Neurologic Examination of the Newborn, Infant, and Child
The ability to perform a thorough neurologic examination and to interpret the findings often obviates the need to perform imaging studies. Our purpose in this chapter is to facilitate understanding of the neurologic examination of children. For purposes of organization, the chapter is organized by age: examination of the newborn (0 to 4 weeks), the infant (1 to 24 months), and the older child (older than 2 years).
3.1 Components of the Neurologic Examination
3.1.1 Screening Methods
Interpretation of the neurologic examination findings depends on a thorough knowledge of normal childhood development. Examination of the term and preterm infant primarily reflects brainstem function and spinal cord reflexes, whereas examination of the older child approximates that of an adult. Maturation of the central nervous system (CNS) proceeds in a rostral to caudal fashion. For instance, head control develops first, with only a slight head lag on pull-to-sit at 4 months of age. The infant is able to sit supported at 6 months and then is able to pull to stand at 9 months. A video review of the neurodevelopmental milestones and the accompanying examination is available online at http://library.med.utah.edu/pedineurologicexam/html/home_exam.html.1
Screening methods have been developed to assist the clinician in identifying those patients with developmental delays. The clinician has several screening tools at his or her disposal to screen for developmental delay. Each may identify different populations of children with developmental delay because each is characterized by different standardizations, comparison groups used for sensitivity and specificity, and population risk status.2 For the purposes of a neurosurgical visit, broad general screening tools that address the main domains of fine and gross motor skills, language, adaptive behavior, and social skills are probably the best to use. There are two types of tools: directly administered scales, such as the Bayley Infant Neurodevelopmental Screen and the Denver-II (Glascoe), and questionnaires given to the family to complete, such as the Ages and Stages Questionnaires.3–5 The advantages of using these screening tests are that norms are stated explicitly and that normal development within each category is reassuring. However, as they reflect a snapshot in time of a child’s development, they may not identify children with mild delays. Parent-based questionnaires may be better screens for mild developmental delay. Several studies have shown that parental reporting of current skills is predictive of developmental delay.4–6 The advantage of screens that rely on parental information is that they do not rely as heavily on the examination of a child who may be sick, afraid, drowsy, or noncompliant at the time of the visit.
In the school-age years, specific underlying abnormalities, such as learning disabilities, may become manifest as school performance demands cognitive levels not assessed by screening tests. Cognitive development can be assessed, albeit imperfectly, by IQ testing, which can be a predictor of attention, social skills, maturational level, and intelligence. The Wechsler Intelligence Scale of Children-III, which tests verbal, performance, and full IQ, is the most commonly used measure of a child’s intelligence. It is used for children ages 6 to 16 years, but some tasks may be difficult for children 6 to 7 years of age. Detailed neuropsychological testing may be necessary to evaluate cognitive function further.
Examiners should be cautioned, however, that a “normal screen” does not preclude subtle developmental abnormalities, as these screens focus narrowly on discrete milestones and do not assess fine detail within those parameters. In addition, a developmental screen assesses the patient’s current developmental level and is not a predictor of future achievements or maximal potential. The real value of screening is to follow developmental milestones and to assess if a particular neurologic symptom is static or progressive over time.
3.1.2 History
In a neurologic examination, the examiner begins by taking the patient’s history, which includes an outline of the evolution of the illness, its character, and the presence of similar illness in family members. The examiner attempts to establish neurologic disorders as progressive, intermittent, static, or saltatory. Static abnormalities noted in the first few months of life suggest congenital abnormalities or brain injuries sustained during the perinatal period. Progressive disorders suggest degenerative CNS disease, whereas abnormalities that are intermittent and alternate with return to normal neurologic function indicate paroxysmal disorders, primarily seizures. Saltatory disorders, characterized by exacerbation and partial recovery, are seen particularly with demyelinating and vascular diseases and with mitochondrial disorders.
Medical History
The medical history in the evaluation of children begins with the birth history. A complete pregnancy history is essential and should include the mother’s age, number of pregnancies, number of deliveries, prenatal care, and number of induced and spontaneous abortions. The pregnancy history should be obtained with the intent of determining parameters that may present risks to the fetus, such as history of exposure to illness, maternal rash, maternal bleeding, maternal drug or alcohol use, and abnormal fetal growth. The history of labor and delivery is often a clue to the timing of a CNS injury. The examiner should note the type of anesthetic, if any, used for delivery of the child; duration of the rupture of membranes; whether or not there was meconium staining; fetal heart rate patterns if available; and finally, the child’s Apgar scores. Gestational age should be noted, as this knowledge may impact interpretation of the newborn’s neurologic examination.
