Nonaccidental Head Injuries
Few topics in pediatric neurosurgical practice engender so much controversy and elicit such strong opinions as does nonaccidental injury. It is an area that most surgeons wish they never had to encounter because it rarely involves surgery at all, and it often thrusts them into a medical and medicolegal maelstrom that many would prefer to avoid. Although neurosurgeons are practiced in making firm decisions with incomplete information on a daily basis, this arena is altogether different, and for many, it is both unfamiliar and uncomfortable territory. Yet because it is common, and because the opinion of the neurosurgeon often holds considerable weight, it is important to have an overall understanding of what is known and what is at present still unknown in this area. The purpose of this chapter is to provide a practical overview for the neurosurgeon called to manage a case in which the differential diagnosis includes inflicted injury.
52.1 History and Terminology
Because some of the confusion in the field of child abuse arises from semantics and terminology, it is useful to understand the background from which some of the labels used for various “syndromes” arose. That children might present with a complex of signs and symptoms resulting from mistreatment at the hands of their caretakers was widely recognized by the medical field only in the middle of the 20th century, although the French physician Ambroise Tardieu attempted to raise awareness of child maltreatment a century earlier.1 What is challenging, and often handicapping, about the presentation of these particular patients is that the true history of illness is usually withheld. Thus, the clinician must rely on the recognition of patterns of findings to infer that injury has occurred, and that it may not be accidental in etiology.
C. Henry Kempe, a pediatrician and chairman of pediatrics at Children’s Hospital Colorado, Denver, and his colleagues pioneered in the recognition of abusive injury in the United States with their description of children who presented for a variety of reasons but had certain physical and behavioral characteristics in common, and whose symptoms and signs resulted from chronic physical abuse and neglect.2 Their so-called “battered child syndrome” was the first widely promulgated clinical constellation to bring the problem of inflicted injury into the consciousness of general pediatrics.
Moving into the realm of even younger children, John Caffey, a pediatric radiologist at the Children’s Hospital of Pittsburgh, Pennsylvania, noticed the relationship between long-bone metaphyseal fractures, subdural hematomas, and retinal hemorrhages in infants. In the 1960s and early 1970s, the role of angular deceleration forces in the biomechanics of concussive head injury and subdural hematoma was being recognized in primate experiments and in some case reports of adult head injury.3–5 Another event that contributed to how this new syndrome was conceptualized involved a well-publicized case in England during the late 1940s and 1950s, in which a nursemaid confessed to apparently causing injury to a number of her charges by shaking them in order to burp them.6 Thus, it was surmised that manual shaking could generate sufficient angular deceleration of the infant head to result in the subdural hemorrhages commonly seen in these infants, and that shaking was therefore the causative mechanism. Caffey coined the term whiplash shaken infant syndrome to denote this condition, which became known in common parlance as shaken baby syndrome.7,8 Central to Caffey’s concept was that shaking was widely perceived as a nonharmful and acceptable method of discipline for infants, and that caretakers were unwittingly causing highly damaging or fatal injuries to their children by this practice.6
The past two decades have seen increasing recognition that inflicted head injury can take many forms. Single acute neurologic events, acute or healing skeletal trauma, and chronic subdural hemorrhages alone or in combination, with or without retinal hemorrhages, bruising, or signs of physical neglect, may be seen. The common findings of apnea and hypoxia are suspected by many to contribute to the pathogenesis of the more severe end of the acute injury syndrome.9 Neuropathologic findings in the cervical spine have been recognized, and whether trauma in this region, caused by manual shaking or some other mechanism, contributes to the clinical picture is an area of ongoing investigation.10–12 However, because the vast majority of children with inflicted injury have subdural hematomas, hypoxia alone seems unlikely as a full explanation for all the findings. As in other branches of medicine, it has become clear that the relatively simple notions of mechanism and context initially proposed in the 1960s and 1970s provided a useful and practical starting point, but that much more work is needed before clinicians have available a full and generalizable understanding of these types of injuries. For this reason, many authors and child advocacy organizations have adopted terminology that does not imply a single mechanism of injury but instead is more general, if admittedly less riveting, than “shaken baby syndrome.”13
As a matter of definition, in this chapter the terms inflicted injury, nonaccidental injury, and abusive head injury are used interchangeably to refer to trauma resulting from the deliberate application of force to a child.
52.2 Epidemiology
Research in the epidemiology of inflicted trauma has been hampered by the same factors inherent in research into other aspects of this topic, including difficulties with ascertainment, inclusion criteria, and follow-up. Nonetheless, several population-based studies have been conducted, and these serve to estimate the incidence of inflicted neurotrauma. A prospective population-based study in Scotland found that “shaken impact syndrome” occurred with an annual incidence of 24.6 per 100,000 children younger than 1 year of age. Cases were more common in urban areas and during autumn and winter. The risk for sustaining an inflicted head injury by 1 year of age was found to be 1 in 4,065.14 At least 24% of children younger than 2 years of age admitted to the hospital for head injury have sustained nonaccidental trauma.15
Inflicted neurotrauma is a syndrome of young children, with a mean age younger than 1 year.16 In most studies, boys are slightly more at risk than girls, although some studies show equal incidence rates.
