Psychiatric symptoms may result from underlying organic disorders, which must therefore be excluded.
DELIRIUM
Delirium is characterized by acute generalized psychological dysfunction that usually fluctuates in degree.
Clinical features
The clinical features of delirium are shown in Figure 3.1. Prodromal symptoms include:
• Perplexity
• Agitation
• Hypersensitivity to light and sound.
 |
| Figure 3.1 (With permission from Puri BK, Laking PJ, Treasaden IH 2002 Textbook of psychiatry. Churchill Livingstone, Edinburgh.) |
Features of delirium itself include:
• Impairment of consciousness – the level of consciousness fluctuates, often being worse at night
• Mood changes – the patient may be anxious, perplexed, agitated or depressed, with a labile affect
• Abnormal perceptions – transient illusions and visual, auditory and tactile hallucinations may occur
• Cognitive impairment – disorientation in time and place, poor concentration, and impaired new learning, registration, retention and recall, may all occur. Language disturbance may also occur
• Temporal course – the disturbance develops over a short period (usually hours to days), and tends to fluctuate.
Epidemiology
Aetiology
Delirium can result from poisoning, psychoactive substance use withdrawal, intracranial causes, endocrinopathies, metabolic disorders, systemic infections and postoperatively. Details are shown in Table 3.1. This is an appropriate place to consider briefly the more important clinical features of some of these endocrinopathies, particularly those that often present with psychiatric symptoms other than delirium.
| Drugs and alcohol | Drug toxicity, industrial poisons, carbon monoxide poisoning, and drug and alcohol withdrawal |
| Intracranial causes | Encephalitis, meningitis, head injury, subarachnoid haemorrhage, space-occupying lesions, epilepsy and postictal states |
| Endocrine disorders | Primary hypoadrenalism (Addison’s disease), Cushing’s syndrome, hyperinsulinism, hypothyroidism, hyperthyroidism, hypopituitarism, hypoparathyroidism and hyperparathyroidism |
| Metabolic disorders | Hepatic failure, renal failure, respiratory failure, cardiac failure, pancreatic failure, hypoxia, hypoglycaemia, fluid and electrolyte imbalance, carcinoid syndrome, porphyria, and deficiency of thiamine, nicotinic acid, folate and vitamin B12 |
| Systemic infections | |
| Postoperative states |
Primary hypoadrenalism (Addison’s disease)
In this relatively uncommon endocrine disorder there is destruction of adrenal cortex, leading to reduced production of glucocorticoids, mineralocorticoids and sex steroids. The condition often presents with symptoms similar to those that occur in depression, including weakness, tiredness, weight loss, depressed mood and anorexia. The important clinical features are shown in Figure 3.2.
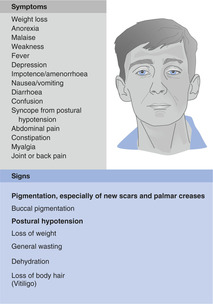 |
| Figure 3.2 (With permission from Kumar P, Clark M (eds) 2005 Kumar and Clark Clinical Medicine, 6th edn. WB Saunders, Edinburgh.) |
Cushing’s syndrome
This describes the clinical state of increased free circulating glucocorticoid and occurs most commonly following the administration of synthetic steroids. Causes include:
• Glucocorticoid administration
• Pituitary-dependent (Cushing’s disease)
• Ectopic adrenocorticotrophic hormone (ACTH)-producing tumours
• ACTH administration
• Adrenal adenomas
• Adrenal carcinomas
• Alcohol-induced pseudo-Cushing’s syndrome.
Cushing’s syndrome may present with symptoms similar to those seen in depression, mania and schizophrenia (including mood changes, delusions, hallucinations and thought disorder). The important clinical features are shown in Figure 3.3.
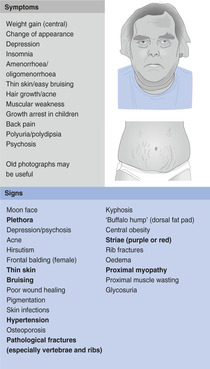 |
| Figure 3.3 (With permission from Kumar P, Clark M (eds) 2005 Kumar and Clark Clinical medicine, 6th edn. WB Saunders, Edinburgh.) |
Hypothyroidism
This is one of the commonest endocrine disorders (particularly in women). Causes include:
• Congenital causes – agenesis; ectopic thyroid remnants
• Atrophic thyroiditis
• Hashimoto’s thyroiditis
• Iodine deficiency
• Dyshormonogenesis
• Antithyroid drugs
• Other drugs – lithium; amiodarone; interferon
• Postinfective thyroiditis
• Post-surgery
• Post-irradiation
• Radioiodine therapy
• Tumour infiltration
• Peripheral resistance to thyroid hormone
• Secondary hypopituitarism.
Hypothyroidism may present with symptoms similar to those seen in depression, mania and schizophrenia (myxoedema madness). The important clinical features are shown in Figure 3.4. Note that these features may not be seen in children and young women. The former often have slowed growth and perform poorly at school; pubertal development may be arrested.
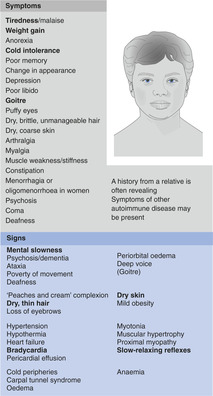 |
| Figure 3.4 (With permission from Kumar P, Clark M (eds) 2005 Kumar and Clark Clinical medicine, 6th edn. WB Saunders, Edinburgh.) |
This condition should be excluded in any young non-pregnant, non-postpartum woman presenting with:
• Oligomenorrhoea
• Amenorrhoea
• Menorrhagia
• Infertility
• Hyperprolactinaemia (manifesting, for example, with lactation).
Note also that the clinical features of hypothyroidism may be difficult to recognize in the elderly, as some of them are similar to those that occur with normal ageing.
Hyperthyroidism
This is also one of the commonest endocrine disorders (particularly in women). Causes include:
• Graves’ disease
• Toxic solitary adenoma/nodule (Plummer’s disease)
• Toxic multinodular goitre
• De Quervain’s thyroiditis
• Postpartum thyroiditis
• Thyrotoxicosis factitia
• Exogenous iodine
• Drugs – amiodarone
• Metastatic differentiated thyroid carcinoma
• Thyroid-stimulating hormone (TSH)-secreting tumours
• Human chorionic gonadotrophin (HCG)-secreting tumours
• Ovarian teratoma.
Hyperthyroidism may present with symptoms similar to those seen in mood disorders, panic disorder, generalized anxiety disorder and, in children, attention-deficit hyperactivity disorder (behavioural problems such as hyperactivity). The important clinical features are shown in Figure 3.5. Note that these features may not be seen in children, in whom the disorder may instead manifest as excessive growth or behavioural problems.
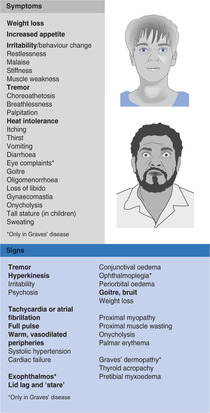 |
Figure 3.5
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|




