Fig. 47.1
Venous sinus thrombosis associated with oral contraceptive use. Axial noncontrast CT image (a) shows hyperattenuation of the internal cerebral veins and straight sinus (arrows). The corresponding T2*GRE MRI (b) shows susceptibility effect within these venous structures (arrows). The FLAIR image (c) shows edema in the bilateral deep gray matter and periventricular white matter. Time-of-flight MRA (d) shows absent flow-related enhancement of the internal cerebral veins and straight sinus (arrows)
On MRI, acute thrombus appears as isointense to the brain parenchyma on T1-weighted sequences, while subacute thrombus will appear hyperintense. On T2-weighted sequences, acute thrombus appears as hypointense, while subacute to chronic thrombus appears as hyperintense. T2* or gradient echo (GRE) sequences demonstrate blooming and can increase the conspicuity of thrombus; however, susceptibility weighting (SWI) is not useful for the evaluation of sinus thrombosis (Fig. 47.1). FLAIR and diffusion-weighted (DWI) sequences are useful for the evaluation of associated brain parenchymal abnormalities, such as venous infarction or edema (Fig. 47.1).
Absence of flow-related signal on a time-of-flight MR venogram (MRV) is suggestive of thrombosis. Gadolinium-enhanced MRV can be performed for confirmation, demonstrating the “empty delta sign” with dural enhancement surrounding a non-enhancing thrombus. One must be cautious not to misinterpret subacute hyperintense thrombus on T1-weighted contrast-enhanced MRV. Other potential pitfalls on gadolinium-enhanced MRV include the enhancement or recanalization of chronic thrombus. Cerebral angiography can be performed for confirmation in equivocal cases.
47.4 Differential Diagnosis
There are numerous other causes of venous sinus thrombosis, including other pharmaceuticals, such as l-asparaginase (refer to Chap. 20); malignancy; pregnancy; infections; disorders of coagulation, such as factor V deficiency; granulomatous diseases; connective tissue disorders; dehydration; trauma; and surgery. In addition, several conditions can also mimic the appearance of venous sinus thrombosis on imaging.
Dehydration and polycythemia: In addition to predisposing to venous sinus thrombosis, these conditions can also mimic the appearance of thrombosis on imaging. For example, there is hyperattenuation of the venous sinuses on CT in a patient with elevated hematocrit (Fig. 47.2). This effect is particularly pronounced in pediatric patients, who have a high relative attenuation of the dural sinuses compared to the brain parenchyma secondary to stage of myelination. Certainly, infants are not expected to be on oral contraceptives!
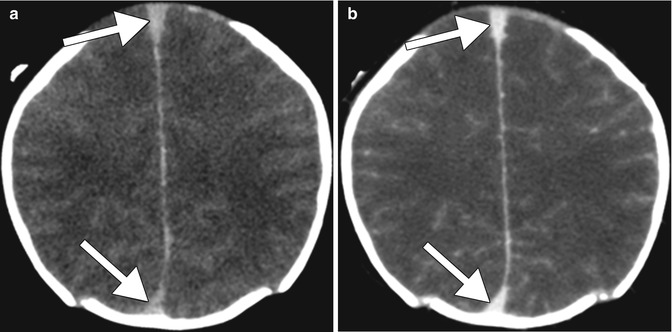
Fig. 47.2
Polycythemia. Axial noncontrast CT (a) shows markedly hyperattenuating superior sagittal sinus contents (arrows). The corresponding CTV (b) shows normal opacification of the venous sinuses (arrows)
Dural sinus hypoplasia/aplasia: Congenitally absent or hypoplastic dural venous sinuses can occur, with hypoplasia/aplasia of the transverse sinuses seen in up to 20 % of patients on time-of-flight venography (Fig. 47.3). In addition, the combined effect of slow flow within a diminutive venous sinus may be mistaken for acute thrombosis. Evaluation of collateral venous pathways or the size of the ipsilateral jugular foramen may be useful when considering a case with hypoplastic or aplastic dural sinuses. Apparent discontinuity of flow on maximum intensity projection (MIP) images should be evaluated on the source images in order to exclude the presence of hypoplastic or aplastic sinus anatomic variants.