17 Neurological Complications of Radiation Therapy
Introduction
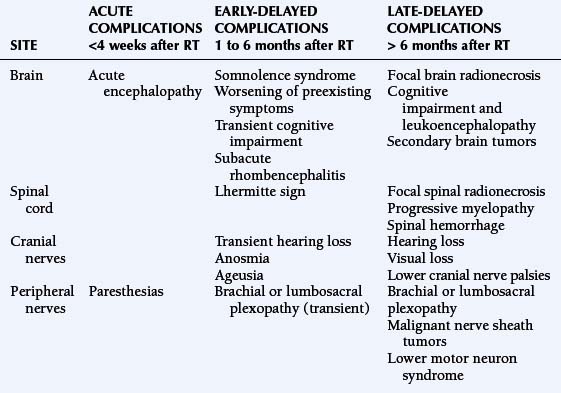
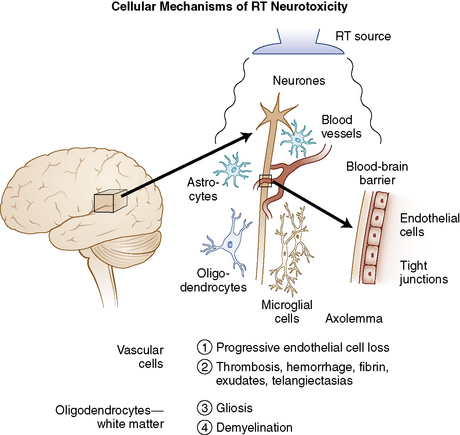
Radiation therapy (RT) plays a key role in neuro-oncology but is associated with significant, sometimes life-threatening, neurotoxicity. The development of new techniques (such as radiosurgery or brachytherapy) has widened the indications of RT to include more benign conditions (e.g., trigeminal neuralgia or vascular malformations), and has increased rates of long-term survivors who may develop late toxicity. Thus, complications of RT have gained increasing interest. Nervous tissue tolerance depends on several currently well-defined factors such as volume, total dose, dose per fraction, and duration of irradiation. In addition, other factors that may increase the risk of radiation-induced toxicity are older age, concurrent diseases (such as diabetes, hypertension), vascular disease, adjuvant chemotherapy, and probably genetic predisposition.1,2 The adverse neurological effects of radiotherapy are usually classified according to the time course in relation to irradiation and include acute disorders (days to weeks), early-delayed complications (1 to 6 months) and late-delayed complications (more than 6 months) (Table 17-1). Radiation damage may be direct to the central or peripheral nervous system, or secondary to vascular or endocrine lesions or to the development of a radiation-induced tumor (Figure 17-1).
HISTOPATHOLOGY
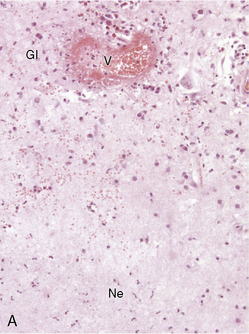
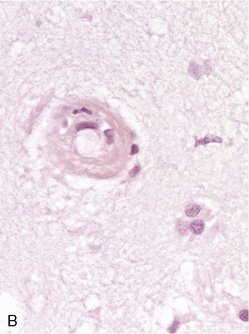
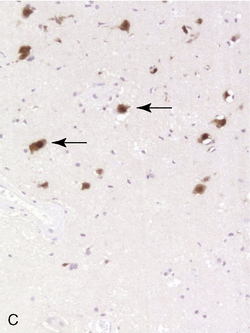
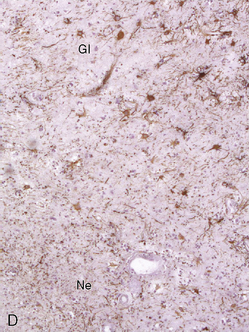
Due to the difficulty in obtaining irradiated human tissue, histopathological studies of irradiated brains in human are scarce. However, a few autopsy studies in adults and children are available and show similar features of vascular and demyelinating lesions at light microscopic level. Lai et al.3 studied the brains of five adult patients with primary CNS lymphoma who were in complete remission, but who died after combined modality therapy with WBRT and chemotherapy. The MRIs showed cerebral atrophy, ventricular dilatation, and white matter hyperintensity on FLAIR and T2 images. Occasional enhancing lesions were observed. The corresponding histopathological lesions were myelin and axonal loss, spongiosis, gliosis in white matter, fibrotic thickening of small blood vessels in the deep white matter, and atherosclerosis of the large vessels in the circle of Willis. All patients but one were older than 60, and symptoms of neurotoxicity developed within 3 months of completion of treatment. An autopsy study was performed in 34 children with gliomas, 22 of whom had undergone CNS radiation therapy.4 Causes of death were not detailed in this study and the cognitive status of the children before they died was unknown. Lesions such as demyelination, focal necrosis, cortical atrophy, endothelial proliferation, vascular thrombosis, and vascular thickening were more frequently observed in irradiated brains, whereas neuronal degeneration, cerebral edema, and gliosis were common in irradiated and nonirradiated brains. Demyelination was observed at all time points from 6 months but was more frequent 9 months after radiotherapy. Vascular changes appeared as a late effect of radiation injury. Panagiotakos et al.5 performed an original and extensive study on human normal and irradiated white matter brain samples from surgical biopsies of glial tissue around tumor. Histological assessments of human tissue were completed by ultrastructural analysis and immunohistochemistry. Samples from irradiated patients exhibited persistent loss of oligoprogenitors starting as early as 2 months after radiation, whereas the decline of more mature oligodendrocytes only started beyond a year after irradiation. Early and transitory endothelial cell loss was noted. Myelin sheaths showed signs of degradation. Signs suggesting axonal damage were only seen late after irradiation. Neuronal cell bodies seemed to be spared from radiation injury.
Radiation-induced histolopathological lesions in brain were studied in rats in a few prospective studies, using either only light microscopy analysis or more sophisticated methods such as immunocytochemical and ultrastructural analysis. Kamiryo et al.6 studied histological changes in the rat brain within 1 year of radiation at doses of 50, 75, and 120 Gy, mimicking therapeutic radiosurgery. The authors observed time-dependent and dose-dependent changes. The first lesions to appear were morphological changes in astrocytes, followed by vasodilation and fibrin deposition in capillary walls for all the studied doses. BBB leakage (Evans blue permeability assay) was observed only after 75 and 120 Gy, and necrosis only after 120 Gy. The time course of these lesions varied dramatically with radiation dose: after 120 Gy, the first lesions were observed only 3 days after irradiation and the whole set of lesions occurred within 4 weeks, whereas after 50 Gy, first lesions were only seen at 3 months and developed over 12 months.
An earlier study by Calvo et al.7 focused on radiation-induced damage in the choroid plexus of the rat brain after a single dose of 17.5 to 25 Gy. They observed early morphological changes in the epithelial cells, followed by interstitial fibrosis associated with degenerative changes of arterioles and thrombi. Severity of lesions was dose and time dependent. The same authors later showed that necrosis was more frequent and occurred earlier in the fimbria than in the internal capsule and corpus callosum. They found a correlation between the incidence of necrosis in the white matter, seen after a latent interval of 26 weeks, and earlier changes in the vasculature such as blood vessel dilatation, blood vessel wall thickening, endothelial cell nuclear enlargement, and hypertrophy of perivascular astrocytes.
Fractionated (eight fractions) WBRT (40 Gy) was delivered to adult rats by Yoneoka et al.,8 more closely modeling therapeutic irradiation in humans. Though rats showed radiation-induced cognitive dysfunction, no histological abnormalities were found in irradiated brains over 12 months after irradiation. This study suggested that cognitive dysfunction can either precede morphological changes in the brain, or even arise without them. It is worthy of note that only light microscopic examination was performed. Vascular permeability was not assessed.
Iradiation of the spinal cord led to progressive abnormalities in the white matter, beginning at 19 weeks, for doses greater than 17 Gy. The spinal cord of paralyzed animals showed areas of necrosis and demyelination, but neither gross vascular lesion nor inflammatory infiltrate was found.9 Occasional vessel dilation was observed.
PATHOPHYSIOLOGY
The pathophysiology of white matter abnormalities potentially leading to necrosis are not fully understood, but several hypotheses have been proposed. Because histological examination usually shows vascular lesions and demyelination, vessels and glial cells have often been considered as the primary target of radiation injury (Figure 17-1). However, the situation is probably more complicated: recently, the interactions between radiation and other cell types have been studied more closely, as well as the regenerative abilities of the CNS.10 A short discussion of the main aspects of the pathophysiology of RT-related injuries is described in the following sections.