Risk factors for inflicted injury include young parents, low socioeconomic status, socially unstable households, single parents, prematurity of the infant, history of prior abuse to the caretaker, and psychiatric or substance abuse histories.17–21 Perpetrators in order of frequency include fathers (37%), boyfriends (20.5%), female babysitters (17.3%), and mothers (12.6%).22 In a significant percentage of cases, evidence of prior trauma is present or inferred, although single events are also common.23–25
52.3 Clinical Presentation and History
The two most common histories given by caretakers when children present with nonaccidental head injury include a history of trivial blunt trauma and no history of trauma. When a history of trauma is obtained, it is most often one of a low-height fall, usually from a bed or other low surface.16,24,26–28 When children present without a history pointing to trauma, they are brought to attention because of specific symptoms or signs, including feeding difficulty or vomiting, lethargy, irritability, abnormal movements, seizures, apnea, and unresponsiveness. Occasionally, the diagnosis will be suspected on the basis of findings noted on routine physical examination, such as an enlarging head or unusual or patterned bruising. When no history of trauma is given and the symptoms are nonspecific, a diagnosis of inflicted injury often may be missed. In one study of 173 children with abusive head injury, it was ascertained that signs and symptoms of inflicted injury had been present, but the diagnosis missed, at prior presentations for medical care in nearly one-third of children.23 The diagnosis was more likely to be missed in young, Caucasian children from intact families who did not present with respiratory compromise or seizures. In 4 of 54 missed cases, the later presentation resulted in a fatality, underscoring the importance of considering the diagnosis of inflicted injury even when symptoms are nonspecific and no history of trauma is provided. Other authors also have discerned racial differences in the evaluation obtained for children presenting for care with similar injuries, reinforcing the fact that ascertainment bias may contribute to missed injuries (or, conversely, to unnecessary testing).29
The best and most helpful history is that obtained at the initial contact. The neurosurgeon should make it clear that the goal is to understand what happened to the child, in order to anticipate what kinds of injuries may have been incurred, to tailor evaluation and management, and to anticipate potential delayed complications. This is true for all head injuries, accidental or otherwise.
After the initial history is provided by the caretaker, specific questions need to be asked and answers obtained. Exactly what happened? At what time did it occur? Who was there? How high was the fall/drop/trajectory? What kind of surface did the baby hit, and with what part of the body? What position was the baby in? Who saw it? If the incident was unwitnessed, who heard it or arrived at the scene? What did the baby look like and do? For how long? What happened next? It may be helpful to describe that what you are trying to create is a “mental video” of the events surrounding the injury. An exact description of the events is invaluable and is best obtained right away. If the person who witnessed the injury is not present, that person should be interviewed as soon as possible.
Because the vast majority of low-height falls in childhood are well tolerated and result in minimal injury, the finding of more serious injuries from this purported mechanism is one of the more common reasons why suspicion of inflicted injury is raised in emergency department and primary care clinicians. This diagnostic criterion falls under the concept of injuries “inconsistent with” or “inadequately explained by” the reported mechanism. However, exactly what mechanism causes what injuries at what age is incompletely understood, although some progress in this area has been made in recent decades (see later section on mechanisms and types of injury). Nonetheless, few clinicians called upon to evaluate potentially injured children are fully knowledgeable regarding the available data in this area. Hence, in practice, the criteria for considering inflicted injury vary among clinicians and hospitals. For example, despite ample evidence to the contrary,30–32 many clinicians still believe that the presence of a skull fracture in an infant is inconsistent with a low-height fall. Epidural hematomas can result from low-height falls in infants, and although they can be serious or even life-threatening, they are only rarely due to inflicted injury.33 Even when similarities in injury types are accounted for, the frequency with which referrals for evaluation for possible nonaccidental injury are made has been shown to be influenced by a number of factors, including the presence of two parents, the insurance status of the patient, and the race of the infant.23,29
Retinal hemorrhages are reported in 65 to 95% of children with inflicted head injury, may be unilateral or bilateral, and are best seen with the use of mydriatics.26,34–36 The exact biomechanics or other conditions necessary to cause retinal hemorrhages are at present not well understood; they can be associated with normal vaginal delivery, coagulopathy, hypertension, accidental trauma, subarachnoid hemorrhage, subdural hemorrhage, papilledema, and some other uncommon conditions, including certain genetic disorders and rare cases of resuscitation.37–46 When accidental trauma is minor or mild, retinal hemorrhages are usually sparse and may be unilateral.15,44,47 However, severe, bilateral retinal hemorrhages, especially if associated with retinal folds or detachments, are associated with major traumatic forces in accidental trauma or with nonaccidental injuries, and they have not been reported from low-height falls.42,48–52
Although some medical conditions can mimic certain aspects of acute and chronic inflicted injury, generally these conditions can be identified with a complete history and physical examination, appropriate imaging studies, and sometimes other specific evaluations, such as laboratory tests.43,53–55 Of somewhat greater difficulty is the distinction between inflicted and accidental trauma, and this will be discussed in more detail below. However, although there may be some diagnostic uncertainties in the assessment of possible nonaccidental trauma, there is no illness or condition known besides inflicted injury that causes the combination of acute subdural hemorrhage, healing skeletal injuries, and severe bilateral retinal hemorrhages (particularly if retinal folds or detachments are seen). When a single severe traumatic event (i.e., one involving very high-magnitude forces) has occurred, acute subdural hemorrhage, acute fractures, and severe bilateral retinal hemorrhages may occur, but this combination of findings has not been reported in association with low-height falls.
