Neurologic and Functional Evaluation
Seth M. Zeidman
Edward C. Benzel
Virgilio Matheus
Appropriate neurologic assessment is critical for the evaluation and treatment of cervical disk herniation and degenerative diseases of the cervical spine. In discussing cervical intervertebral disk lesions and degeneration, precise terminology and definitions are essential. The clinical spectrum of symptomatology for cervical disk disease can be divided into four broad categories: (a) cervical degenerative discogenic (internal disk disruption), (b) cervical radiculopathy, (c) cervical myeloradiculopathy, and (d) cervical myelopathy. Defining where patients fall along this continuum is a necessary prerequisite to providing optimal management.
DEGENERATIVE DISK DISEASE
Cervical disk disease results from disk degeneration, that is, mechanical breakdown of disk integrity. It may be more appropriately considered an aging process, rather than a disease. As such, cervical disk degeneration most commonly results from aging and dehydration, but the condition is affected by lifestyle, genetics, smoking, nutrition, and physical activity. Radiographic degenerative changes may reflect simple aging and do not necessarily indicate a symptomatic or even a pathologic process. Cervical disk degeneration includes degenerative annular tears, loss of disk height, and nuclear degradation. Disk degeneration often develops insidiously, without overt clinical manifestations. Initial symptoms may reflect mechanical instability and only later denote neural compression. The disk begins to degenerate in the second decade of life. Circumferential tears form in the dorsolateral annulus after repetitive use. Several circumferential tears can coalesce into radial tears, which progress into radial fissures. The disk then disrupts with tears passing throughout the disk. Loss of disk height occurs with subsequent peripheral annular bulging. Proteoglycans and water escape through fissures formed from nuclear degradation, resulting in further thinning of the disk space. Vertebral sclerosis and osteophytic formation ultimately result.
With aging, the intervertebral disks desiccate, resulting in disk height loss. Disk degeneration causes instability, resulting in irregular vertebral movement. This puts greater stress on the articular cartilage of the vertebrae and their respective end plates. Osteophytic spurs develop at the margins of these end plates. Cervical instability produces dorsal joint strain with consequent axial and referred pain from injured and stressed ligaments and damaged facet joints. Intervertebral disk height collapse forces bony prominences and the uncovertebral joints of adjacent vertebral bodies to approach and ultimately oppose one another, with resultant reactive hyperostosis and osteophyte formation. Osteophytes stabilize adjacent vertebrae whose hypermobility is caused by the degeneration of the disk. Osteophytes increase the articulation surface area, allowing a more equal distribution of compressive forces.
Osteophytes develop along the dorsal portion of the vertebrae in association with uncovertebral joint and facet osteoarthritis, which may produce zygapophyseal joint hypertrophy, decreased anteroposterior (AP) diameter of the vertebral canal, and neural foraminal encroachment.
Osteophytic compression of the intervertebral foramina can occur from either the uncovertebral or the zygapophyseal joint hypertrophy. Compression of the nerve root initially affects the larger, more pressure-sensitive A fibers, resulting in the characteristic radiculopathic syndromes of weakness, numbness, and reflex loss. Uncovertebral and facet hypertrophy can cause epidural adhesions and perineural inflammation. The combination of root compression and inflammation produces pain in a radicular distribution, that is, radiculopathy.
Osteophytic compression of the intervertebral foramina can occur from either the uncovertebral or the zygapophyseal joint hypertrophy. Compression of the nerve root initially affects the larger, more pressure-sensitive A fibers, resulting in the characteristic radiculopathic syndromes of weakness, numbness, and reflex loss. Uncovertebral and facet hypertrophy can cause epidural adhesions and perineural inflammation. The combination of root compression and inflammation produces pain in a radicular distribution, that is, radiculopathy.
CERVICAL INTERNAL DISK DISRUPTION AND DISCOGENIC PAIN
Cervical discogenic and internal disk disruption is a subjective disorder without objective neurologic deficits or testable abnormalities. Internal disk disruption was initially popularized by Crock, who described disk lesions characterized by alteration in internal structure and metabolic functions not associated with rupture or other definable pathoanatomy. A biochemical basis for deficiency was postulated, a hypothesis subsequently based on certain inflammatory-type pathologic features as shown by microscopy, in addition to intraoperative observations suggestive of peridiscal inflammation. Crock cited the often-observed element of increased peridiscal vascularity with sympathetic trunk matting and softening of the vertebral bodies. Clinical features of internal disk disruption are variable; however, Crock pointed out certain universal features that serve to differentiate the condition from others, such as rupture. A constant symptom described as a deep-seated, dull, aching neck pain was invariable. Shoulder girdle or limb pain was typically described as nondermatomal and generalized, in contrast to the more discrete pain characteristic of nerve root compression. A significant association with headache and constitutional symptoms has been noted.
The cardinal lesion rendering a cervical disk painful is internal disk disruption. The characteristic feature of internal disk disruption is a radial fissure extending to the innervated outer third of the annulus fibrosus. As radial fissures extend to the outer third of the annulus, nerve endings are exposed to the inflammatory and algogenic chemicals produced by nuclear degradation. As a radial fissure develops, fewer and fewer lamellae remain intact to bear the load. At some stage, the threshold for mechanical nociception is attained, especially if the nerve endings have been chemically sensitized. Disk stimulation reveals this condition by showing a reduced threshold for mechanical stimulation of the disk.
CERVICAL RADICULOPATHY
Classic syndromes of cervical root compression are well defined (Table 10.1). Many tests and signs have been described to complement the physical examination and to define more clearly the nature of a patient’s neck and arm pain and its relationship to compression of either nerve roots or the spinal cord. The onset of symptoms with radiculopathy may be insidious, or patients may ascribe their symptoms to some inciting event. Acute trauma can trigger radicular symptoms. Patients with abrupt onset of radicular complaints still may have a soft disk rupture superimposed on cervical degenerative disease. Radiculopathy is the most common symptom that results in cervical disk surgery.
TABLE 10.1 Classic Nerve Root Involvement: Radiculopathy | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
In patients with cervical radiculopathy, the arm pain greatly exceeds mechanical problems in the neck (Fig. 10.1). Radiculopathy is defined as pain and associated neurologic deficits in a nerve root distribution. This results from compression of cervical nerve roots by herniated disk material or degenerative disk disease at or near the vertebral foramen. Discomfort and numbness in a root distribution are often the only symptoms. The pain is related to neck position and worsened by rotation, lateral flexion, or extension of the head. Patients may be roused from sound sleep by severe neck pain. Moving or extending the neck reproduces the arm pain.
 Figure 10.1. Radiculopathy resulting from disk herniation. MRI demonstrated lateral disk herniation in a patient who presented with unilateral radiculopathy. |
The term radiculopathy implies consistently reproducible neurologic findings: motor loss, sensory abnormalities, and reflex changes. Radicular symptoms are characterized by proximal pain and distal paresthesias in the distribution of the affected nerve root. In general, symptoms are referable to an individual nerve root. There may be overlap between dermatomes innervated by a particular nerve, and only rarely are findings isolated to a single dermatome. Likewise, because there is overlap of the innervation to the muscles and reflexes in the upper extremities, clinical localization is not exact.
Isolated numbness may develop, with minimal pain or without pain. Patients occasionally present with a motor deficit without sensory pain or numbness. Usually, the deficit affects a single nerve root and evolves so slowly that the patient is able to compensate with other muscle groups. Only simultaneous symmetric assessment of arm and hand musculature will detect the motor loss. Arm abduction sometimes brings relief to patients with a ruptured cervical disk. Patients occasionally present with an arm draped over the head. Relief is uncommon in patients with spondylosis.
The neck compression test reproduces radicular symptoms with lateral flexion, rotation, and vertical compression of the patient’s head. The Spurling sign results in cervical root compression and pain with hyperextension and contralateral rotation of the neck. This has been reported to be present in 25% to 50% of patients with radiculopathy. The Valsalva test creates radicular symptoms with intentional increases in intra-abdominal pressure. Radicular symptoms may be improved by 10 to 15 pounds of axial traction or by elevation of the patient’s hand over the head while the patient is sitting.
Two-thirds of patients with acute radiculopathies remain persistently symptomatic, and only one-third obtain long-term relief with medical and physical therapy. In contrast to acute radiculopathy, chronic radiculopathy is generally unaffected by either neck position or motion. The principal manifestation of chronic progressive radiculopathy is atrophy. Older patients with unilateral or bilateral multilevel involvement and atrophic changes often have symptoms that simulate those of other neurologic disease. More chronic radiculopathies with spondylotic disease affecting two or more adjacent levels sometimes involve more than one nerve root. Determination of the levels warranting operative intervention requires careful neurologic examination of the patient.
CERVICAL MYELORADICULOPATHY
Myeloradiculopathy is defined as a radiculopathy with myelopathic findings. Myelopathic findings are more common than root symptoms. Motor and reflex changes are observed more often than sensory changes, and analgesia is more common than anesthesia. Motor findings are generally paretic at the lesion level and spastic below that level. Arm findings can be unilateral, but leg findings are typically bilateral. Sensory disturbances can be variable and are typically below the area of compression. Touch is usually preserved, with decreased pain and temperature sensation. Reflex changes typically follow the pattern of motor involvement.
Cervical myeloradiculopathy represents a well-known syndrome in which patients manifest a variety of symptoms. The most common presentation is subtle neck pain in conjunction with radicular complaints. On initial examination, patients exhibit signs of radiculitis and radiculopathy. However, the reflexes in the lower extremities are hyperactive. Careful questioning of the patient elicits their decreased ability to run or to button their clothing. During the initial evaluation, such patients should be asked to run in place in the examination room or to stand on one leg with eyes closed. These maneuvers provoke the subtle signs of myelopathy. The pathologic substrate of myeloradiculopathy is compression of both the spinal cord and nerve root.
It is now known from trauma experiments that as much as 30% of the spinal cord volume can be lost without affecting the neurologic examination. Patients with broadbased disk herniations, typical radiculopathy, and normal neurologic findings in the lower extremities who report improvement in their ability to run and walk after successful ventral decompression have been observed. Hindsight shows that some patients are treated for radiculopathy when they actually also had a subtle myelopathy that was not diagnosed preoperatively.
CERVICAL SPONDYLOTIC MYELOPATHY
Cervical spondylotic myelopathy (CSM) is a neurologic disorder manifested in its most severe form by spastic gait, clumsy hands with atrophy and sensory impairment, sphincter disturbances, and pain related to the underlying spondylosis of the cervical spine. CSM is a graded process with myriad clinical manifestations. Compressive, ischemic, and dynamic factors all contribute to the pathophysiology. CSM is typically a slowly progressive disorder that ultimately produces significant disability and results from a combination of factors.
ETIOLOGY
Although the clinical manifestations of myelopathy due to spinal cord tumors, abscesses, trauma, and other conditions are similar, our discussion is confined to disorders associated with cervical spondylosis. The common initiating pathology in the production of CSM is spinal cord compression (Fig. 10.2). Chronic or (subacute) myelopathy secondary to cervical spondylosis is a common entity. Myelopathy due to cervical spondylosis was initially recognized in the 1950s.
Degenerative changes, such as a dorsal protruding disk, ossification of the posterior longitudinal ligament (OPLL), vertebral osteophytes, facet joint spurs, overriding joint of Luschka, invagination or ossification of the ligamentum flavum, and trauma, can contribute to spinal stenosis, which leads to spinal cord compression (Fig. 10.3). The sequelae of spinal cord compression result from the interaction of three synergistic factors: canal narrowing secondary to degenerative disk disease and congenital cervical stenosis, compromise of cord circulation, and repetitive motion and intermittent mechanical compression of the spinal cord.
Compression may be secondary to disk herniation, degenerative osteophyte production, OPLL, or congenital
spinal stenosis with minor degenerative changes. Chronic disk degeneration with osteophyte formation is the most common cause of myelopathy in older patients. Spondylotic myelopathy is the most common cervical cord disorder during and after middle age. Within the cervical cord, there is a gradation of sensitivity to direct compression of the cord, with the most sensitive area being the corticospinal tract, followed by anterior horn cells, anterior funiculus, and posterior funiculus.
spinal stenosis with minor degenerative changes. Chronic disk degeneration with osteophyte formation is the most common cause of myelopathy in older patients. Spondylotic myelopathy is the most common cervical cord disorder during and after middle age. Within the cervical cord, there is a gradation of sensitivity to direct compression of the cord, with the most sensitive area being the corticospinal tract, followed by anterior horn cells, anterior funiculus, and posterior funiculus.
 Figure 10.2. MRI showing intrinsic spinal cord hyperdensity supradjacent to disk herniation in a patient with acute myelopathy. |
The normal spinal canal has a diameter of 17 to 18 mm between C3 and C7. The normal spinal cord AP diameter is about 9 mm. There should be a minimum of 1 mm of cerebrospinal fluid (CSF) on each side of the cord and 1 mL of dura. These additional 4 mm, in addition to the 9 mm of cord, demand a space of 13 mm. Therefore, an AP cervical vertebral canal diameter of 13 mm or less results in spinal cord impingement.
The two major components are (a) compressive forces from spinal canal narrowing and (b) dynamic forces due to cervical spine motion. Although trivial trauma may prompt recognition of the neurologic deficit, myelopathy is nearly always a progressive process. Repetitive trauma to the spinal cord sustained with movement in a spondylotic canal may be a major cause of progressive myelopathy.
Spinal cord compression may be confined to a single level secondary to disk herniation or to a sizable osteophyte, or it can extend over several segments (Fig. 10.4). When it is multilevel, it is often caused by multilevel degenerative changes or OPLL (Fig. 10.3). Occasionally, diffuse compression occurs over many segments in a patient
with a congenitally narrowed canal and mild age-related spondylosis, and the cord has insufficient space.
with a congenitally narrowed canal and mild age-related spondylosis, and the cord has insufficient space.
 Figure 10.3. MRI in a patient with severe spondylotic disease and myelopathy resulting from stenosis. |
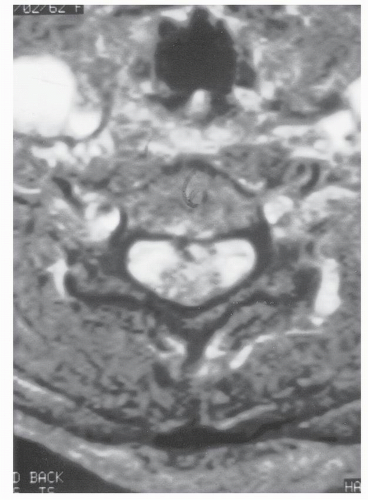 Figure 10.4. Soft disk herniation of central disk. Axial MRI of patient with acute development of cervical myelopathy with numb and clumsy hands and lower extremity clonus. |
Pressure on the spinal cord results in vascular compromise, with resultant ischemia. Cervical spinal cord blood flow is dependent on the integrity of both the anterior and posterior spinal arteries, in addition to the radicular supply from the vertebral arteries. The position of the anterior spinal artery is variable and may extend well ventral to the spinal cord. Ventral compressive pathology, including spondylotic ridging and disk compression, may hinder arterial flow, producing focal ischemia. Ischemia can also be secondary to local compression of intramedullary branches. This is more prominent in the gray matter because vascular demands of the gray matter are four to five times that of the white matter, and it is therefore more sensitive to ischemia. Gray matter ischemia accounts for the lower motor neuron phenomena observed in many patients. The etiology of the progressive pathology dictates the therapeutic response. If there is marked ventral compression, this pressure may be directly on the anterior spinal artery, accelerating the course of pathologic events. More commonly, the microcirculation of the cord in the area of compression is damaged.
Although the compressive pathophysiology exceeds the vascular changes, in the more advanced stages, it is a combination of both pathologic entities that ultimately leads to spinal cord damage. Development of significant myelopathy secondary to cord compression has three components: degree of cord compression, rate of compression, and constancy or intermittence of the compressive force. Acute CSM can develop in the presence of spondylosis and can occur without an identifiable inciting event. Acute myelopathy can arise in the setting of extreme hyperextension, acute disk herniation with spinal cord compression and torticollis, or other involuntary movement disorders. Patients with torticollis, torsion dystonia, and other involuntary movement disorders aggravate the normal cervical spine trauma and may induce premature cervical spondylosis with resultant myelopathy.
The cervical spine normally has a lordotic curvature. Degenerative disk disease results in loss of intervertebral disk height, with obliteration of cervical lordosis and a straightened or even kyphotic spine. Kyphosis may be a cause of cord compression as well. In the presence of underlying spinal cord compression, the natural movements of the cervical spine produce increased pressure on the cord. Extension of the neck causes ligamentum flavum prolapse and buckling, exacerbating preexisting ventral pathology, and can initiate painless loss of neurologic function caudal to the area of compression. Therapy should address this compression and relieve cord impingement. There is no medical therapy to relieve or correct spinal cord impingement. Cervical spine immobilization and nonsteroidal anti-inflammatory drugs (NSAIDs) may reduce the incidence of microtrauma, which can contribute to progression. When one considers that patients live for years after the initial symptoms appear, spinal cord decompression is mandated.
Recent studies have convincingly demonstrated that apoptosis also plays a pivotal role in numerous pathologic processes, contributing to the adverse effects of various diseases and traumatic conditions. A growing body of evidence has implicated apoptosis as a key determinant of the extent of neurologic damage and dysfunction after acute spinal cord injury and in chronic cervical myelopathy. There is now strong evidence to support a significant role for apoptosis in secondary injury mechanisms after acute spinal cord injury as well in the progressive neurologic deficits observed in such conditions as spondylotic cervical myelopathy (1,2).
SIGNS AND SYMPTOMS
The classic presentation of myelopathy is numbness and clumsiness of the hands in association with a stiff, spastic unsteady gait. Patients with CSM generally report neck stiffness; unilateral or bilateral deep, aching neck, arm, and shoulder pain; and possibly stiffness or clumsiness while walking. Patients sometimes report greater difficulty walking at night, owing to reduced proprioceptive input.
CSM usually develops insidiously and with a stepwise “stuttering” progression. In the early stages of CSM, complaints of neck stiffness are common because of the presence of advanced cervical spondylosis. Other common complaints include crepitus in the neck with movement; brachialgia, which is characterized as a stabbing pain in the preaxial or postaxial border of the arm, elbow, wrist, or fingers; a dull, achy feeling in the arm; and numbness or tingling in the hands. Symptoms may be asymmetric, particularly in the legs. Loss of sphincter control or frank incontinence is rare; however, some patients may complain of slight hesitancy on urination.
The clumsiness experienced in the hands reflects the neuroanatomy of the efferent innervation of the hand musculature. The corticospinal tracts and extrapyramidal system travel down the posterolateral funiculus of the spinal cord to synapse with internuncial neurons two to three segments above the primary motor neuron. For example, intrinsic muscles of the hand are driven by motor fibers descending down the corticospinal tract to end and synapse with internuncial neurons as high as C5 and C6. Here, there is an internuncial neuronal pool with a variety of both inhibitory and facilitatory influences from the local afferent input. The internuncial neuronal pool then feeds down the cord to the anterior horn cells at the C8 cord level. Here, the anterior horn cell output is modulated and emerges as the final output from C8 and T1 and goes to the hand. If the internuncial neuronal pool is disrupted, normal coordination and smoothness of hand function is disrupted, and clumsiness appears. With disruption of the neuronal pool higher in the spinal cord, the hand can appear as if it has a lower motor neuron disease. Within the cervical enlargement with its corresponding large quantity of gray matter in the cervical cord, disruption of the internuncial neurons can lead to the classic symptoms of numbness and clumsiness, which are difficult to fit with a single radicular pattern. This is an important part of the myelopathy and is termed myelopathy hand. OPLL as high as C2 can present with this clinical finding. Loss of hand dexterity, with painful dysesthesias and difficulty in writing, is common. The syndrome of myelopathy hand may be the most important indicator of a good response to surgery.
In patients with myelopathy, the cord signs and symptoms generally outweigh the focal radicular disorder, and motor loss exceeds sensory loss. Lower motor involvement occurs at the level of the lesion, with atrophy of upper extremity muscles, especially hand intrinsics. Upper motor neuron findings are noted below the level of the lesion, with lower extremity spasticity and hyperreflexia. The sensory fibers are polysynaptic, and the posterior columns remain intact because the circulation is well collateralized, enters dorsally, and is therefore minimally affected. Focal sensory loss is less readily appreciated. Many patients have a subtle loss of sharpness to pinprick on the lower half of the body, with a sensory gradient across the trunk to normal sensation. Analgesia is more common than anesthesia, which is more common than proprioceptive loss. Reflex changes may be present, with relative hyperreflexia in the legs as compared with the arms. Bilateral Hoffman and Babinski signs are commonly present.
Lhermitte sign is the axial shock-like sensation elicited by neck flexion, extension, or axial compression. It is classically produced by pressing down on the top of the head. Lhermitte sign is present in as many as 25% of myelopathic patients. Babinski and Hoffman signs are nonspecific findings with upper motor neuron lesions and can be demonstrated in patients with myelopathy secondary to cervical disk disease. Determination of the range of motion of the cervical spine should be performed actively, passively, and against resistance.
Acute myelopathy can occur spontaneously or after minor or major trauma. The common presentation is a central spinal cord syndrome with pain. The neurologic loss is that of lower motor abnormalities in arms and hands with hyperreflexia and with spasticity in the legs. Acute myelopathy after minor trauma can occur without fracture or dislocation. It is often associated with spondylosis or congenital stenosis. Static cord impingement often cannot be demonstrated radiographically. Acute myelopathy also occurs in young people with congenital spinal stenosis or multiple sports traumas. Such patients may develop diffuse cervical spinal stenosis as a result of multiple minor spinal injuries. Patients with congenital or acquired stenosis and an AP diameter of less than 10 mm are vulnerable to acute spinal cord injury when the spine is sufficiently hyperextended. Such patients typically are football players who present after some trivial trauma with what has been described as neurapraxia, stinger, or spinal cord concussion. Cervical spondylosis produces canal narrowing, and hyperextension precipitates acute compression and injury. Dynamic compression of the spinal cord results in neurologic injury, often a central cord syndrome.
The anterior spinal artery syndrome has a variety of causes. Acute quadriparesis and dissociation of sensory loss with preservation of posterior column functions are its hallmarks. Acute soft disk herniation with cord compression can present with myelopathy and requires urgent surgical intervention. This should be suspected in patients whose plain radiographs demonstrate congenital or spontaneous fusion and in patients with previous cervical injury.
Few studies of the natural history of spondylotic myelopathy have been performed, and those that have were small, with dissimilar disability grading systems and with outcomes that are not comparable. Despite these limitations, some information can be gleaned from the available literature. Myelopathy secondary to spondylosis typically has an insidious onset, developing over a prolonged period. The natural history is characterized by long intervals of clinical stability punctuated by short periods of worsening and ultimately intermittent progression. Myelopathy may initially appear as an isolated condition, in conjunction with a severe radiculopathy or as a significant component of myeloradiculopathy. Patients may have very minor degenerative changes and become symptomatic. Their neurologic deficits can be dramatic and anxiety producing, causing patients to present for evaluation. Once myelopathy occurs, complete reversal is rare. Patients with myelopathy often go for long periods of time without development of new or worsening signs and symptoms.
Spondylotic myelopathy may present as a stepwise deterioration (75%), as a relentless downhill slide without plateaus or remissions (20%), or as a downhill course with occasional remissions (5%). In few patients, the myelopathy will reverse with conservative care or no care. Significant reduction in neurologic deficits is unusual. After conservative treatment, most myelopathic patients experience periods of stable disability punctuated by episodes of progressive deterioration. Reported improvements may represent a plateau with lack of progression or with the patients growing accustomed to their disability. After onset of clinical myelopathy, rarely do patients regain neurologic normality, and spontaneous remission of symptoms is unlikely.
Nurick (3) postulated that the degree of disability in cervical myelopathy was established early in the disease process and rarely progressed. In a clinical review of 1,355 patients with CSM, Epstein reported that conservative therapy resulted in 36% improvement and 64% nonimprovement. In the group with nonimprovement, 26% of patients significantly deteriorated neurologically.
A subset of patients presents with relentless progression that proceeds to severe disability. Our clinical experience is most similar to that of Symon and Lavender, who reported that more than two-thirds of the patients with myelopathy whom they studied displayed relentless deterioration of neurologic function rather than a series of plateaus and downhill progression. Patients presenting with markedly myelopathic findings in association with drastically reduced spinal canal dimensions over several levels can expect progressive deterioration.
Real improvement in patients with myelopathy can be expected after operative cord decompression if symptoms have been present for less than 2 years. When the duration of symptoms exceeds 2 years, demonstrable significant improvement in patients is rare. Age at presentation and duration of disease before treatment are the most important factors affecting prognosis. Increased age is associated with poorer outcome. Age and clinical severity are less important factors than duration of disease and the operation performed. Myelopathy is a treatable condition, and prompt diagnosis improves the likelihood of favorable outcome.
Attempts at grading myelopathy have focused on the effects on patient performance. Patient grading is essential to evaluate the results of various available therapies. A standardized grading system for myelopathy would allow
more complete understanding of the natural history of this disorder as well as provide a valid means of comparing the results of the different treatment modalities. Identification of more serious neurologic problems, the rapidity of their progress, and their response to therapy would then dictate the urgency for treatment. Double-blinded, prospective, randomized trials of both ventral and dorsal procedures as well as conservative therapy are the best methods for determining the efficacy of the various therapies available today.
more complete understanding of the natural history of this disorder as well as provide a valid means of comparing the results of the different treatment modalities. Identification of more serious neurologic problems, the rapidity of their progress, and their response to therapy would then dictate the urgency for treatment. Double-blinded, prospective, randomized trials of both ventral and dorsal procedures as well as conservative therapy are the best methods for determining the efficacy of the various therapies available today.
TABLE 10.2 Classification System for Myelopathic Gait Abnormalities | |||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







