Cavernoma location
#
%
Rolandic (39 cases)
7
38
Speech (43 cases)
5
12
Insular (14 cases)
2
14
Visual (9 cases)
1
11
Surgery-related outcome is presented in Tables 2 and 3. As for superficial cavernomas (Fig. 1) (Table 2), 21 cases out of 39 (54 %) operated in the rolandic/perirolandic cortex showed post-operative neurological deficits: in 16 patients the deficit disappeared within 6 months; 5 patients (13 %) developed permanent deficits, 3 of them with a mild disability (mRS 1–2) and 2 with a significant disability (mRS > 3) (as a consequence of previous hemorrhage in one). Only transient deficits were reported in 14 patients operated on in the speech area, mostly lasting for less than 1 month (64 %). After surgery in the visual cortex, in 4 cases (55.5 %) a visual deficit was present transiently and in only one case it was permanent (quadrantopsia).
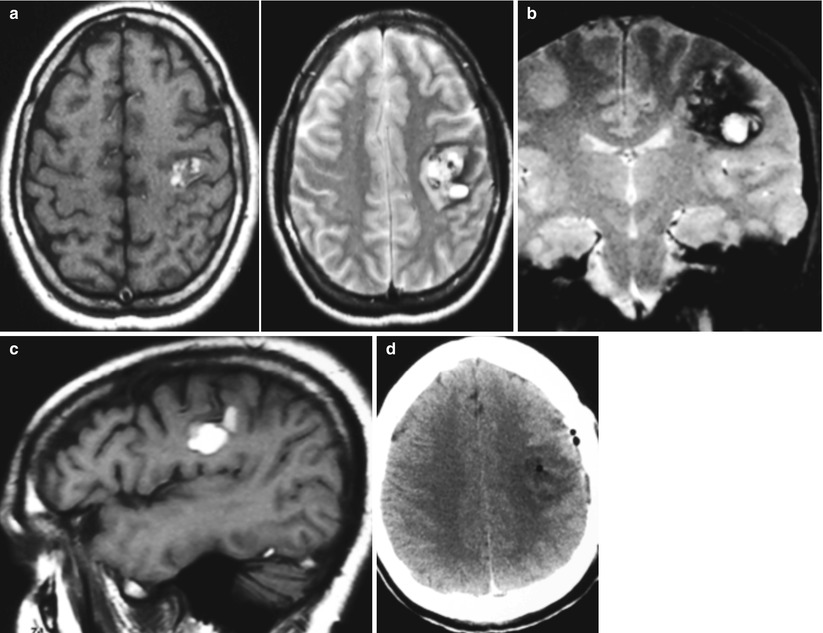
Table 2
Clinical outcome in patients with cavernomas in a superficial location
Transient deficits | Permanent deficits | ||||
|---|---|---|---|---|---|
<1 month | 1–3 months | >3 months | Mild (mRS 1–2) | Significant (mRS ≥ 3) | |
Rolandic (39 cases) | 6 (15 %) | 4 (10 %) | 6 (15 %) | 3 (8 %) | 2a (5 %) |
Speech (43 cases) | 9 (21 %) | 4 (9 %) | 1 (2 %) | – | – |
Visual (9 cases) | 1 (11 %) | 1 (11 %) | 2 (22 %) | 1 (11 %) | – |
Table 3
Clinical outcome in patients with cavernomas in a deep location
Transient deficits | Permanent deficits | ||||
|---|---|---|---|---|---|
<1 month | 1–3 months | >3 months | Mild (mRS 1–2) | Significant (mRS ≥ 3) | |
Insular (14 cases) | 1 (7 %) | 2 (21 %) | 1 (7 %) | 2 (14 %) | 2 (14 %) |
Ventricular (6 cases) | 1 (17 %) | – | – | 2 (33 %) | – |
Basal ganglia (10 cases) | – | 1 (10 %) | – | 6 (60 %) | 2 (20 %) |
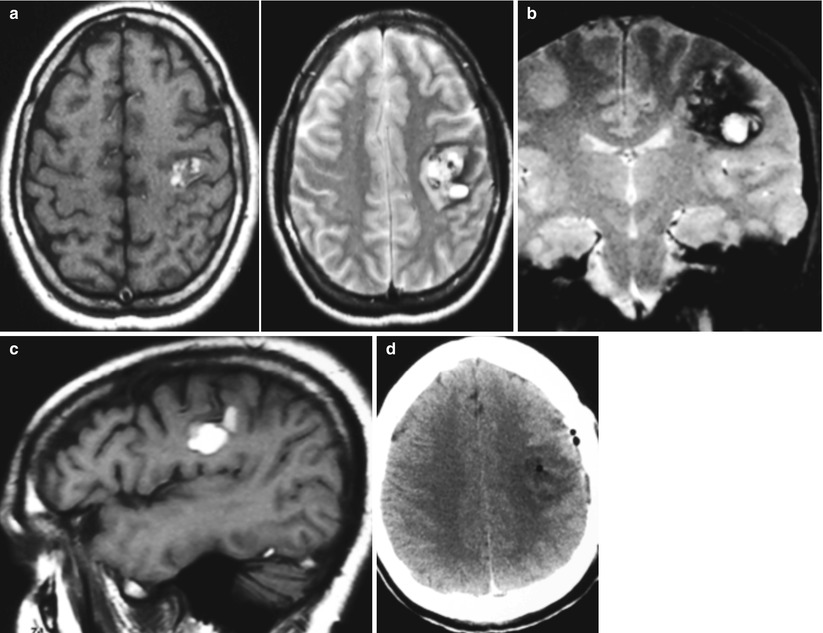
Fig. 1
A 31-year-old man with hemorrhage and left subcortical rolandic cavernoma; (a–c) axial, coronal and sagittal view in T1 and T2 weighted MRI sequences; (d) post-operative CT-scan. The patient experienced a transient hemiparesis
As for deep cavernomas (Table 3), 9 of the 14 patients operated on in the insula (Fig. 2) showed post-operative deficits that were transient in 5 cases (55 %) and permanent in 4 cases, with significant disability (mRS > 3) in 2 patients (22 %). As for intraventricular cavernomas (Fig. 3), 3 cases (50 %) out of 6 patients showed post-operative deficits (2 permanent but not disabling). As for basal ganglia cavernomas, 9 patients (90 %) showed neurological deficits that were transient in 1 case (disappearing within 30 h), mild (mRS 1–2) in 6 cases and disabling (mRS > 3) in 2 cases. Statistically, surgery for superficial lesions carried a lower risk of post-operative deficits as compared to deep lesions (p = 0.02), with a highly significant difference in the incidence of permanent deficits (p < 0.0001).
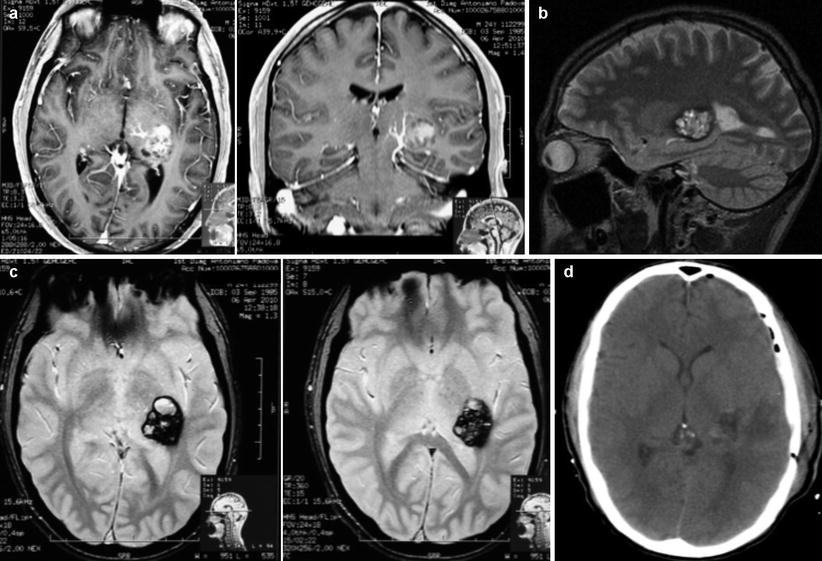
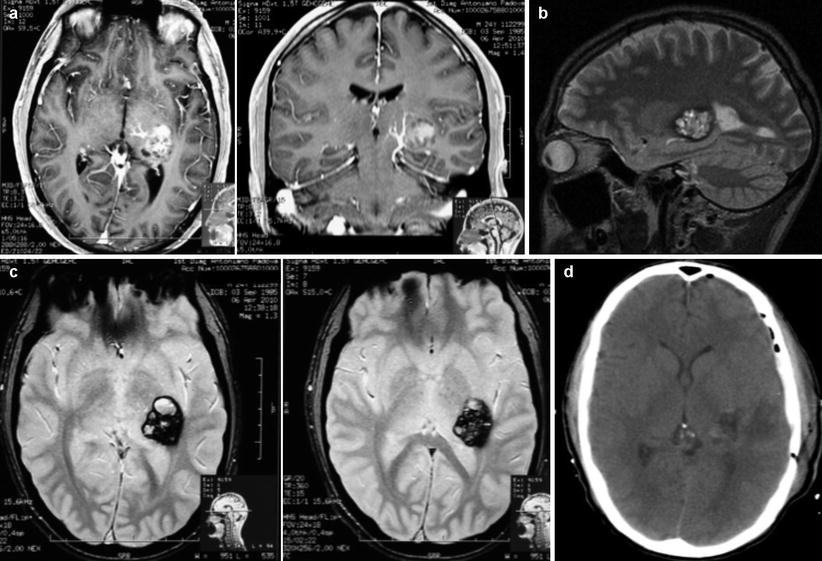
Fig. 2
A 24-year-old man with headache and left posterior insular cavernoma; (a) axial and coronal T1 weighted + Gadolinium MR images, with evidence of a venous anomaly medial to the cavernoma; (b) sagittal view in T2 weighted MR images; (c) axial view in fast spin-echo T2 MR images; (d) post-operative CT-scan. The patient experienced a transient dysphasia, with complete recovery 1 month after surgery
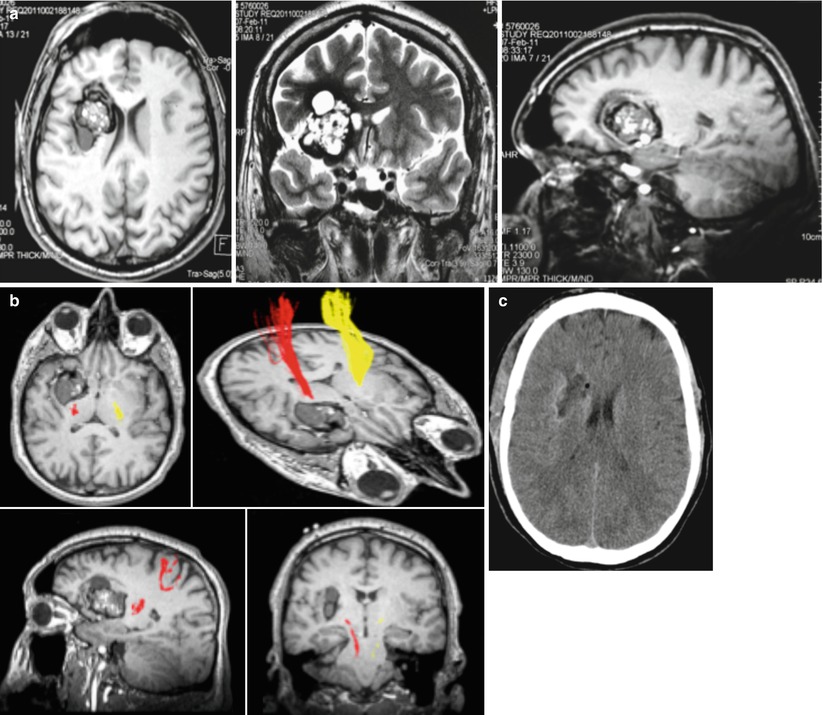
Fig. 3
A 35-year-old man with epilepsy and large right fronto-insulo-caudate cavernoma (with adjacent cystic component); (a) axial, coronal, sagittal view in T2 weighted MR images; (b) reconstruction of the pyramidal tract (DTI); (c) post-operative CT-scan. The patient experienced a transient left hemiparesis (<30 h) and exhibited no deficits at discharge
Epilepsy at follow-up is presented in Table 4, according to the Maraire scale [16]; as a whole, favorable results (Maraire 0) were observed in 44 % of cases, with no seizures and no therapy at follow-up. Moreover, of 15 patients with early post-operative seizures, 13 were seizure-free without therapy at follow-up.
Table 4
Epilepsy at follow-up, in 77 patients presenting with epilepsy
Location | Maraire grade | |||
|---|---|---|---|---|
0 | 1 | 2 | 3 | |
Rolandic (34 cases) | 10 (29 %) | 23 (68 %) | 1 (3 %) | – |
Speech (28 cases) | 16 (57 %) | 12 (43 %) | – | – |
Visual (3 cases) | 1 (33 %) | 2 (67 %) | – | – |
Insular (7 cases) | 4 (57 %) | 3 (43 %) | – | – |
Basal ganglia (5 cases) | 3 (60 %) | 2 (40 %) | –
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

| |