52.4 Diagnostic Imaging
Nearly all types of head injury have been reported in the context of inflicted mechanisms, but the most common is acute subdural hematoma.12,15,16,35,56 Often, the hemorrhages are thin but extensive collections over the surface of one or both cerebral hemispheres, as well as in the posterior interhemispheric fissure (▶ Fig. 52.1). In some children, the brain parenchyma appears normal. In other children, parenchymal hypodensities may be present initially or appear within the first 1 to 2 days after trauma and may range from focal and patchy to extensive.57–59 In the latter case, an entire hemisphere or both supratententorial compartments may be affected, the so-called “big black brain”60 (▶ Fig. 52.2). This extensive hypodensity does not appear in all children with inflicted injury but is seen in a subset of those who are the most impaired at presentation. The pathophysiology of this phenomenon is incompletely understood, but it seems to be unique to infants and young children. Diffuse hypodensity is bilateral in two-thirds of cases and unilateral in one-third, with the latter constellation more common in older infants and young children. Unilateral cases often include an affected region in the contralateral medial frontal region due to subfalcine herniation (▶ Fig. 52.2). In such cases, the hypodensity is usually present on the side of the greater subdural hemorrhage.36,58,59,61,62 The observation that one-third of children with this finding have the unilateral form also argues against a pathophysiology related solely to apnea/hypoxia.62 Children in whom unilateral or bilateral “big black brain” develops usually are unresponsive on admission and have a mortality of 67%. Survivors tend to be very young, probably because the ability of the calvaria to expand serves as some protection against brainstem compression and fatal herniation.61 Outcome in survivors of bilateral hypodensity is dismal, with children remaining blind, nonverbal, nonambulatory, and profoundly developmentally impaired, thus making the utility of aggressive acute intervention in such cases arguable.63
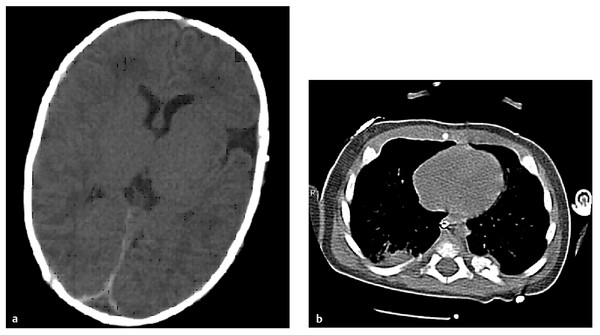
Fig. 52.1 Unenhanced computed tomographic (CT) scan of a 6-week-old baby who was found at home unresponsive with irregular breathing. There was no history of trauma. (a) Axial view through the brain showing interhemispheric blood. (b) CT scan of the chest showing a healing left posterior rib fracture.
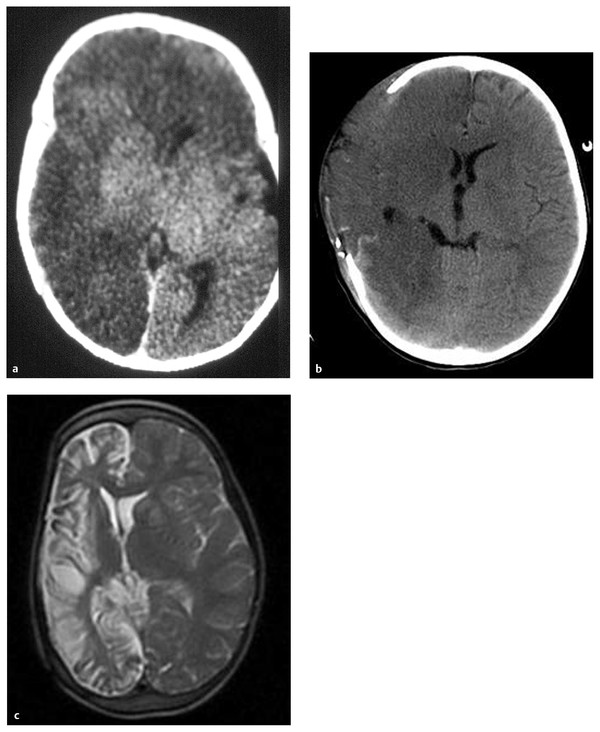
Fig. 52.2 (a) Unenhanced axial computed tomographic (CT) scan showing unilateral hypodensity of the entire hemisphere (“big black brain”) with involvement of the contralateral medial frontal lobe in a child with inflicted injury, likely reflecting subfalcine herniation. (b) CT scan in a child with inflicted injury treated acutely with cranial decompression. (c) Rapid T2 magnetic resonance image 2 years later. Note preservation of the contralateral frontal lobe.
Magnetic resonance (MR) imaging may be helpful in identifying small subdural hemorrhages and parenchymal contusions that may be inapparent on a computed tomographic (CT) scan. However, the early hope that subdural hemorrhages could be reliably dated by MR imaging has not been realized because the multicompartmental nature of the traumatized subdural and subarachnoid spaces makes hemorrhagic collections layer and mix in various ways that may influence their signal characteristics.64,65 Thus, the dating of hemorrhages is only approximate and is not generally accurate to within specific hours or days, as is sometimes needed in criminal investigation. Diffusion-weighted imaging and spectroscopy have been used to corroborate the degree of parenchymal injury seen on CT.66,67 One of the main practical values of MR imaging is that it distinguishes extra-axial cerebrospinal fluid collections from hemorrhagic subdural collections, which when identified point the clinician toward a consideration of a traumatic etiology for an enlarging head (▶ Fig. 52.3). In some children with macrocephaly as the presenting complaint, rapid MR imaging techniques, which do not require sedation (typically, fast-acquisition T2-weighted images in multiple planes), serve as an increasingly utilized means to differentiate chronic subdural collections from the much more common enlargement of the subarachnoid space68 (▶ Fig. 52.4). Skull fractures are noted in approximately 25 to 75% of children, depending on the techniques used to assess them; historically, plain skull films are more likely to diagnose skull fractures than are CT scans, but in the digital era, the resolution of plain films may be decreased, and three-dimensional CT reconstructions with reduced radiation dosage may be the most reliable at present56,69–72 (▶ Fig. 52.5 and ▶ Fig. 52.6). Some fractures and scalp injuries are visible only at autopsy.12,24 Skeletal injuries to the ribs, long bones, or spine occur in 30 to 70% of children with inflicted head injuries.69,73 Fractures of the metaphyses of the long bones and to the posterior ribs are highly associated with inflicted mechanisms, and other injuries, such as spiral fractures of the femur, also occur with increased frequency in this setting. Because the identification of unexplained injuries is one of the most reliable adjuncts to a diagnosis of inflicted injury, a full skeletal survey should be performed, rather than a “babygram” (i.e., a single anteroposterior image of the entire infant) or other less thorough survey. Radioisotope bone scan also may be helpful in equivocal cases to identify subtle acute injury, and follow-up plain films can confirm the presence of healing bone injury.74 Radioisotope bone scan may identify some skeletal injuries not seen on plain films and may be complementary.75
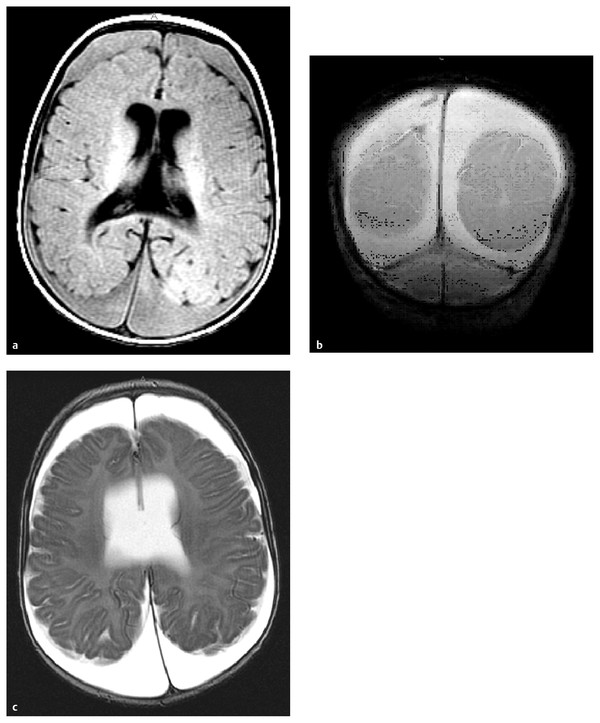
Fig. 52.3 Axial T1-weighted (a), coronal gradient-echo (b), and T2-weighted (c) magnetic resonance images of the brain of a 3-month-old infant with an enlarging head circumference. Note the ruptured parasagittal bridging vein in (b) and the tear in the septum pellucidum, best seen in (c). The infant was also found to have multiple healing fractures. The father, who had been abused as a child, admitted to throwing the infant on the floor and across the room when she cried.
