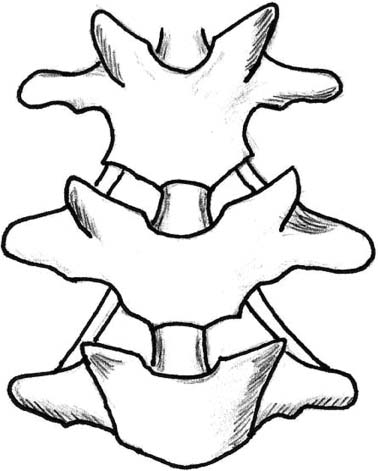
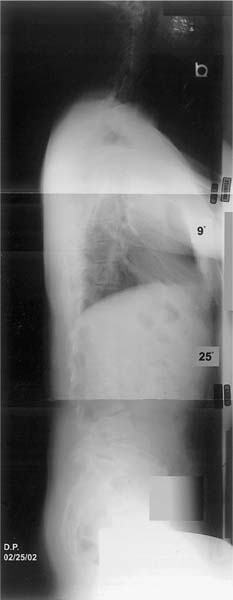
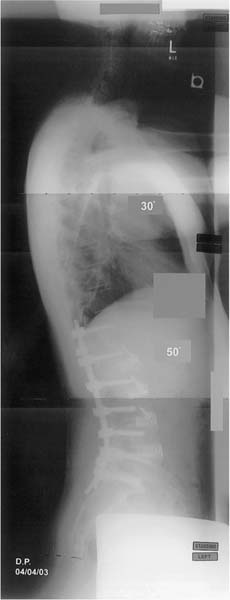
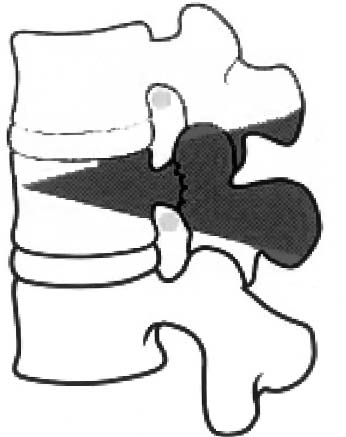
Chapter 22 The decompensated spine, either in coronal, sagittal, or both planes, remains a challenge to the spinal surgeon when symptomatic and meriting treatment. Risks, benefits, and the patient’s expectations should be considered before attempting any reconstruction procedure. Important milestones in the surgical treatment of complex spine deformity were the introduction of spinal osteotomy techniques and the use of instrumentation in spine fusion. In 1945, Smith-Petersen et al.1 first performed a wedge osteotomy in the lumbar spine. Lichtblau and Wilson2 were first to use instrumentation for the fixation. Mason et al.3 and Urist4 in the 1950s also introduced the cervical spine osteotomy. For the purpose of this chapter, complex spine deformity is characterized by multiplanar spine deformity with one or more features of scoliosis, kyphosis, or lordosis resulting in spinal imbalance that lacks flexibility between the vertebrae and cannot be balanced with manipulation of soft tissue but requires a form of bony resection/osteotomy to restore physiologic global and segmental spinal balance. Such deformities can be analyzed in two arbitrary categories: (1) predominantly sagittal imbalance and (2) multiplanar deformity with coronal and sagittal imbalance. To benefit from these physiologically demanding surgeries, the patients have to be physiologically young and without substantial medical comorbidities. Careful consideration should be made for the older patients who are subjected to such complex procedures because of a high incidence of pseudarthrosis and other postoperative complications. Careful history and clinical examination are necessary to select patients appropriately for the procedures, identify underlying comorbidities, and to assess the overall appearance and balance of the patient. This is done in conjunction with radiographic studies to assess the most suitable osteotomy site and the flexibility of the deformity and to provide a basic differential diagnosis and treatment plan. A multidisciplinary approach is necessary to obtain preoperative clearance as needed from medicine, cardiopulmonary, and neurology specialists. Imaging studies include plain standing anteroposterior and lateral radiographs. On the lateral x-ray, sagittal imbalance (SI) is determined with the patient standing fully erect with hips and knees in extension and the arms supported horizontally on an intravenous pole. A plumb line is dropped from C7 to S1 and the horizontal distance from the posterior corner of the L5-S1 disk to this line is measured to represent the sagittal vertical axis (SVA). Frontal balance is determined on the anteroposterior radiograph by measuring the distance from the center of the sacrum to a plumb line that is dropped from the center of the seventh cervical vertebra. Overextension over a bolster at the apex of the kyphotic deformity and lateral bending films are necessary to estimate the rigidity of the deformity. If spondylolisthesis is suspected, flexion-extension lateral radiographs should be obtained. Computed tomography (CT) is useful to estimate the integrity of a fusion mass. Magnetic resonance imaging (MRI) would assess both the neurologic structures and the vertebrae in cases of possible infection; if MRI is contraindicated, a myelo-CT scan can be obtained to evaluate the neural canal. Finally, in older patients, the bone mineral density should be assessed. In the upright posture, the spinal column develops normal sagittal curves that tend to balance to position the head directly over the pelvis. There is considerable variation in the normal range of values for lumbar lordosis and thoracic kyphosis, therefore the absolute value is not as important as the overall sagittal balance of the spine.5 This is best reflected by measurement of the distance from the sacrum to a plumb line that is dropped from the center of the seventh cervical vertebra6 and has a normal range of ±2 cm. Absolute values are used for estimation of required correction, and rule of thumb is that the patient has to have at least 30 degrees more lumbar lordosis than thoracic kyphosis.7 Sagittal imbalance is also classified in two types: Type I represents a hypolordotic or kyphotic lumbar segment, whereby the patient compensates by hyperextension of the thoracic spine and remains in balance. Type II deformity is characterized by global imbalance, whereby the spine is flat due to loss of segmental lordosis or kyphosis and the patient is out of balance and unable to compensate; the plumb line falls in front of the S1 superior end plate.8 Until the evolution of spinal instrumentation, systemic diseases, mainly ankylosing spondylitis, were the most common cause of fixed sagittal deformity.9–17 Nevertheless, the iatrogenic flat-back syndrome is currently more often encountered, mainly