Social History
The social history can provide clues to a neurologic diagnosis, such as exposures to toxins or medications. School reports may highlight specific cognitive difficulties that a child may have. The adverse effect of environmental risk factors, such as single parenthood, less than a high school education for one parent, limited parental contact, parental mental health concerns, and parental predilection for substance abuse, may be evident in the child’s development.
Family History
Family history is important in many neurologic abnormalities. The presence of consanguinity, neurologic disorders, and systemic disease should be noted in family members. A family history of neonatal deaths is often a clue to metabolic disorders. A family history of seizures often points to the presence of one of the epilepsy syndromes. Neurocutaneous disorders are often inherited in an autosomal-dominant fashion, and family members should therefore be examined for neurocutaneous lesions, such as hypopigmentation and hyperpigmented macules, if a neurocutaneous disorder is suspected.
3.1.3 Physical Examination
CNS function depends upon normal function of all other body organs. Thus, abnormalities of other organ systems detected on examination are important. However, particular attention should be paid to abnormalities of hair, skin, teeth, and nails because they, like the brain, are of neuroectodermal origin and may reflect CNS lesions. For example, the pattern of hair growth reflects underlying brain development, so that the absence of a posterior hair whorl or the presence of multiple hair whorls suggests an abnormality in prenatal brain growth. Neurocutaneous abnormalities, such as café au lait spots, neurofibromas, and port wine stains, occur in several CNS disorders, such as tuberous sclerosis, neurofibromatosis, and Sturge-Weber syndrome, respectively. Therefore, the child’s entire skin surface should be examined during the physical examination. Weight, height, and head circumference should routinely be measured. At birth, head circumference is approximately 35 cm, with growth at a rate of 2 cm per month from 0 to 3 months and 1 cm per month from 3 to 6 months of age. Intrauterine insults and many genetic syndromes associated with below- or above-average size have been linked with developmental delay. Microcephaly and macrocephaly are red flags for developmental problems with underlying structural CNS pathology, especially in the context of genetic or acquired disorders. As long as the head circumference is within normal limits, the size of the anterior fontanel is of little concern. Conditions that may lead to a large anterior fontanel include hypothyroidism, trisomy syndromes, in utero malnutrition, hypophosphatemia, rickets, osteogenesis imperfecta, and hydrocephalus.
3.2 Neurologic Examination of the Neonate
The formal neurologic evaluation includes an assessment of mental status, cranial nerves, motor system, sensory system, cerebellar function, and reflexes.
3.2.1 Mental Status Evaluation
The mental status examination of the neonate is made by the observation of spontaneous eye opening; movements of the eyes, face and extremities; and response to stimulation. Although both normal-term and preterm infants spend a large proportion of time in sleep, activity during wakefulness and duration of sleep vary with age. For instance, awake and sleep states are difficult to distinguish in a preterm infant born before 28 weeks of gestation. After 32 weeks of gestation, there is an increase in the frequency and duration of alertness. The normal-term newborn is easily aroused to a state in which the eyes are open and blink at a strong light stimulus. The ability to visually fix and follow at or after 34 weeks is a reassuring finding. To assess if a baby is visually fixing, the examiner should look for arrest of other activity, such as sucking. An astute examiner can observe subtle changes in mental status; an irritable infant will appear agitated, spontaneously cry, or cry to minimal stimulation and will not be easily soothed. The lethargic infant will have delayed or poorly maintained responses to stimulation.
3.2.2 Cranial Nerve Examination
Cranial Nerve I
Olfaction cannot be reliably assessed at bedside in the neonate.
Cranial Nerve II
Vision may be tested with the infant’s blink response to a strong light stimulus. The blink response can be predictably elicited beyond 30 weeks of gestation. The ability of the infant to fix visually on a face and follow it is reassuring for the assessment of normal visual acuity. Visual fields are not reliably assessed in neonates. The pupillary response to light is predictably present beyond 29 weeks of gestation. Funduscopic examination may demonstrate the presence of congenital malformations involving the eye or retina. Placing a pacifier in the child’s mouth may aid in keeping the eyes open during the examination. A direct and consensual pupillary response should be present. An afferent pupillary defect can be detected even at this young age by swinging the light from eye to eye and noting pupillary dilation when the light is brought to bear on the involved optic nerve.
Cranial Nerves III, IV, and VI
By 34 weeks of gestation, an infant will be able to fix and follow an object with his or her eyes, particularly the mother’s face. Another maneuver to test extraocular movements is to stimulate the vestibulo-ocular reflexes by gently spinning the infant. The baby is held in front of and slightly above the examiner and spun to the right or left. There should be conjugate eye deviation in the direction in which the examiner spins the child. After cessation of spinning, post-rotational nystagmus in the opposite direction is noted for a brief period, after which the vestibular response is ablated by visual fixation. This technique allows the examiner to assess vestibular function, the presence of intact extraocular muscle function, and visual acuity with a single procedure. Of note, disconjugate gaze is common in normal newborn infants when they are not fixing on objects.