Vascular Damage
Transient disruption of the blood-brain barrier, possibly initiated by sphingomyelinase-mediated endothelial apoptosis, is thought to be responsible for the acute or early-delayed, steroid-responsive forms of radiation toxicity.11–13 A vascular theory has also been advocated to explain radiation necrosis. Necrosis would be a consequence of ischemia secondary to blood vessel damage. Vascular damage is indeed prominent during radionecrosis, including thrombosis, hemorrhage, fibrinous exudates, telangiectasias, vascular fibrosis/hyalinization with luminal stenosis, and fibrinoid vascular necrosis. Furthermore, a progressive endothelial cell loss and vessel rarefaction seems to precede white matter necrosis.12 Thus, a cascade (involving signaling molecules among others) could be initiated at the time of irradiation, producing gradual cell loss throughout the clinically silent period.3 At the molecular level, VEGF seems to play a pivotal role in the endothelial cell loss.9 This progressive loss would eventually lead to overt necrosis.14 Despite these findings, several points argue against a purely ischemic model: first, neurons are very sensitive to ischemia and should be prominently damaged if the lesion was primarily vascular, whereas neurons are in fact largely spared during radionecrosis.15 Second, vascular damage is not always present in radionecrosis.16 Other cellular mechanisms may be involved and perpetuate vascular damage or contribute to edema, gliosis, and demyelination in the brain, such as upregulation of diverse adhesion molecules,17 production of cytokines,18,19 or cumulative oxidative stress in endothelial cells.
Oligodendrocytes
The demyelinating lesions observed after RT underscore the putative role of oligodendrocytes as a target of radiation damage. Oligodendrocytes are responsible for the production of the myelin sheath in the CNS and derive from progenitor cells such as O-2A. CNS radiation induces depletion of oligodendrocytes and suppresses, at least transiently, the production of oligodendrocyte progenitors,20–22 possibly through a p53-dependent pathway.23–25 However, the contribution of demyelination in tissue destruction remains questionable since severely demyelinating conditions such as multiple sclerosis do not lead to overt necrosis.15
Other CNS Cell Types
Several studies over the past few years have focused on the potential role of neurons, astrocytes, and microglia in the development of radiation-induced lesions, either as primary targets or through alterations of their regulatory capacity.26–28 Particularly noteworthy is the possible role of microglia29 that may enhance radiation injury through persistent oxidative stress.30,31 Radiation damage to the subventricular zone, a tissue containing glial and neural stem cells, was reported more than 25 years ago.32 Recent studies have found a dose-dependent reduction of neural stem cells of the subependyma after irradiation in this region.33,34 Their implication in radiation injury thus seems probable but remains to be elucidated.
Sequelae of Radiation Therapy to the Brain
ACUTE ENCEPHALOPATHY
Acute encephalopathy usually appears within 2 weeks after the beginning of cranial RT, often a few hours after delivery of the first fraction. The patient presents with nausea and vomiting, drowsiness, headache, dysarthria, and a worsening of preexisting neurological deficits, sometimes associated with fever. The clinical course is usually favorable, but herniation and death have been reported in patients with large tumors who have already presented with intracranial hypertension (e.g., in multiple metastases, posterior fossa tumors, or intraventricular tumors). Large doses per fraction (usually >3 Gy/fraction) are the main risk factor: Young et al.35 reported acute radiation damage in 50% of patients with brain metastases treated with 15 Gy in two fractions, and Hindo et al.36 reported four deaths within 48 hours of a 10 Gy RT given in one fraction. As these large doses are no longer in use, this syndrome is rarely seen. However, a minor form of this condition occurs in many patients, consisting of nausea and moderate headache occurring within hours following cranial irradiation. Steroids may help in preventing or limiting the consequences of acute encephalopathy, especially in patients with large primary or secondary brain tumors or with considerable edema, particularly those at risk of herniation. In such patients, daily doses of steroids of at least 16 mg dexamethasone should be prescribed 48 to 72 hr before the first fraction; a limitation of dose per fraction (2 Gy or less per fraction) is also recommended in this situation.37,38 The pathophysiology of acute complications supposedly results from radiation-induced blood-brain barrier (BBB) disruption, accounting for a rise in intracranial pressure.39 To prevent this complication, surgical debulking should, ideally, be carried out before starting RT treatment.
EARLY-DELAYED COMPLICATIONS OF RT
Several early-delayed clinical patterns have been described (Table 17-1). They occur 2 weeks to 6 months after RT. The pathophysiology is thought to be due to a transient demyelinating process triggered by BBB disruption and/or selective oligodendrocyte dysfunction.
