♦ Preoperative
Operative Planning
- Review imaging; identify tumor location relative to normal parietooccipital anatomy
- Visual field examination
- Consider using visual functional magnetic resonance imaging (MRI)
- For lesions of the parieto-occipito-temporal junction in the dominant hemisphere (i.e., angular gyrus), cortical mapping may be appropriate
- Plan the craniotomy to provide the shortest possible working distance between the tumor and the surface of the brain
- Measure the tumor in all three major axes and determine which side of tumor is nearest the visual cortex
- Note degree of edema and enhancement pattern of lesion on MRI
- Note presence of calcium or hemorrhage within the lesion on noncontrast computed tomography and MRI
- Note proximity and relation to sagittal and transverse sinus and deep draining veins
- To differentiate between enhancement due to recurrent tumor or enhancement due to radiation necrosis, consider use of specialized imaging of metabolic activity (positron emission tomography scan)
- Neuropsychological testing has been advocated by some experts as a means of delineating subtle deficits not apparent after neurological examination
- Stereotactic set-up may be needed for small, poorly defined lesions in critical regions in neurologically intact patients
- Spinal drain may be needed if there is excessive mass effect, especially if it is necessary to access the interhemispheric fissure
- Operating microscope (optional)
- Mayfield head holder
- Frameless stereotaxy
- Yasargil bar and Greenberg retractors
- Cavitron
Anesthetic Issues
- Communicate degree of intracranial pressure elevation to anesthesiologist
- Arterial line blood pressure monitoring
- Intravenous (IV) antibiotics with skin flora coverage (oxacillin 2 g) should be given 30 minutes prior to incision
- Dexamethasone 10 mg IV prior to incision
- Mannitol (0.5 to 1 mg/kg) for brain relaxation; given prior to turning bone flap to avoid dural tears
- Seizure prophylaxis with phenytoin or phenobarbital
♦ Intraoperative (Fig. 17.1)
Positioning
- Options
- Three-quarters prone: helps the medial occipital lobe fall away, less need for retraction
- The occipital area to be operated lowermost, face toward floor
- Less risk of air embolism
- The occipital area to be operated lowermost, face toward floor
- Lateral position: similar to three-quarters prone approach
- Prone position
- Semisitting position: with neck and back flexion
- Spinal drain may be helpful for brain relaxation and prevention of postoperative cerebrospinal fluid (CSF) leak
- Three-quarters prone: helps the medial occipital lobe fall away, less need for retraction
Minimal Shave
- Use disposable or electric razor
- One-cm margin beyond skin incision
Sterile Prep and Drape
- As for normal craniotomy
Incision
- Large U-shaped incision begun in midline at superior nuchal line, carried along midline, and extended anteriorly to end laterally inferior to the squamosal suture
- It must extend across the midline and below the transverse sinus in certain cases (e.g., torcular meningioma)
< div class='tao-gold-member'>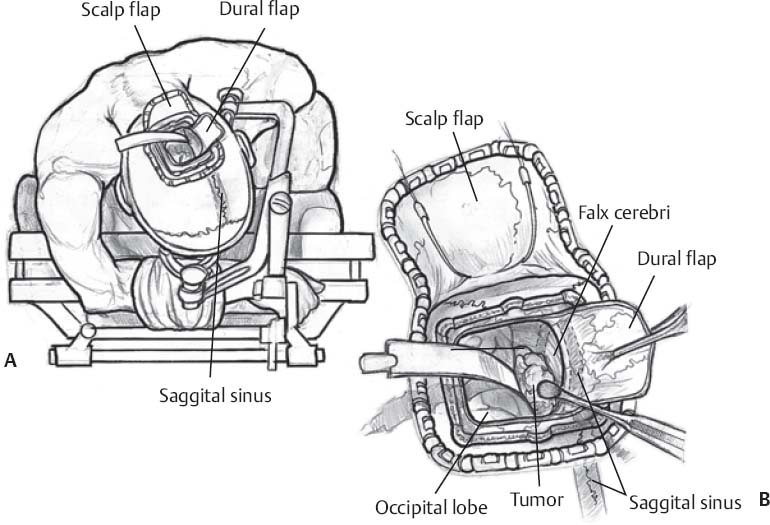 Only gold members can continue reading. Log In or Register to continue
Only gold members can continue reading. Log In or Register to continue
- It must extend across the midline and below the transverse sinus in certain cases (e.g., torcular meningioma)