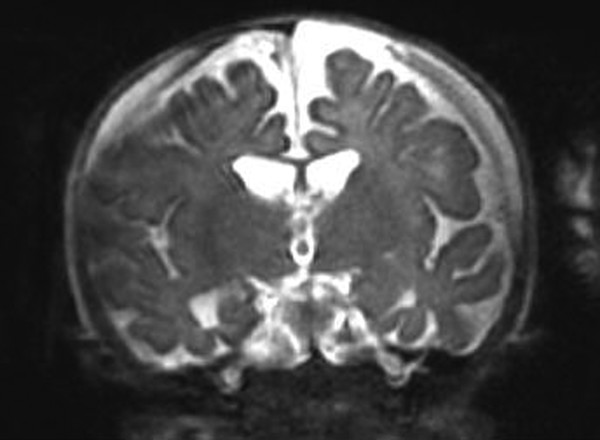
Fig. 52.4 Rapid T2-weighted magnetic resonance (MR) image, coronal view, showing bilateral subdural collections in an infant with an enlarging head. Rapid MR imaging techniques appear to be sensitive in visualizing subdural collections, can be performed without sedation or radiation exposure, and have gained increasing utilization for macrocephaly screening.
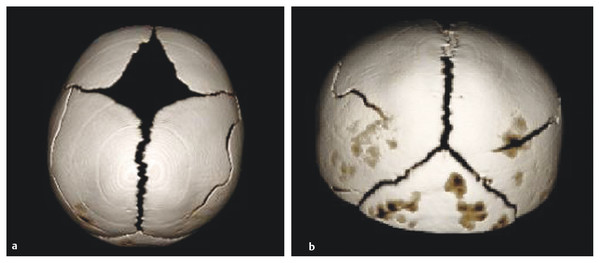
Fig. 52.5 (a,b) Three-dimensional computed tomographic scans of the head of a child dropped while being carried by its mother, who tripped over the family dog. The impact to the child’s forehead caused bilateral parietal fractures. Images were acquired with a reduced radiation dose technique.
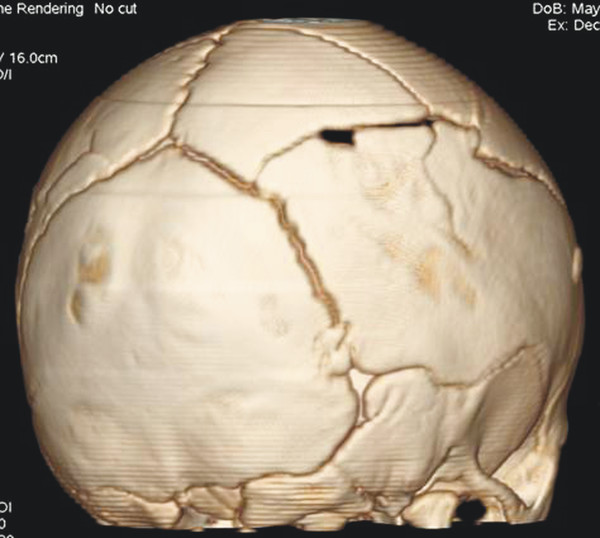
Fig. 52.6 Three-dimensional computed tomographic scan of a child with skull fractures after a reported fall in a bathtub. Note multiple complex fractures. The father later confessed to abuse.
Copy editor, note to Thieme: Caption for ▶ Fig. 52.7 has been moved to where the figure is first called out. Although evidence of injury to the cervical spine has been described with more consistency in several autopsy series, these injuries (which include extradural and intradural hemorrhages, nerve root injuries, and small parenchymal abnormalities) are rarely visualized on MR imaging.12,76–78
Soft tissue injuries including frenulum tears and patterned bruising (e.g., loop marks, bite marks, or bruises in the pattern of a striking object) or burns may be seen.79 Care should be taken to avoid misinterpreting the patterned bruises seen in some folk remedies practiced in various cultures, such as coin rubbing, as inflicted injury.
52.5 Mechanisms and Types of Injury in Infants and Young Children
Part of the confusion in the literature on injury in infants and children arises from semantics—that is, from terminology that is defined differently in different contexts or by different authors. Head injuries can be classified in a number of ways, including by injury type, by mechanism, and by severity. It is worth reviewing the terminology briefly because in the medicolegal context, these semantic differences can be problematic, and the unsuspecting physician acting as a fact or expert witness may find that these terms become a point of controversy during testimony.
First, head injuries may be classified by pathoanatomical injury type. This is the “where and what” of a specific injury. Thus, as is obvious to neurosurgeons, an epidural hematoma is located in the epidural space and is a clot, and scalp contusion, skull fracture, subdural hematoma, intracerebral hemorrhage, diffuse axonal injury, and other injury types also follow this “where and what” terminology. It is useful to keep in mind that many if not most clinical traumatic events produce more that one injury type.
Head injuries also may be classified by mechanism. These include impact and inertial events, the former requiring contact with the head and the latter reflecting movements of the head and/or brain. Inertial forces may be translational, in which the head moves in a straight line, or rotational (also described as angular), in which the head and/or brain moves around a center of rotation. The specific injuries incurred from a traumatic mechanism depend both on the type and the magnitude of the specific forces applied to the head and brain. In most clinical injuries, the head and brain are subjected to multiple types of forces at different magnitudes, even during a single event.80,81 For example, in a motor vehicle crash, the contact of the head with the dashboard results in focal contact forces at the site of impact, while the movement of the brain during deceleration results in the application of diffuse inertial forces throughout the brain parenchyma. A patient subjected to this mechanism may have both frontal brain contusions resulting from impact forces and diffuse axonal injury from inertial forces related to rapid angular deceleration.
Finally, head injuries may be classified by severity. The Glasgow Coma Scale (GCS) and its derivatives for the pediatric population have all been used to categorize acute injuries as mild, moderate, or severe. The original GCS was designed to be used at 6 hours after injury and after resuscitation to compare patients among different centers, and it was validated to be predictive of outcome after head injury in adults when used for that purpose.82 However, it has major drawbacks as a predictive tool in infants and preverbal children and is sensitive to influence by sedative and paralytic agents and intubation.83 In addition, in common parlance, laypersons may think of a skull fracture as a “serious” injury, but from the neurologic point of view, a skull fracture may occur with essentially no injury to the brain and so is not “serious” in the sense of expected long-term consequences. Confusion over this sort of terminology can be vexing when neurosurgeons interact with legal or child protection professionals.
In the context of inflicted injury, these terms and classifications may arise with erroneous assumptions that are worth noting. For instance, with respect to pathoanatomical injury types, subdural hematomas are the most common intracranial hemorrhage in inflicted injuries in infancy, but there are different mechanisms that may be associated with subdural hemorrhages and different lesions that may be misinterpreted on CT scans as subdural hematomas.64,84 Thus, the presence of something that is or looks like a subdural hemorrhage does not in and of itself confirm a diagnosis of inflicted injury. Likewise, some nonaccidental injuries are “life-threatening,” but so are arterial epidural hematomas, which may arise from low-height falls in infants. Thus, the presence of a “serious” or “life-threatening” head injury does not by itself imply an inflicted mechanism, or even a mechanism that is necessarily inconsistent with the history given. Our colleagues in the legal profession who do not have a broad experience with the range of head injuries common in accidental and inflicted injuries may not have as complete an understanding of the crossover between these types of terms, which may lead to frustration when the neurosurgeon is called as a witness. Several articles have been written that detail series of injury types resulting from various accidental mechanisms of injury in infants and young children, including falls from beds at home, falls from beds while in the hospital, and falls in stairways and from heights.85–90 Other authors have approached the question of what mechanisms cause what injury at what age by retrospective or prospective studies of consecutively assessed children admitted or evaluated through emergency departments.15,31,91–93 These studies are remarkably consistent in that they show that, with the exception of epidural hematomas, low-height falls in children (generally from household surfaces with a head-to-impact distance of less than about 3 feet) do not result in life-threatening brain injuries. When small focal collections are interpreted on CT scans as subdural hemorrhages, they usually are found in infants who appear clinically well.84,91–93 This is why the history of a low-height fall in a child with an acute subdural hematoma and neurologic compromise is generally considered grounds to consider inflicted injury as a possible mechanism of injury.16,35,81,94
An exception to the wide body of literature cited above documenting the relative safety of low-height falls is a paper written by Plunkett that is often quoted by defense experts in inflicted injury cases.95 This paper was a retrospective review of data on playground equipment collected by the U.S. Consumer Product Safety Commission (CPSC) National Injury Information Clearinghouse. Data were collected from selected U.S. hospital emergency departments to create a probability sample that could be used to assess consumer product–related injuries. A subset of these injuries underwent more in-depth investigations by CPSC staff. The author of the paper reviewed files in the database for head and neck injuries involving playground equipment that occurred from 1988 to 1999. He found 18 deaths due to falls in children ranging in age from 12 months to 13 years. The article profiles these cases, most of which involve falls from swings, ladders, and platforms. Distances, measured from the body part closest to the ground (not from the head to the ground), ranged from 2 to 10 feet. Most children had skull and/or scalp injuries, and the most common intracranial pathology was subdural hematoma with brain swelling; some children had contusions and/or epidural hemorrhages. In some children, the clinical symptoms were minor initially and then progressed over hours to days. Some children had retinal hemorrhages. About two-thirds of the patients had autopsies. The author concluded that “short-height” falls can cause fatal injuries in children, that retinal hemorrhages can occur, and that a “lucid interval” may be present.
For neurosurgeons who deal with many traumatic injuries, none of these conclusions is surprising. However, there is a difference between these mechanisms and the histories given in many inflicted injury scenarios, which most often describe low-velocity falls from low heights, usually from a stationary reclining position, so that the distance the head falls is less than 2 feet (the average couch is about 18 inches in height). Playground falls typically happen in older children, there is often an initial velocity in addition to free fall acceleration (such as occurs on swings and seesaws or when children are jumping or swinging on bars), and the fall height of the head itself may be several feet greater than the distances cited for the body part closest to the ground. Contact and other types of subdural injuries (discussed further below), contusions, and intracranial lesions can indeed progress over time as brain swelling occurs, particularly if the seriousness of the injury is not initially recognized. Contusional swelling, hyponatremia, hypoventilation, and seizures can all contribute to a worsening clinical status. Retinal hemorrhages, seen in some of the children reported in Plunkett’s paper, have been previously documented in a number of accidental scenarios, particularly those associated with acute subdural hematoma.15,40,42,47
Because subdural hematomas are so common in cases considered as possibly inflicted injuries, it is worth discussing briefly the different types of subdural hematomas with respect to what structures constitute the sources of hemorrhage and the different mechanisms involved. Although at least one neuropathologist has suggested that the subdural hemorrhages seen in inflicted injury might be due to hypoxia alone,96 most researchers continue to assume that the hemorrhages are traumatic in origin. This assumption is based on the frequent finding of additional signs of mechanical injury, as well as the lack of subdural hemorrhage in most cases of hypoxia/ischemia in infancy with other causes. As described below, it may be that more than one mechanism is at work to explain the varied findings encountered.
Classically, convexity subdural hemorrhages in adults are thought to occur from rapid angular deceleration, in which the head stops moving but the brain continues to rotate within the skull. This causes stretching and ultimately rupture of the parasagittal bridging veins, which are avulsed from the cortical surface and bleed into both the subarachnoid and subdural space.97,98 In primate experiments, an anterior–posterior (sagittal) plane of rotation is the one most likely to result in bridging vein rupture, and a large magnitude of angular deceleration is required.99 Despite the fact that case reports, mostly of older adults in motor vehicle collisions, have documented the occurrence of subdural hemorrhages without contact, in most cases of acute subdural hemorrhage in adults (especially in younger patients), contact is required to create the large angular deceleration forces necessary to rupture cortical bridging veins.3,80,99 Under conditions of lower magnitudes of angular deceleration (i.e., those that involve lower velocities and more gradual deceleration), the parasagittal veins may stretch but do not fail. Contrary to Caffey’s original descriptions, it has been reported that in the majority of cases of inflicted injury in infants and young children, signs of cranial impact are evident with careful radiologic and forensic techniques, including skull fractures and scalp hematomas.24,100–102 When impact forces are dissipated over a wide area against a deformable skull, surface contact injuries may not be evident clinically or radiologically, or contact injury may not occur at all.
A great deal of effort has been expended by persons in the field of child maltreatment to address the question of whether shaking alone can or cannot cause serious injury in infants and young children. This question revolves around the specific mechanism of injury as well as the types and magnitude of forces and the injury threshold necessary for the particular types of injuries seen in cases suspicious for inflicted trauma to occur. There are arguments on both sides of this debate arising from clinical, medicolegal, and biomechanical sources.10,101–109 One factor that clouds the debate arises from the fact that many clinical and autopsy series concluding that shaking has occurred rest on the assumption that the absence of findings of impact necessarily implies that shaking took place. In fact, impact and rapid deceleration both may occur without visible sequelae of direct impact. This fact has been documented in series of children with clear accidental trauma.110
With respect to the magnitude of deceleration, biomechanical studies using anthropomorphic surrogates have shown that shaking alone appears to correlate with relatively small angular deceleration forces in comparison with inflicted impact to the head, with impact causing deceleration 30 to 50 times greater than that caused by vigorous shaking alone.24,103 The forces generated by shaking, when scaled for injury thresholds in young adult nonhuman primates, do not reach the concussion threshold. In contrast, impact events span the range of concussion, subdural hemorrhage, and even diffuse axonal injury.24 Inflicted impact in a recently reported model of a 6-week-old infant was associated with significantly greater angular deceleration than that caused by a fall from 5 feet in which the head struck cement.103
Finally, the question of whether infants and young children have a lower threshold for injury in the context of shaking compared with older children, adults, primates, and other sources of comparison is still under study. Some data from immature large animal models suggest that the threshold for axonal injury resulting from angular forces may be lower during immaturity, whereas younger subjects may be more resistant to damage from focal injury and subdural hematoma.111–113
At present, although different opinions exist, it is probably accurate to say that the exact mechanism and threshold necessary to cause any injury to the intracranial contents, as well as the amount and type necessary to cause severe or fatal brain injury, remain incompletely understood. This is particularly true when the contributions of repetitive injury, hypoxic/ischemic insult, and/or cervical spine injury are also taken into account.60,67,78,107,111,114–116 This is not to say, however, that nothing has been learned about mechanisms of injury and the typical sequelae of injury, as will be further discussed below.
Finally, challenges have been raised about whether the presence of subdural hemorrhage necessarily implies a traumatic mechanism or whether subdural bleeding can occur from hypoxic/ischemic stress, coughing, or vomiting.96,117 Although such explanations have been proposed, and some autopsy cases used to explore these possibilities, to date such occurrences do not fully match the types of clinical injuries typically seen in suspected cases of inflicted injury, and these mechanisms have not been found to be associated with subdural hemorrhage in series of children with medical conditions causing repeated coughing or vomiting.118
In acute inflicted injuries, although the questions of which vessels rupture and what mechanisms are required to cause acute subdural hemorrhage are still debated, it seems likely that different mechanisms may be at play in different cases.11,96 Chronic subdural collections are even more problematic with respect to mechanism; the likelihood of a nonaccidental etiology for chronic collections remains a matter of debate, with estimates ranging from 46 to 68%.94,119 In elderly patients with cortical atrophy or children with shunted hydrocephalus, it has been observed that relatively mild blows to the head may result in subdural hemorrhage; it is generally hypothesized that enlargement of the subarachnoid space results in greater stretch of the bridging vessels. However, in children with so-called “benign external hydrocephalus,” in which the subarachnoid spaces are enlarged, subdural hemorrhage appears to occur rarely.64,120 Whether small collections that are minimally symptomatic may predispose to recurrent bleeding, with symptom onset after relatively mild trauma, remains a point of debate in the defense world. However, the frequency with which young children fall repeatedly without catastrophic hemorrhage seems to argue against this “two in a row” explanation for serious brain injuries potentially resulting from low-height falls. The term second impact syndrome is used to describe the rare occurrence of highly morbid or fatal consequences after repeated sports-related contact injuries in adolescents and young adults.121–123 These athletes are found to have subdural hemorrhages and/or severe acute brain swelling accompanied by acute unconsciousness immediately or within minutes of second contact. To date, there is no convincing evidence of a similar phenomenon resulting from low-height falls (less than 3 to 4 feet) in infants and young children.64
One difference between infants and older children and adults is the relative deformability of the infant skull. Thus, other surface vessels besides the parasagittal bridging veins may be stretched or torn during certain kinds of events. Small convexity, posterior fossa, and tentorial subdural hemorrhages may occur during birth, and skull deformation from static loading during crush injuries may lead to collections at these sites.124,125 It has been hypothesized that deformation of the back of the head due to inflicted impact might rupture posterior draining veins, thus accounting for the high frequency of posterior interhemispheric fissure hemorrhages.11 In a series of infants younger than 2 years of age with subdural hemorrhages due to motor vehicle collisions, skull fractures were seen in the majority, and half had other types of parenchymal brain injury and varying levels of depressed consciousness. The subdural collections were seen most commonly along the falx and frontoparietal convexities, and retinal hemorrhages were sometimes seen.126
Other mechanisms that can cause subdural bleeding include contact subdural injuries, which can occur in adults and children from a focal blow over a cortical vessel (▶ Fig. 52.4). Venous epidural hemorrhages, usually associated with fractures, may be indistinguishable from subdural hemorrhages on CT scan. So-called “disappearing subdurals” may occur in children after falls and likely represent focal subarachnoid hemorrhages that are diluted rapidly and resolve over a day or two after injury.84
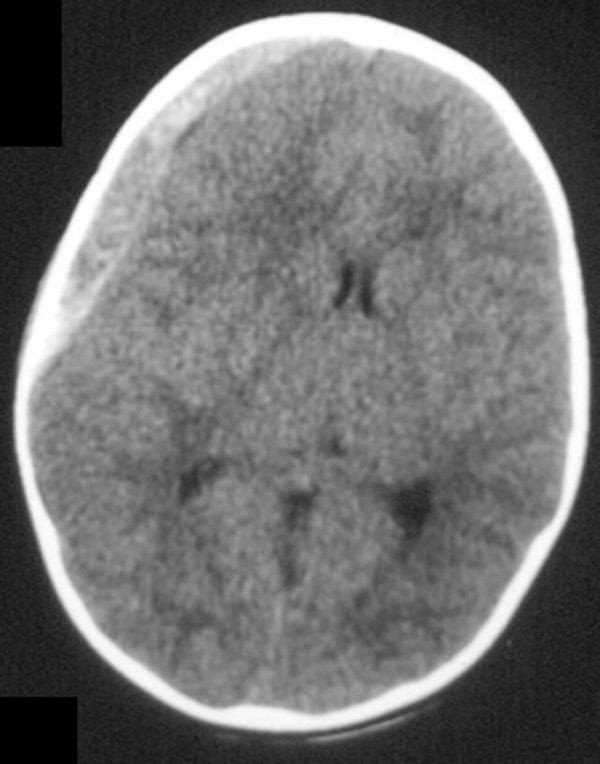
Fig. 52.7 “Contact” subdural injury. This 16-month-old toddler fell from the side of a basement stairway onto cement. She sustained a skull fracture and an underlying torn cortical vessel, resulting in an acute subdural hematoma, and was minimally responsive on presentation. After evacuation of the hematoma, she made a good neurologic recovery.