because the patients treated for scoliosis in the 1960s and 1970s with Harrington distraction instrumentation are now becoming symptomatic. The syndrome was first recognized in 1973 by Doherty18 who recognized the reduction of the physiological lumbar lordosis (flat back) and the subsequent development of sagittal imbalance. Patients are unable to maintain the erect position without hip and knee flexion. This results in back pain, generalized to the lumbar and thoracolumbar spine, and fatigue that develops as the day proceeds. Cervical pain may develop from exacerbation of the cervical lordosis in the patient’s effort to assume a horizontal visual field; thigh and knee pain develop from the quadriceps muscle strain.19 These patients who were treated with distraction Harrington instrumentation to the lower lumbar spine and sacrum6,19–21 were able to compensate for the loss of lumbar lordosis during adolescence and young adult age. Later, reduced muscle strength, adjacent disk degeneration, and hip and pelvic disease all combine to decrease the patient’s ability to compensate and may result in increase disability.19 The same effect in the lumbar spine is also associated with the use of anterior compression instrumentation (Dwyer or Zielke) without structural inter-body grafting that shortens the anterior column.8 Iatrogenic fixed sagittal imbalance may also result from pullout of posterior segmental spinal instrumentation or settling of anterior spinal column long fusion done without structural grafting. Vertebral fractures, either osteoporotic or traumatic, can either heal naturally or be surgically fused in kyphosis. Finally, severe lumbar degeneration may be associated with rigid lumbar kyphosis. Nevertheless, spinal stenosis usually coexists with lumbar kyphosis after a posterior fusion associated with either adjacent level breakdown or an area of pseudarthrosis within the fusion mass.22 Less common causes are neuromuscular, congenital, and infectious conditions.23–26 Conditions not related to the spine, such as hip or knee flexion contractures, can also present with sagittal malalignment and must be ruled out. Lumbar spine osteotomies are the mainstay of treatment in fixed sagittal decompensation secondary to excessive thoracic kyphosis, loss of lumbar lordosis, and combinations of sagittal malalignment. In symptomatic flat-back syndrome, osteotomies should be reserved for the failure of conservative means.8 The goal of the osteotomy is to restore the sagittal balance so the plumb line intersects the posterior superior corner of the S1 vertebra, enabling the patient to resume a more erect posture, restore the horizontal visual field, relieve lung compression by the abdominal viscera, improve diaphragmatic excursion, and, finally, improve appearance. The surgical correction of the kyphosis deformity was first described by Smith-Petersen et al. in 1945.1 Multiple posterior osteotomies were performed after resection of the spinous processes and removal of the edges of the laminae with the ligamentum flavum. They were performed with an osteotome through the synostosed articular processes. This resulted in extension and opening through the disk spaces, rupture of the anterior longitudinal ligament, and elongation of the anterior spine to produce lordosis. La Chapelle27 in 1945 described a two-stage osteotomy with combined approaches. In 1947, Briggs et al.9 reported a posterior wedge osteotomy with bilateral intervertebral foraminotomy. All these procedures as well as various modifications of the Smith-Petersen osteotomy (SPO)9,11,16,27–30 represent a shortening of the posterior column and lengthening of the anterior column with the posterior margin of the intervertebral disk as a pivot of angulation. The elongation of the anterior column has caused major complications, including paraplegia from cauda equina stretching, aortic rupture from stretching of the abdominal aorta, and high intestinal obstruction from tensing the superior mesenteric artery across the duodenum.2,15,29,31–33 Instead of a monosegmental SPO that may produce a dangerous kinking, Hehne et al. had recommended a polysegmental SPO.16 With each SPO, a 10- to 15-degree per segment correction should be expected, ~1 degree of lordosis for each resected millimeter.8,16,34 The disk space must be mobile and of adequate height. Young patients with good bone stock are preferred for the secure anchoring of the segmental instrumentation. In Type I kyphosis, the deformity site determines the osteotomy site. In Type II, it is better to correct the deformity in the lower spine because the lever arm correcting the axis of view is greater and the complication rate is smaller. In addition, in ankylosing spondylitis patients, the correction is not hindered by the fixed ribs.16 The patient should be positioned prone on a four-poster frame and provision of spine extension and hip extension should be made to close the osteotomy site at the end of the operation. Fixation points should be obtained above and below the osteotomy sites. Starting the osteotomy at the interlaminar space, the neural arch is undercut to avoid neural structure compression at the closure of the osteotomy. Extending laterally in a V-shape fashion over the foraminal space both articular processes are excised (Fig. 22–1). After positioning of the rods, a combination of compression and cantilever maneuvers is applied to close the osteotomy sites. SPOs can be performed in conjunction with anterior diskectomies and fusion (Figs. 22–2 and 22–3) or with similar technique over a fusion mass.6,35 Figure 22–1 Technique of Smith-Petersen osteotomy demonstrating the V-shape laminar and facet resection It is critical to identify and spare the pedicle, which in case of no discernible normal anatomy is feasible either by the transverse process visualization or by fluoroscopy. The V-shape of the osteotomy provides rotational control and enhances the segmental interlocking. Caution should be taken when the osteotomy is performed in patients with scoliotic deformity that exceeds 45 degrees because there is a tendency to push the patient off to the concavity. Nevertheless, asymmetrical resection can be done to improve coronal deformities. It should also be avoided in patients with spinal stenosis, especially foraminal stenosis, because the osteotomy decreases the foraminal space.22 A SPO that is not closing suggests the anterior column is stiff; then the only alternative is to perform a pedicle subtraction osteotomy between two adjacent SPOs with resection of the pedicles and the vertebral body between them.36 Transpedicular decancellation of the vertebral bodies was initially described by Michelle and Krudger as a biopsy technique for the diagnosis of vertebral lesions.37 Based on this technique, two original three-column osteotomies were described. Heinig38 introduced the eggshell procedure as a one-stage operation for correction of rigid deformities that permits protection of the neurologic elements and vascular structures. Heinig described removal of the superior end plate and intervertebral disk and fracture of the anterior cortex permitting compression rather than wedge closure. Thomasen modified the osteotomy39 and described a circumferential wedge excision rather than decancellation and compression with vertebral body collapse (Figs. 22–4 and 22–5). Both transpedicular approaches are closing wedge osteotomies with an anterior apex of correction and shortening of the spine rather than elongation. They create a large neural foramen through removal of the pedicles. Because the surfaces of the osteotomy are cancellous bone, they heal rapidly and effectively. Figure 22–2 Preoperative lateral standing radiograph of a 41-year-old patient with lumbar Scheuermann’s kyphosis and sagittal imbalance treated with posterior Smith-Petersen osteotomy (SPO). Pedicle subtraction osteotomy (PSO) consists of removal of cancellous bone of the selected vertebral body through both pedicles to weaken the vertebral body and creation of posterior compression of the laminae and posterior aspect of the vertebral body with minimal force. The posterior arches of the adjacent vertebrae are approximated under direct vision by manipulation of the table, extension of the spine, and cantilever forces on the spine with the instrumentation. Figure 22–3 Postoperative lateral standing radiograph of a 41-year-old patient with lumbar Scheuermann’s kyphosis and sagittal imbalance treated with posterior Smith-Petersen osteotomy (SPO); demonstrates restoration of lordosis and sagittal imbalance. The amount of the correction should be estimated on standing full-length lateral spinal radiographs. Approximately 30 degrees to 50 degrees of correction can be achieved per osteotomy13,17; a 6- to 13.5-cm correction of the SVA is also anticipated.40,41 It can be performed in rotated scoliotic segments, preferably at the apex, which can be corrected if a trapezoidal shape is given to the osteotomy. The osteotomy is best placed at the midlumbar spine to avoid working around the spinal cord and to allow adequate proximal and distal fixation points. If possible, the level has to be parallel to the sacrum to avoid osteotomy translocation at the completion of the procedure. Again, good bone stock is a prerequisite to secure the segmental instrumentation. Ideally, the osteotomy is performed in an area of previous fusion.22,42 If performed through a motion segment, then neither the bone stock nor the stability after the procedure are ideal and may compromise the fusion outcome. Figure 22–4 Pedicle subtraction wedge osteotomy and decancellation of spinal column.
Osteotomies and Vertebral Column Resections for Complex Spinal Deformities
♦ Preoperative Planning and Patient Evaluation
♦ Sagittal Imbalance
Etiology
Indications for Surgical Treatment
Surgical Techniques
Smith-Petersen Osteotomy
Pedicle Subtraction Osteotomy, or Eggshell Osteotomy
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree