and antedates all of the more complex systems. A complete injury had the following: complete loss of voluntary motor function below the level of the injury, complete absence of somatic sensation below the level of the injury, and complete loss of voluntary control of bowel and bladder function. Later, other features were added to the definition of the complete syndrome such as the presence of abnormal reflexes including priapism and the early return of the bulbocavernosus reflex. In contrast, a patient was neurologically incomplete when there was any residual voluntary motor or sphincter function or sensation below the level of the injury. As shown in Table 14.1, a large number of incomplete syndromes have been described, generally based on the anatomical location of the maximal cord injury in the transverse plane.
TABLE 14.1 Simple Systems for Neurologic Classification of Acute Cervical SCI: Complete and Incomplete Neurologic Syndromes | ||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||
TABLE 14.2 Complex Systems for Neurologic Classification and Scoring in Acute Cervical SCI | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
presumed location of the maximal injury in the transverse plane of the spinal cord (15) (Figs. 14.1, 14.2, 14.3, 14.4 and 14.5). It is useful clinically to categorize incomplete patients on the basis of the anatomical location of the cord injury because it provides information about the mechanism of injury and influences selection of treatment. These incomplete syndromes have differing prognoses for recovery, and therefore, categorization provides prognostic information.
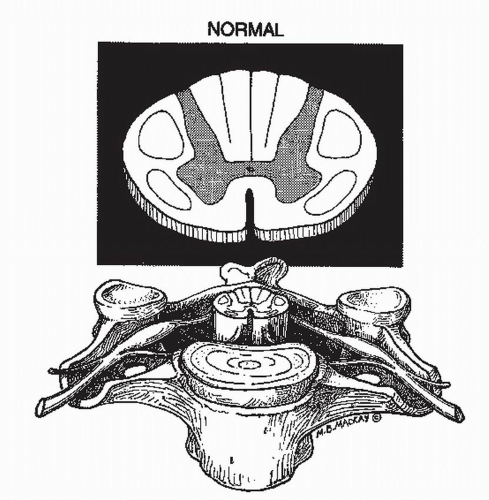 Figure 14.1. The normal spinal cord and spinal column. The normal relationships between the spinal cord, spinal column, and nerve roots are depicted in the mid cervical region. For clarity the durra has been omitted. In the upper diagram, the gray matter is finely stippled, and the corticospinal and spinothalamic tracts are outlined. The intervertebral disk is shown. Reprinted with permission from Narayan et al. Neurotrauma. New York: McGraw-Hill, 1996, Chapter 75. |
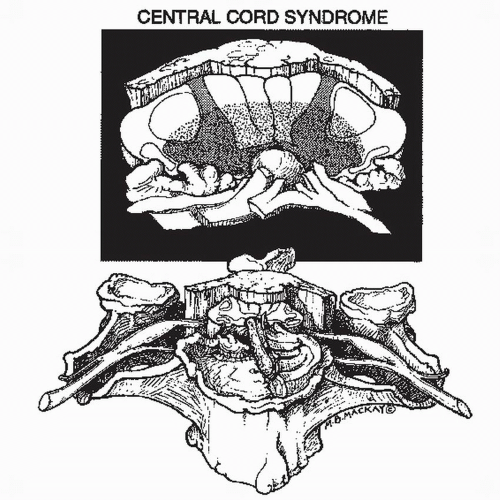 Figure 14.2. Central cord syndrome. The drawing depicts a case of cervical spondylosis with osteoarthritis of the cervical spine including anterior and posterior osteophytes and hypertrophy of the ligamentum flavum. Superimposed is an acute hyperextension injury, which has caused rupture of the intervertebral disk and infolding of the ligamentum flavum. The spinal cord is compressed anteriorly and posteriorly. The central portion of the cord shown in rough stippling sustained the greatest damage. The damaged area includes the medial segments of the corticospinal tracts presumed to subserve arm function. Reprinted with permission from Narayan et al. Neurotrauma. New York: McGraw-Hill, 1996, Chapter 75. |
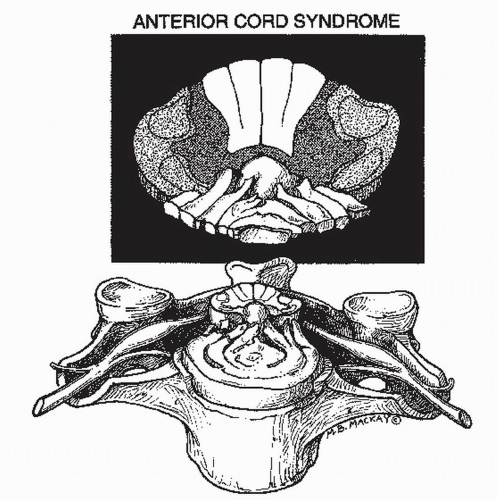 Figure 14.3. Anterior cord syndrome. A large disk herniation is shown compressing the anterior aspect of the cord and resulting in damage (rough stippling) to the anterior and lateral white matter tracts and to the gray matter. The posterior columns remain intact. Reprinted with permission from Narayan et al. Neurotrauma. New York: McGraw-Hill, 1996, Chapter 75. |
definition, the negative radiologic examination includes only plane films and tomography, either conventional or CT. If a negative MR was included in the definition, the number of cases would diminish dramatically because of the extreme sensitivity of MR for detecting even mild cord injury such as T2 signal change and spinal column injury such as torn ligaments and ruptured disks. True SCIWORA can also occur in adults but is much less frequent than the syndrome of acute SCI without radiologic evidence of trauma (SCIWORET) (28). Cervical spondylosis is the most commonly associated condition in adults with SCIWORET, but other conditions including spinal stenosis, ankylosing spondylitis, disk herniation, and nucleus pulposus embolism may on rare occasion be associated with SCI and not show radiologic evidence of trauma (28). Thus, in SCIWORET, there are often abnormal radiologic exams, but no evidence of trauma. Prior to the use of CT or MRI in spinal trauma, the incidence of SCIWORET in SCI in adults was approximately 14% (15). The addition of CT has reduced the incidence of SCIWORET to about 5%. One study showed that many patients with SCIWORET have demonstrable compression by myelography or MRI and should be considered for early surgical decompression (29). It is likely that very few SCIs will remain undetected by MR because of its high sensitivity for detecting mild SCI and nonbony spinal column lesions.
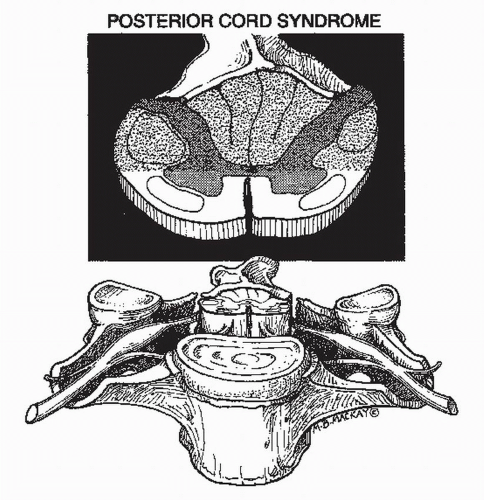 Figure 14.4. Posterior cord syndrome. A laminar fracture is depicted with anterior displacement of the fractured bone and compression of the posterior aspect of the spinal cord. The damaged area of the cord (roughly stippled in the upper diagram) includes the posterior columns and the posterior half of the lateral columns including the corticospinal tracts. Reprinted with permission from Narayan et al. Neurotrauma. New York: McGraw-Hill, 1996, Chapter 75. |
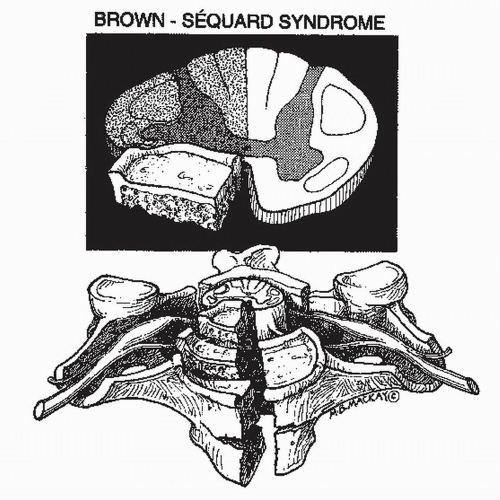 Figure 14.5. Brown-Séquard syndrome. A burst fracture is depicted with posterior displacement of bone fragments and disk, resulting in unilateral compression and damage (rough stippling) to one-half of the spinal cord. Reprinted with permission from Narayan et al. Neurotrauma. New York: McGraw-Hill, 1996, Chapter 75.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|