Somnolence Syndrome
This condition was first described in the late 1920s in children receiving low-dose RT for scalp ringworm. Several studies reported cases of children who developed somnolence syndrome 5 to 8 weeks after prophylactic cranial RT for leukemia40,41; other reports have shown that it also occurs in adults. The incidence of somnolence syndrome varies greatly (with figures ranging from 8%41 to 84%42; this difference is related to various factors including tumor types, radiation dose, fractionation, and diagnostic criteria).43 Prominent symptoms include drowsiness, hypersomnolence, nausea, and anorexia. Headache and/or fever may also be reported. Friends or family often notice irritability, attentional deficits, and short-term memory impairment. The clinical severity of this complication is variable, with extremes ranging from minimal disorders to sleep periods of over 20 hours a day.41 MRI studies are not contributory. Electroencephalographic abnormalities include nonspecific diffuse slow waves.43 Most studies report a monophasic course of symptoms, usually with a favorable outcome within a few weeks. However, a prospective study on 19 adults treated for primary brain tumors with cranial RT (45 to 55 Gy) reported a biphasic pattern of symptoms with two critical periods (from the 11th to the 21st day and from the 31st to the 35th day) following RT.44 Furthermore, in this study, an accelerated fractionation led to significantly more severe drowsiness and fatigue than a conventional scheme. Some authors advocate the use of steroids during and after radiotherapy as prophylactic or symptomatic treatment.45 A prospective double-blind randomized trial in leukemic children found that a dose of 4 mg/m2 of dexamethasone during cranial radiotherapy reduced the incidence of somnolence syndrome (17.6% vs. 64.3%) as compared to a dose of 2 mg/m2.46
Worsening of Preexisting Symptoms, or Tumor Pseudoprogression
In patients under treatment for malignant brain tumors, a worsening of preexisting neurological focal deficits leads to concerns over tumor progression, especially when observed in association with features of the somnolence syndrome and with transitory cognitive impairment. This complication arises within 6 weeks to 3 months after RT, and is clinically impossible to differentiate from progressive disease. Neuroimaging may be normal or show edema and contrast enhancement within the tumor bed, a situation that does not allow this syndrome to be differentiated from tumor recurrence and explains why inclusion of patients in experimental regimens for “recurrence” is not indicated during this period47; it is worth noting that this radiological pattern can also be associated with no clinical worsening—“pseudoprogression” rates can reach 20% after a concomitant temozolomide and radiotherapy regimen used to treat glioblastoma and may be associated with better tumor response.48 Improvement usually follows within a few weeks or months and a close followup of CT or MR scan will show spontaneous regression within 4 to 8 weeks. As in the somnolence syndrome, the treatment lies in supportive care with steroids. Improvements in imaging techniques such as magnetic resonance spectroscopy (MRS) may help in distinguishing between pseudoprogression and true progression but are limited by the fact that residual tumor is often still present within the irradiated area.
Transient Cognitive Decline
A transient cognitive decline can be observed within the first 6 months after cranial RT, mainly affecting attention and recent memory, and may sometimes be associated with a somnolence syndrome. Armstrong et al.49 prospectively followed five patients treated for primary brain tumors: memory impairment was conspicuous in all patients 1.5 months after focal cranial RT (43 to 63 Gy), but complete regression was observed after 2.5 to 10.5 months. In another prospective study by Vigliani et al.50 comparing 17 patients treated with focal cranial RT (54 Gy) for good-prognosis gliomas and 14 matched control patients who did not undergo RT, 36% of the patients had a significant early-delayed impairment of their reaction test, with a return to normal baseline performance 12 months after RT. This test result was correlated with their occupational status: 69% of the patients could not work at 6 months, whereas 73% had continued or resumed their jobs at 1 year. In our experience, informing patients about this possible difficulty in returning to a normal life (particularly work), at least during the first 6 months following radiotherapy, is useful. Although severe and, in some cases, persistent early-delayed symptoms have been occasionally reported,51 it is of note that transient cognitive impairment does not appear to be a clear-cut prognostic factor predicting the further development of long-term cognitive disorders.
Subacute Rhombencephalitis
Distinct from brainstem radionecrosis, which occurs later, early-delayed subacute rhombencephalitis may be observed about 1 to 3 months after RT using portals involving the brainstem, as in ocular, pituitary, or head and neck tumors. The clinical picture includes ataxia, dysarthria, diplopia, and/or nystagmus as well as auditory loss. In some cases, the cerebrospinal fluid analysis shows inflammatory changes. MRI may demonstrate white matter abnormalities appearing as grossly round or more extensive T1-weighted hypointensities and T2-weighted hyperintensities affecting the brainstem and the cerebellar peduncles; the lesions may enhance after gadolinium injection.52,53 The condition usually improves progressively over a few weeks to a few months, either spontaneously or with steroids, but coma and death have been reported in rare cases.54,55
LATE-DELAYED COMPLICATIONS OF RT
Focal Brain Radionecrosis
Focal radionecrosis constitutes a challenging complication of radiation therapy because it often mimics tumor recurrence and its functional consequences can be devastating. This complication may occur not only in patients who received local RT for a primary or metastasic brain tumor but also in patients without brain lesions with a history of RT for extraparenchymal lesions, in whom normal brain was included in the radiation field (head and neck or pituitary tumors, meningiomas, skull osteosarcomas). A classical example is the bilateral medial temporal lobe necrosis that results from RT for pituitary or nasopharyngeal tumors. This once frequent complication of conventional RT has become rarer over the last 20 years, as a consequence of the generalized use of safer irradiation protocols. It has been shown that the upper limits of a “safe dose” were defined by a total dose of 55 to 60 Gy administered to a focal field with fractions of 1.8 to 2 Gy per day. Vascular risk factors such as diabetes, old age, and associated chemotherapy may also favor the potential development of radionecrosis. However, patients without any particular risk factors may develop radiation necrosis, probably because of an individual, unpredictable sensitivity to irradiation.56 The focal delivery of a single large radiation fraction during “radiosurgery” may also lead to focal necrosis of the brain adjacent to the irradiated lesion. In arteriovenous malformations (AVM), the incidence of brain necrosis ranges from less than 5% to 20% of cases, with location and volume found to be the main risk factors.57–59 After standard RT, radiation necrosis generally occurs within 1 to 2 years,60 but it has also been observed after several decades. As described above, shorter latencies (as short as 3 months) have also been reported, especially in patients treated with interstitial brachytherapy61 or radiosurgery. Patients may experience seizures (first symptom in about 50% of cases), intracranial hypertension, and/or focal neurological deficits.62–64 Such symptoms closely mimic tumor recurrence or progression.
Diagnosing radiation necrosis is often a challenge. In many cases, CT and MR scans show a tumor-like pattern, often indistinguishable from tumor progression or recurrence.65 As diagnostic assessment based on clinical and standard neuroimaging data is difficult, many studies have tried to address the problem of noninvasive differentiation between tumor recurrence/progression and radionecrosis. Positron emission tomography (PET) with 18F-fluorodeoxyglucose66 or 11C-methionine, single photon emission computed tomography (SPECT) with 201thallium or marked methoxy-isobutyl-isonitrile (99mTc-MIBI),67 and, more recently, the use of 3-[123]iodo-alpha-methyl-l-tyrosine (IMT)68,69 have been used to assess the nature of the lesions. In typical cases, radionecrosis is characterized by hypometabolism and tumoral growth by hypermetabolism. The more recent development of magnetic resonance spectroscopy (MRS) seems promising70: spectral analysis of necrosis areas shows an overall, harmonious decrease of metabolite peaks, and a possible increase of lipids corresponding to cellular necrosis; no lactate peak is observed.71,72 However, none of these techniques offers 100% sensitivity or specificity.73,74 One of the reasons for limitations is the frequent coexistence of radiation-induced necrosis with viable tumor tissue within the same area, a situation that obviously renders clear cut distinction impossible.37 In some cases, angiography may provide further information, with an avascular mass seen in patients with radionecrosis; however, the risks and benefits of this procedure must be carefully weighed. While neuropathological examination remains the diagnostic standard (Figure 17-2),75 even pathological analysis may be difficult because of the frequent mixture of both residual/recurrent tumor and radiation necrosis within the lesion.13
Resection of necrotic foci is often the best treatment in symptomatic cases. Steroids are generally used, with possible long-term improvement37; however, steroid dependence does occur. Other treatments have been reported in this setting, but their efficacy has not yet been addressed in large studies: anticoagulants have been prescribed by Glantz et al.76 in eight glioma patients (seven with histological evidence of necrosis) after the failure of steroids, leading to improvement in five patients. In our experience, anticoagulants have been somewhat disappointing. Further assessment of this therapy is required to confirm those results. Some authors have advocated the use of hyperbaric oxygen (HBO), with the rationale that HBO increases the tissue pO2 and enhances angiogenesis. Chuba et al.77 treated ten patients with CNS radionecrosis (proved by biopsy in eight cases) with 100% oxygen at 2.0 to 2.4 atm for 90 to 120 minutes/session in at least 20 sessions. All patients were stabilized or improved initially, and the six surviving patients showed durable improvement after 3 to 36 months. However, most patients were given steroids, and the respective effect of each treatment is not clear. HBO treatment was also reported to improve radionecrosis due to radiosurgery.78,79 The possible role of HBO in radiation-induced neurotoxicity needs to be evaluated in prospective trials.80 Other drugs or combinations such as pentoxifylline, alpha-tocopherol,81 low-iron diet, desferrioxamine, and pentobarbital1 have also been proposed occasionally without definite evidence of efficacy. The usefulness of radioprotective agents such as difluoromethylornithine (DMO),82 U-74389G (a 21 aminosteroid83), or others84–87 in reducing the risk of necrosis remains to be determined. Preclinical studies have suggested that embryonic stem cell-derived glial precursors could be used as myelinating transplants in demyelinated postradiation experimental lesions.88
Several assays have been developed to identify individuals at risk for radiation sensitivity, such as analysis of the survival fraction of cultured skin fibroblasts after 2 Gy irradiation,56 study of radiation-induced chromosomal aberrations, search for the ataxia-telangectasia mutation, and the G2 cell-cycle phase delay analysis.1,89 However, to date, such assessments have not reached the clinical setting.
Cognitive Dysfunction and Leukoencephalopathy
Considering cognitive dysfunction as a consequence of RT alone would result in a considerable overestimation of the incidence of radiation-induced sequelae. Cognitive impairment may be the consequence of complex interactions90 between preexisting cognitive abnormalities (especially in the case of brain tumors), brain tumor growth, concomitant treatments (such as chemotherapy, antiepileptic91 or psychotropic drugs), paraneoplastic encephalomyelitis, and endocrine dysfunction. In practice, this should lead to a precise individual workup in patients with potential radiation-induced cognitive impairment, but also to a careful and critical interpretation of the higher cognitive dysfunction rates found in the literature. Interestingly, a study comparing 195 low-grade glioma patients (104 had undergone RT during the previous years) to low-grade hematological patients and controls, showed that cognitive dysfunction was mostly tumor-related; patients treated with doses per fraction over 2 Gy were the only ones to develop RT-linked memory impairment.92 A more recent study of these patients followed up for 12 years has shown a progressive cognitive decline in attentional and executive tasks in patients treated with radiotherapy fractions less than 2 Gy/fraction compared with unirradiated patients, which was not apparent after 6 years follow-up.92a
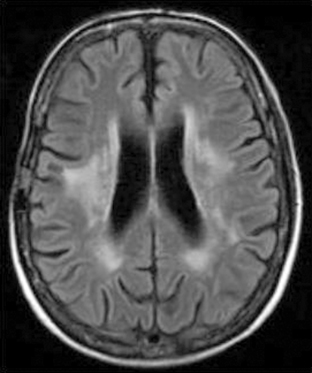
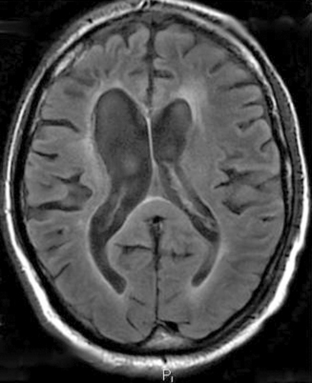
Recent studies seem to confirm that RT plays a limited part in cognitive decline when using modern irradiation procedures.93–95 Nevertheless, several factors have been clearly linked to an increased risk of leukoencephalopathy (Figure 17-3):
Methotrexate (MTX) is clearly implicated in combined toxicity; neurotoxic by itself, it is responsible for frequent cognitive dysfunction when associated with RT. In children, most studies to date have concluded that the combination of cranial irradiation and intrathecal MTX was associated with declines in both IQ and achievement scores.103 In adults treated with WBRT (40 Gy + 14 Gy boost) and a combination of intravenous and intrathecal MTX for CNS lymphoma, the incidence of severe progressive cognitive impairment increases with age, reaching 83% in patients over 60 years.104,105 The timing of MTX chemotherapy is important, because the cognitive dysfunction rate is higher whenever MTX is prescribed during or after RT. This drug should therefore be given before irradiation. Data about the neurotoxicity of other combinations are sparse, but agents such as nitrosourea, cisplatin, etoposide, cytarabine, or actinomycin D are also suspected to increase radiation-induced cognitive toxicity. Multidrug regimens or high-dose chemotherapy combined with WBRT are probably associated with a higher risk of neurotoxicity.106 Although there is a progressive continuum between mild to moderate cognitive impairment and severe fatal dementia, we will consider the two conditions separately.
Radiation-Induced Mild to Moderate Cognitive Impairment
A mild to moderate cognitive dysfunction is more frequent in long-term survivors than real dementia. The features of this condition are not perfectly defined, as results greatly vary according to the studies, probably due to neuropsychological evaluation procedures, duration of follow-up, and population discrepancies.107
In most reported cases, cognitive impairment affects mainly attention and short-term memory, while intellectual functions are generally preserved as assessed by neuropsychological evaluations. Nevertherless, most patients have to decrease or even discontinue their professional activities. CT scan may be abnormal, showing periventricular hypodensities, an increase in the normal interface between white and gray matter, and ventricular enlargement. However, there seems to be no correlation between CT-scan abnormalities and the degree of cognitive impairment. MRI shows variable degrees of T2-weighted hyperintensities in the white matter, with a gross correlation between neuropsychological status and white matter lesions (Figures 17-3 and 17-4).108
The course of the disease is difficult to predict: some patients deteriorate slowly while the majority apparently remains stable. Progression to dementia is seldom reported. There is no recognized treatment for this syndrome although some authors have advocated the use of methylphenidate for symptomatic relief.109 More recently, anticholinesterase drugs have been used with encouraging results.110 Data from animal studies have also shown that the administration of erythropoietin (EPO) may prevent cognitive impairment.111
Free-radical scavengers, such as amifostin or angiotensin-converting enzyme inhibitor (ACEi) could have a protective effect.111b Amifostin is already under clinical investigation with controversial results,111c but to date, despite encouraging preclinical data, no trial has been conducted with ACEi.
Radiation-Induced Dementia
The incidence of this devastating complication varies widely in the literature (from 0% to more than 60%) according to the series. In a large review of several studies comprising 748 adult patients, the incidence of severe cognitive impairment compatible with dementia was at least 12.3%.112 More recent studies and clinical practice provide less cause for alarm.30,113
The clinical picture is characterized by a “subcortical dementia” pattern that probably reflects the consequences of diffuse white matter injury, occuring in 69% of patients within 2 years of radiotherapy.107
Patients present with progressive memory and attention deficits, intellectual loss, gait abnormalities, emotional lability, apathy, and fatigue.114 The absence of hallucinations or delirium and the very unusual occurrence of aphasia, agnosia, or apraxia (deficits suggesting cortical involvement) are important clinical features for narrowing the differential diagnosis, especially in elderly patients. Depression is frequent, but antidepressants do not improve cognitive function. Eventually, patients may develop gait ataxia, incontinence, and sometimes a picture of akinetic mutism. Nonspecific features such as seizures, pyramidal or extrapyramidal signs, or tremor are also frequently encountered in the course of the disease. Neuroimaging always shows diffuse white matter lesions, best seen on MRI as T2-weighted hyperintensities, associated with cortical and subcortical atrophy as well as ventricular enlargement (Figure 17-4). When performed, the lumbar puncture usually shows normal to moderately elevated (< 1 g/l) CSF protein levels.
No specific treatment is currently able to cure radiation-induced dementia. However, as the clinical features are similar to those of normal-pressure hydrocephalus, some authors have advocated ventriculoperitoneal shunting; this procedure does improve the quality of life in a few selected patients.30,115,116
Deterioration occurs in about 80% of cases, leading to the death of the patient; stabilization is possible (18% of cases). Lasting improvement is exceptional. Death generally occurs within 1 to 48 months after the onset of the disorder.102
Radiation-Induced Brain Tumors
The precise role of RT in the development of a tumor is difficult to determine and cannot be assessed with certainty, in great part because these tumors have no distinctive features compared to unirradiated patients. However, data from animal and epidemiological studies indicate that irradiated patients or animals are more likely to develop a second brain tumor than would have been expected from the control data.117
The relative risk of developing a radiation-induced tumor has been studied in several large studies. A study by Ron et al. of 10,834 patients treated with low-dose cranial and cervical irradiation for Tinea capitis (mean dose to neural tissue: 1.5 Gy) showed a relative risk of developing a tumor of 6.9; the risk for glioma was 2.6.118
In another study of 10,106 survivors of childhood cancers by the British Childhood Cancer Research Group,119 the relative risk of developing a secondary CNS tumor was 7. Most other studies have found similar results.120,121 However, the risk is probably higher in patients treated for acute lymphoblastic leukemia (ALL): a large retrospective cohort study of 9720 children122 found a relative risk of developing a nervous system tumor as high as 22. In another setting, a large study on second brain tumors in 426 patients with pituitary adenoma treated with surgery and radiotherapy showed a 2.4% risk at 20 years.121
