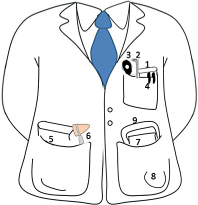
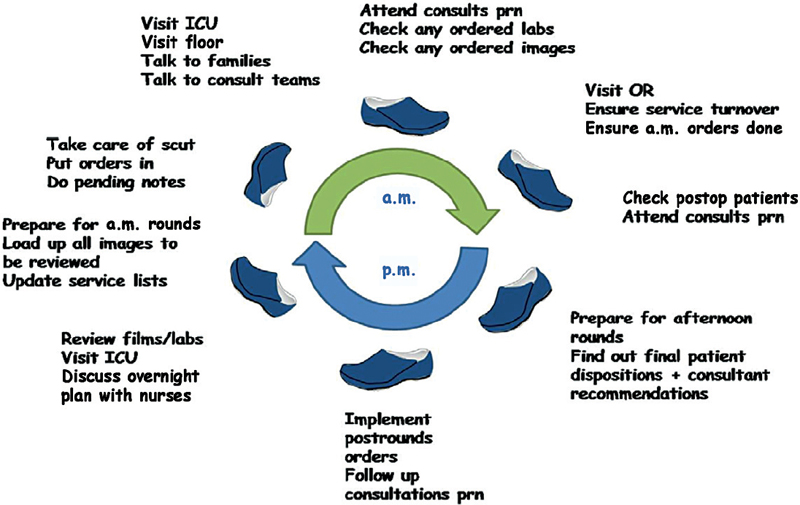
12 As a neurosurgery student on call, what should I carry in my pocket? Fig. 12.1 The nine items an on-call student should carry (see text for itemized list). Top left pocket: 1. Pocket pharmacopoeia 2. Penlight 3. Ophthalmoscope (optional) 4. Two or three pens Right bottom pocket: 5. A handbook related to neurosurgery 6. Reflex hammer Left bottom pocket: 7. Gauze 8. Tape 9. Suture removal kit (optional) Also, make sure you have a stethoscope, tuning fork and/or tongue blades handy. What are some basic principles that apply to the neurosurgery student on call? 1. Try to help the on-call person with as much “scut” as you can: drains, EVDs, changing dressings, finding films, etc. 2. If seeing consults, evaluate all aspects of the patient and present succinctly. 3. Be always accessible and willing to help. 4. Have an inquisitive mind but don’t ask questions you can easily access yourself. 5. If your upper level resident is awake, you are awake. 6. If the resident rests, you read, study, or prepare next day cases when free. 7. If you go to the OR, be sure to help position and help with Foley and lines, throughout the case. 8. Check all postop patients. What are the 10 rules of on-call duty neurosurgery resident? 1. Ensure you get a good sign-out from the morning rounds and a clear goal for each patient. 2. Start taking care of “scut” and orders ASAP. 3. See the patients, talk to the nurses. Examine all the patients. Maintain contact with all hospital sections where you have patients, walk between morning and evening rounds to see how patients are doing. 4. All consults should be seen promptly. Never refuse or complain about it. 5. Go to the OR at least once to check on the progress of surgeries and offer to help assist in closing, moving the patient to recovery, and writing postop orders. 6. Do postop checks and find out if any untoward events occurred in surgery. 7. Have a “YES” policy for transfers so long as they are stable for such transfer. A “NO” attitude will be detrimental for relationships with the vicinity referring physicians. 8. Maintain upper levels and staff updated according to their preference (some prefer not to be contacted unless there is an emergency, but others like regular updates). 9. Your pager is to be answered promptly. 10. Give a good sign-out to the person receiving call from you. Don’t leave a “dirty pager.” How should you manage your time? Follow the steps indicated above that will make your time more efficient. 1. Have paper order sets ready for admissions or develop computer sets (if computerized system). Keep them handy. 2. Have consents handy. 3. Follow a “circular station pattern” while on call. Time management can be challenging. As soon as you are getting ready to do something, a page may interrupt both your train of thought and your current activity. Don’t get distressed or angry. Answer the page, resume your course, and prioritize. What is the “circular station pattern” of rounds?” While on call, there are several “stations” you have to cover (e.g., seeing patients, checking laboratories, talking to families, etc.). While moving forward, you should keep a constant mindset to check on the pending results and exams that need to be checked. Fig. 12.2 Example of a possible day of on-duty call with sample tasks to consider during different times of the day. How do I know how to prioritize? Everything seems equally important! This is a learning process. Not everything is equally important. Things also take longer when you are a junior resident, and you will gain in efficiency as you move along in residency. 1. Situations requiring active medical decisions and actions go first. If you are faced with multiple emergencies at the same time, you will have to move fast (e.g., OPERCON 1). At that time, documentation becomes secondary, although the minimum acceptable has to be accomplished. In other words, you can do your notes later. Take care of issues first. Talking to the referring team will avoid getting paged on “what are your plans” with the consult, if you have spoken with them. Talk to the nurses too! 2. Disposition of current patients to assist in the flow of service is important as well. Keep your cool. Put yourself above and look down to the situation. Then proceed with the lifesaving actions and then the less serious injuries. Remember the acronym ACLS: Act promptly (implement actions quickly). Communicate effectively (with all involved); ask for help from a fellow resident if the situation requires it. Lead on the care of the patients. Safety first (primum non nocere). Stabilize. What are the general rules of consults? First, serve the patient’s needs. Answer the question that is being asked regarding the patient’s care as well as you can. Second, create a good “referral pattern.” Make the referring teams like your promptness and efficiency in caring for the consults. Communicate with them. Third, never refuse to see a consult. Some tips? Say “Yes”; have a positive attitude. As you are talking to the referring team, you may pull up films to make decisions and possibly implement some orders.
On-Call Skills
12.1 On-Call Students
12.2 On-Call Residents
12.3 Consults
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