Cranial Nerve V
In neonates, the muscles of mastication can be assessed by watching the infant suck and swallow. The corneal reflex may be assessed at the end of the evaluation.
Cranial Nerve VII
Facial symmetry at rest and during sucking activity is used to assess facial nerve function. One should also note facial symmetry during crying. Congenital absence of the depressor anguli oris, a disorder that mimics facial nerve lesions, is noted only during smiling or crying (▶ Fig. 3.1a,b and ▶ Fig. 3.2).
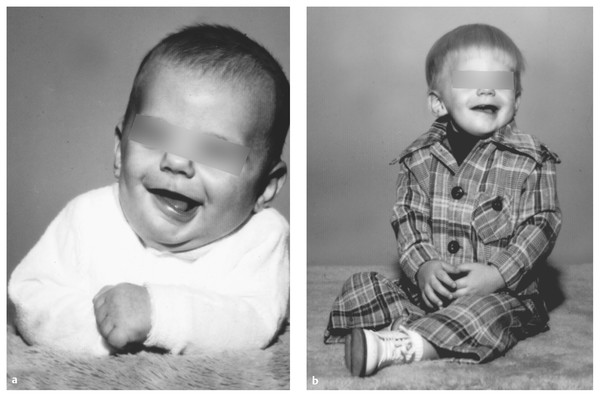
Fig. 3.1 (a) Congenital absence of the depressor anguli oris seen during smiling in early infancy. (b) Same patient as a toddler.

Fig. 3.2 Neonatal right peripheral facial paresis.
Cranial Nerve VIII
The vestibular portion of cranial nerve VIII can be assessed by spinning the infant as described in the examination of cranial nerves III, IV, and VI. Hearing can be grossly evaluated by the presence of a blink elicited by a sharp sound, such as a bell directed at either ear. Vestibular function mediated by the vestibulocochlear nerves is tested by caloric stimulation. The head is angled at 30 degrees, orienting the horizontal semicircular canals vertically, and the external canal is inspected for cerumen or defects of the tympanic membrane. Ten milliliters of ice water is then instilled into the ear, and the resulting eye movements are observed. In the conscious patient, coarse nystagmus develops toward the ipsilateral ear without eye deviation. In the comatose patient, the fast component is depressed, and the eye becomes tonically deviated ipsilaterally.
Cranial Nerves IX and X
The gag reflex can be reliably elicited beyond 30 weeks of gestation. The quality of the infant’s cry may be abnormal in many neurologic as well as genetic disorders.
Cranial Nerve XI
Sternocleidomastoid function and trapezius function are best assessed in the neonate by detecting shoulder droop, by noting a preferential position of the infant’s head and decreased spontaneous activity of the shoulders, or both.
Cranial Nerve XII
Tongue movements of the normal newborn are such that fasciculations are difficult to recognize, but atrophy, tongue deviation, or both, can be appreciated.
3.2.3 Motor Examination
Normal newborn motor function varies with gestational age (▶ Table 3.1). From 28 to 40 weeks, with myelination of subcortical motor pathways from the brainstem, the infant develops increasing flexor tone in the legs, with increasing flexor tone spreading rostrally. After 40 weeks, with progressive myelination of the corticospinal tracts, there is a progressive “unfolding” from the flexor tone of the neonate to balanced flexor–extensor tone, increasing voluntary control of axial and extremity muscles, and refinement of movements in a rostral to caudal, proximal to distal fashion. The newborn motor examination is best achieved through the observation of spontaneous motor activity, tone, and posture. Overall, the term infant’s movements are of small amplitude and rapid frequency, whereas those of a preterm infant are slow and athetoid in quality.
| 28 weeks | 32 weeks | 34 weeks | 40 weeks | Red flags | |
| Mental status | Needs gentle rousing to awaken | Opens eyes spontaneously; sleep–wake cycles apparent | At 36 weeks ↑ alertness, cries when awake | -Irritable or lethargic infant | |
| Cranial nerves | |||||
| Pupils | Blinks to light | Consistent pupillary reflex | Fix and follow | -No response to auditory stimulus -“Chomp suck”: clamps down on pacifier but no suck (bulbar dysfunction) | |
| Hearing | Pauses, no orientation to sound | Head + eyes turn to sound | |||
| Suck + swallow | Weak suck, no synchrony with swallow | Stronger suck, better synchrony with swallow | Coordinated suck + swallow at 37 weeks | ||
| Motor | |||||
| Posture | Minimally flexed | Flexed hips and knees | ↑ Flexion at hips and knees | Flexed in all extremities | -Hypotonia -Hypertonia -28-Week infant with jerky movements -Full-term infant with writhing movements |
| Neck flexion | 0 | 0 | 0 | Fair | |
| Reflexes | |||||
| Moro reflex | Weak,incomplete hand opening | Complete extension + abduction | Full Moro reflex (with anterior flexion) | -Asymmetry -If obligatory or sustained, suggests pyramidal or extrapyramidal motor abnormality -Fixed obligate grasp (suggests bilateral hemispheric dysfunction.) | |
| ATNR | Present but weak | Present, involves arm | ATNR appears at 35 weeks | ||
| Palmar grasp | Present with reinforcement | Present without reinforcement | Grasp stronger | Strong grasp, able to be lifted out of bed | |
| Rooting | Present | Present | |||
| Abbreviation: ATNR, asymmetric tonic neck reflex. Source: Adapted from Koenigsberger MR. Judgment of fetal age. Pediatr Clin North Am 1966;13:823–833.7 | |||||
At 28 weeks of gestation, the normal posture of the preterm infant is flexion of the lower extremities with partial abduction at the hip and extension of the upper extremities. Abnormal postures, such as extension of the lower extremities in the term infant or flexion of the upper extremities in the premature infant, indicate hypertonia. Grasping the infant’s arms and pulling the infant to a sitting position allows examination of cervical tone. The normal preterm infant has profound head lag with little to no neck flexion. In contrast, the term infant has both extension and flexion of the neck if normal strength is present. Tone can also be assessed through the vertical and horizontal suspension maneuvers. In the vertical suspension maneuver, the infant is held under the axilla. The hypotonic infant will slip through the examiner’s hands. In the horizontal suspension maneuver, support is held under the trunk with the infant in the prone position. The normal infant can hold the head up and flex the limbs against gravity with the back held relatively straight. The hypotonic infant, when held in this position, will form a u-shape characteristic of hypotonia. Of note, because infants function primarily at the level of the rubrospinal, vestibulospinal, and reticulospinal pathways, they can have significant hemispheric dysfunction with relatively few deficits on the neurologic examination.
3.2.4 Sensory Examination
The full sensory examination assesses sensation to light touch, pinprick, temperature, vibration, and proprioception but is difficult to perform completely in neonates. Sensation can be grossly tested with pinprick and by observation of the neonate’s response, either facial grimace or withdrawal of an extremity, to the stimulus beginning at 28 weeks of gestation. In an infant who is feeding, interruption of the sucking rhythm indicates perception of the sharp stimulus.
3.2.5 Reflexes
Beginning at 33 weeks of gestation, the Achilles, patellar, biceps, brachioradialis, and pectoral reflexes can be elicited. Myotactic reflexes are elicited with sudden tendon stretch by percussion over the tendon. The muscle itself should not be percussed, because muscle contraction occurs even in the presence of lower motor neuron lesions. The plantar response is a nociceptive reflex elicited by noxious stroking of the lateral aspect of the plantar surface from the heel toward the toes. This is not a helpful response to elicit in newborns as the response can be flexor or extensor, depending on the technique used to elicit the response. Unsustained clonus at the ankle (< 8 beats) is normal if symmetrical, but sustained clonus is suspect at any age.
Primitive Reflexes
Several primitive reflexes evolve with maturation of the CNS and reflect the functional integrity of the brainstem. As a group, they tend to be symmetric, and they are modified with age, reflecting the normal maturation of descending inhibitory cerebral influences. Persistence of these reflexes indicates improper maturation of brain structures or injury (see ▶ Table 3.1).
The full Moro reflex consists of bilateral hand opening with upper extremity extension and abduction, followed by anterior flexion of the upper extremities, then an audible cry. This is best elicited by dropping the infant’s head in relation to the body into the examiner’s hands, but any sudden change in position will elicit this reflex. The Moro reflex, which is mediated by the vestibulospinal pathway, is fully elicited at 28 weeks of gestation and disappears at 4 to 6 months of age.
The asymmetric tonic neck reflex (ATNR) is elicited by rotating the head to one side, with subsequent elbow extension to the side toward which the head is turned and elbow flexion on the side of the occiput (▶ Fig. 3.3). This reflex also disappears at 4 to 6 months of age. An obligate ATNR is always abnormal and indicates bilateral hemispheric dysfunction with lack of brainstem inhibition of this reflex.

Fig. 3.3 Asymmetric tonic neck reflex.