Criteria for a radiation-induced tumor include: (a) long interval between radiotherapy and the occurrence of the second tumor (the mean onset delay is 12 years, with cases ranging from 1 to 40 years); (b) tumor growth within the radiation portal or at its margins; (c) a different histological subtype. After stereotactic radiosurgery, radiation-induced neoplasms are extremely rare, with only four reported cases in the literature.123 Three types of tumors have been reported to be linked with cranial irradiation: meningioma in about 70% of cases, glioma in 20%, and sarcoma in fewer than 10%. More than 300 cases of radiation-induced meningiomas have been reported in the literature; female predominance is less prominent than in spontaneous meningiomas.124 The risk of occurrence correlates with radiation dose: low-dose RT induced a relative risk of 9.5 in one study,118 whereas high-dose RT was linked to a relative risk of 37.120 The tumor emerges after a long latency period: a review found extremes ranging from 2 to 63 years (mean 18.7 years) after high-dose RT.125
Most patients (68%) had been irradiated during childhood, and the interval between RT and the onset of the tumor was shorter in younger patients; however, the radiation dose did not influence the latency. Radiation-induced meningiomas are often multiple and recurrent with malignant histological features.126,127 Unlike sporadic meningiomas, NF2 gene inactivation and chromosome 22q deletions seem to be less frequent in radiation-induced meningiomas, while other chromosomal lesions (especially loss of 1p) possibly induced by irradiation, may be more important in the development of these tumors.128,129
Radiation-induced gliomas are much less frequent. Since 1960, about 120 cases have been reported in the English literature;130,131 fewer than half of them were glioblastomas. In the group of patients treated with RT for acute leukemia, multifocality occurred in 20% of cases. The median delay of onset ranges from 6 to 9 years.131 The prognosis of these tumors is poor: intrinsic resistance to treatment as well as previously received aggressive therapies considerably limits the applicable therapies.
Molecular alterations are apparently the same in sporadic and radiation-induced gliomas.132 Fewer than 40 cases of sarcomas have been reported to date, different and they consist of several histological types (e.g., gliosarcomas, meningiosarcomas, neurofibrosarcomas).117
Radiation Vasculopathy
Large and Medium Intracranial and Extracranial Arterial Injury
An arteriopathy affecting the large cervical blood vessels, especially the carotid artery,133 may be a complication of cervical radiation therapy, usually administered for lymphomas or head and neck cancers. Intracranial vessels may also be affected. The main early-delayed vascular complication is carotid rupture,134,135 which usually follows a few weeks after cervical RT and surgery for head and neck tumors. Associated skin lesions such as necrosis or wound infection are common. The outcome of this exceptional complication is, of course, very poor.
Late-delayed complications are more frequent, and generally occur many years after RT (median time about 20 years for extracranial, 7 years for intracranial artery lesions). The lesions are similar to those induced by atherosclerosis, but are often located in unusual places for common atherosclerosis and occur in an accelerated fashion. It has been observed that the larger the diameter of an irradiated artery, the longer the latency between RT and the onset of vasculopathy, a fact that might explain the shorter latency of RT-induced vasculopathy in children. Shorter latencies have also been reported with interstitial radiotherapy.136 The dose required to induce vascular lesions usually exceeds 50 Gy, but the type of irradiation, fractionation, and portal differs greatly from one case to another. The lesions consist of one or more stenoses or occlusions in the arteries included within the radiation portal. The diagnosis, suspected when a cervical murmur is heard in the immediate vicinity of radiation-induced skin lesions, relies on magnetic resonance angiography, ultrasound examination and arteriography.
The treatment is similar to that of usual atherosclerotic lesions; in the event of carotid stenoses, endarterectomy may be appropriate. However, surgery may be more difficult than in unirradiated patients because of vascular fibrosis and skin lesions, with higher postoperative risk of infection or healing problems. In other patients, antiplatelet agents may be prescribed if there is no contraindication. Some authors have advocated lowering serum cholesterol levels to prevent the development of such lesions in patients at risk.137
Radiation-Induced Vasculopathy with Moyamoya Pattern
Intracranial vasculopathy leading to a progressive occlusive disease and a moyamoya pattern (characterized by abnormal anastomoses and netlike blood vessels), accounting for focal seizures, strokes, or transient ischemic attacks, may follow intracranial irradiation, especially in very young children. This complication is particularly frequent in children treated for optic chiasm glioma, a condition often associated with neurofibromatosis type 1 (NF-1, which is a risk factor for vasculopathy itself). It may also occur with other tumors such as brainstem glioma and craniopharyngioma.138 In a series139 of 69 children (11 with NF-1) treated for optic pathway glioma with RT (median dose 55 Gy), 13 (19%) developed clinical and radiological signs of vasculopathy after a median latency of 36 months. The strong association between NF-1 and moyamoya is one of the reasons why radiation has been replaced with chemotherapy in younger children.113 The treatment focuses on preventing further strokes through surgical revascularization techniques; calcium blockers such as flunarizine have been advocated by some authors.140–143 The role of antiplatelet agents has not been defined in this setting.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree