage is most commonly caused by arterial hypertension and may be putaminal, thalamic, lobar, cerebellar, or pontine. Cerebral amyloid angiopathy may cause lobar hemorrhage in the nonhypertensive elderly. CT is the primary method of evaluation. In younger, nonhypertensive patients, a cerebral or dural AVM may be the cause of hemorrhage, requiring further workup with MRI and cerebral angiography, which may
need to be repeated or delayed if there is a large and compressive hematoma. Contrastenhanced MRI and possibly MR spectroscopy may be useful if a tumor is suspected.
need to be repeated or delayed if there is a large and compressive hematoma. Contrastenhanced MRI and possibly MR spectroscopy may be useful if a tumor is suspected.
Severe unilateral headache with cervicalgia and/or a Horner syndrome may be caused by an acute carotid or vertebral arterial dissection. MRI/MRA, especially with precontrast fat-saturated axial T1 imaging, is diagnostic, showing the true lumen as a flow void and the mural thrombus as a bright crescent, so that there is generally no need for conventional angiography unless intracranial extension is suspected or endovascular treatment is contemplated. Migraines can cause severe acute headaches, usually periorbital, hemifacial, and frontal. The diagnosis is clinical, and CT may be sufficient to rule out hemorrhage in typical cases. Sinusitis is also diagnosed clinically; coronal CT shows soft tissue material obstructing sinus drainage pathways and filling the sinuses, and air-fluid levels in acute sinusitis. Glaucoma, retrobulbar optic neuritis, hydrocephalus, and infection may also cause acute headaches, evaluated with CT in clinically uncertain cases.
B. Subacute headaches.
Subacute headaches, particularly in the elderly, may be caused by a subdural hematoma. CT is usually adequate for both the initial evaluation and the follow-up, showing subdural space crescentic collections. Acute blood is hyperdense, whereas chronic collections are hypodense. CT is also the modality of choice to diagnose hydrocephalus (the temporal horns and the third ventricle are early reliable indicators of hydrocephalus). Cerebral tumors and infections may be evaluated with postcontrast CT (although contrast-enhanced MRI is superior). Spontaneous intracra nial hypotension, possibly associated with a chronic CSF leak, is a potential cause for headaches causing recurrent ER visits; postcontrast MRI (particularly in the coronal plane) may be diagnostic, showing thickened and densely enhancing meninges as well as “sagging of the midbrain” and decreased volume in the suprasellar and basilar cisterns.
C. Chronic headaches.
Unruptured AVMs, temporal arteritis, vasculitides, colloid cysts of the third ventricle, and cervical spondylosis are all potential causes of chronic head aches, in addition to migraine, cluster headaches, and chronic sinusitis. MRI has the highest yield in screening patients with a suspected structural intracranial anomaly.
III. CEREBRAL ISCHEMIA
Cerebral ischemia may be the result of acute arterial occlusion, hypoxic or anoxic injury, or may result from venous occlusion with increased venous pressure. Arterial occlusion may be an acute event, a chronically progressive process or an acute process superimposed on chronic.
A. Acute stroke.
It is a true emergency (time is brain). There is a 4.5-hour window after the ischemic stroke onset for the delivery of intravenous tissue plasminogen activator. Past that, and up to 6 hours in the carotid circulation (possibly longer in the vertebro basilar circulation), intra-arterial thrombolysis may be an option. One proposed algo rithm for the emergency evaluation of acute stroke is to obtain a plain CT, followed (if no hemorrhage) by a contrast CTA and CT perfusion study to evaluate the perfusion deficit. In some centers, MRI, MRA, and MR perfusion are utilized in acute stroke patients. DWI is positive for acute stokes as early as 30 minutes and up to 10 days after the onset and is therefore particularly well-suited to differentiate acute and subacute from chronic events (Fig. 32.3A and B).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree