CHAPTER 23 OPTIC NEUROPATHIES
Virtually every pathological process that can damage an organ in the body can damage the optic nerve. Thus, optic neuropathies can be produced by ischemia, inflammation, infection, compression, infiltration, toxic exposure, metabolic dysfunction, and trauma. Unfortunately, regardless of the cause of an acute optic neuropathy, the optic disc—the only portion of the optic nerve that can be observed with an ophthalmoscope—has only two possible appearances: swollen or normal. Even more confusing is that with chronic damage to the optic nerve, the optic disc simply becomes pale. Thus, the determination of the cause of an optic neuropathy usually cannot be made from the appearance of the optic disc alone. It can, however, be made from a complete assessment, including a complete history, a complete examination, and, in many cases, appropriate ancillary studies.
OPTIC DISC SWELLING WITHOUT VISUAL LOSS
The most common cause of optic disc swelling without visual loss is papilledema. Papilledema is defined as optic disc swelling caused by increased intracranial pressure.1 It may be produced by an intracranial mass, by blockage of the arachnoid villi by blood or protein (e.g., after a subarachnoid hemorrhage or from a spinal cord tumor), by obstruction of flow of cerebrospinal fluid through the ventricles, and by decreased flow of venous blood through dural sinuses.
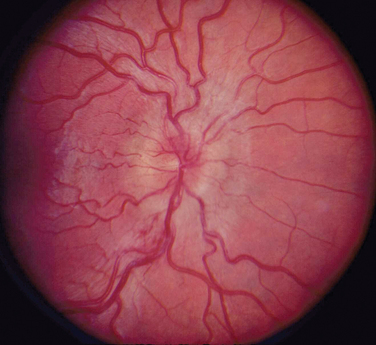
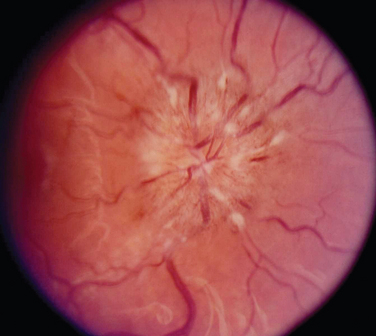
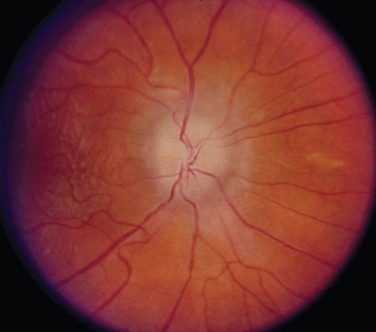
The appearance of papilledema varies with its severity. Early papilledema is characterized by mild swelling and hyperemia of the optic discs (Fig. 23-1). There are often no hemorrhages, and the retinal veins are not dilated. Visual function is usually normal at this time. As papilledema worsens, the disc becomes increasingly swollen and hyperemic, the vessels on the surface of the disc become obscured by the swollen tissue, and peripapillary flame-shaped hemorrhages may appear (Fig. 23-2). Patients with this fully developed papilledema continue to have normal visual acuity and color vision; however, their blind spots are enlarged, and they may have some mild, nonspecific field defects. If intracranial pressure is not lowered, chronic papilledema develops, characterized by a rounding up of the discs, which begin to become pale (Fig. 23-3). During this time, the hemorrhages resolve. The visual acuity may be slightly decreased, but the main visual finding is significant constriction of the visual field. The final stage of papilledema—atrophic papilledema—occurs when the swelling resolves as nerve fibers die, and the optic discs become pallid (Fig. 23-4). At this point, the visual acuity is reduced, and the visual field is markedly constricted, often to only 5 degrees or less.
SUDDEN VISUAL LOSS WITH AND WITHOUT OPTIC DISC SWELLING
Acute Optic Neuritis
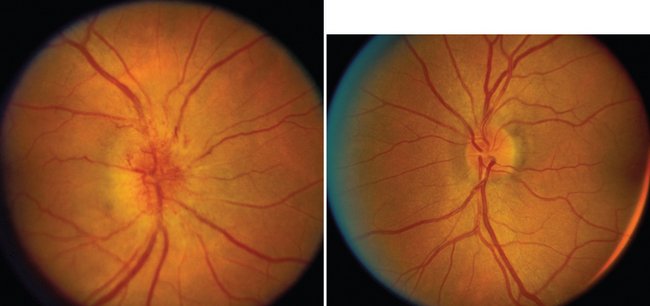
Most patients with optic neuritis are women between 25 and 45 years of age, although this condition can also develop in children and older patients. Optic neuritis is characterized in more than 95% of cases by the sudden onset of pain, often quite severe, behind or around the eye, followed shortly thereafter by decreased central vision and, in many cases, by central field loss.2 The loss of central vision is variable. It may be extremely mild or quite severe; indeed, in some cases, all vision is lost. Affected patients have decreased color vision that may be worse than the acuity would suggest. A relative afferent pupillary defect is always present unless the patient has experienced a previous attack of optic neuritis or has some other optic neuropathy in the opposite eye or the acute process is bilateral. The affected optic disc appears normal in about two thirds of cases; in the other one third, it is swollen (Fig. 23-5).
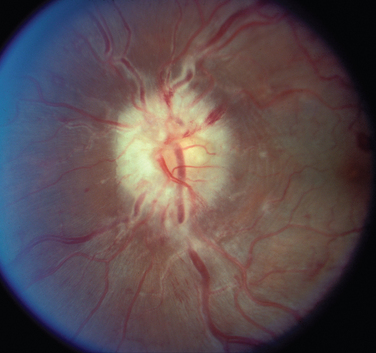
Figure 23-5 Acute optic neuritis. Note swelling of optic disc associated with perivascular sheathing.
Most cases of optic neuritis are idiopathic or demyelinating in origin; however, rare cases are caused by such inflammatory or infectious conditions as sarcoid, syphilis, Lyme disease, and cat-scratch disease.2
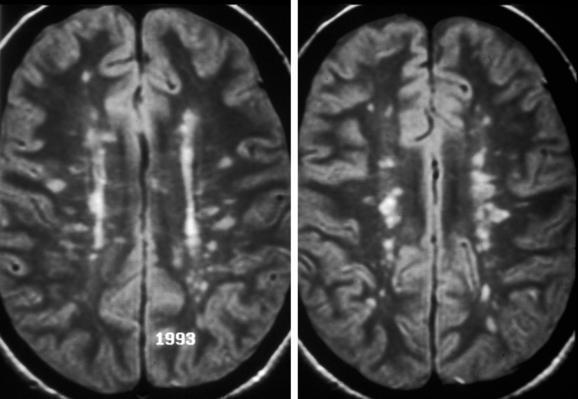
Patients who experience an attack of acute optic neuritis have an increased risk of developing multiple sclerosis, depending in large part on whether white-matter lesions are visible on magnetic resonance images at the time of the acute attack (Fig. 23-6). The presence of even one lesion doubles a patient’s risk of developing multiple sclerosis over the subsequent 10 years.3 Fortunately, there is evidence that the use of interferon β-1a reduces the risk of developing multiple sclerosis in these patients.4
Patients who experience an attack of optic neuritis in one eye have a 10% to 20% risk of developing a similar event in the opposite eye.2 Risk factors for second-eye involvement include white-matter lesions on magnetic resonance images, a family history of multiple sclerosis, and neurological symptoms.
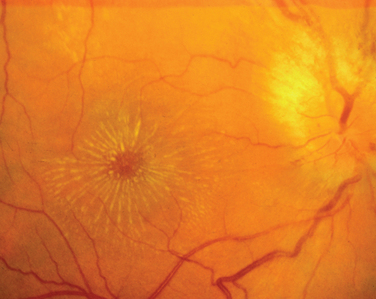
A variant of optic neuritis that has a very different prognosis from the demyelinating or idiopathic form is neuroretinitis.5 This condition begins as an apparently straightforward anterior optic neuritis in which vitreous cells may or may not be present; however, within 1 to 3 weeks, a macular star develops that often persists after the optic disc swelling resolves (Fig. 23-7). Neuroretinitis may be caused by cat-scratch disease, sarcoid, syphilis, tuberculosis, or Lyme disease; however, it is never caused by multiple sclerosis.
Ischemic Optic Neuropathy
The second major cause of acute visual loss with and without optic disc swelling is ION.6 This condition occurs in three main settings: (1) as a complication of systemic noninflammatory vascular diseases, such as diabetes mellitus, hypertension, and hypercholesterolemia; (2) in the perioperative period, most often after cardiac surgery or back surgery in the prone position; and (3) as a complication of vasculitis, most often temporal (giant cell) arteritis.
Nonarteritic ION may be of the anterior or the retrobulbar variety.7 In anterior ION, which constitutes about 90% of all cases, the optic disc is usually hyperemic, and peripapillary flame-shaped hemorrhages are often present (Fig. 23-8); however, soft exudates (cotton-wool spots) are usually absent. The opposite optic disc is almost always small with little or no cup (see Fig. 23-8), and this morphological anomaly is believed to predispose the nerve to ischemia by causing crowding of the optic nerve axons. Patients with retrobulbar ION have a normal-appearing optic disc. Because this condition is rare in comparison with anterior ION, retrobulbar ION should be considered a diagnosis of exclusion: that is, other causes of retrobulbar optic neuropathy, particularly an intracranial mass, should be considered.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree