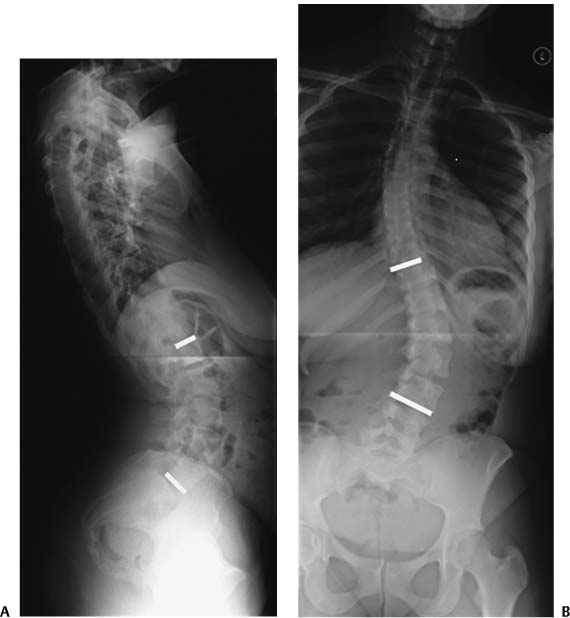
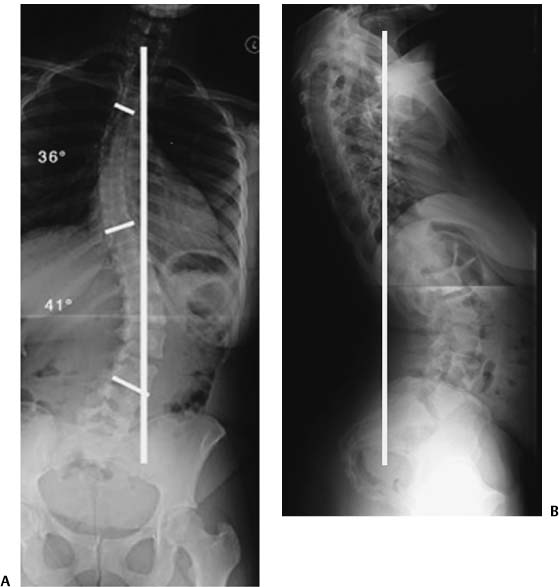
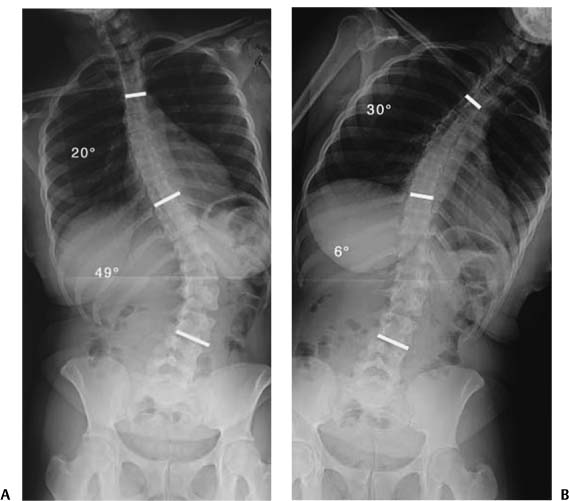
Chapter 1 Spinal deformity is a complex and dynamic process that occurs in both the sagittal and coronal planes of the thoracolumbar spine. Successful treatment is aimed at achieving satisfactory balance in both of these planes. The spinal curvatures in adult deformity differ greatly from those in adolescent deformity. As a general rule, the curves in adults tend to be stiffer, whereas the adolescent curves are more flexible. In addition to cosmetic concerns, adult patients frequently present with pain and neurologic symptoms. Adolescents usually do not have this degree of pain or neurologic symptoms. Deformity surgeries tend to be complex procedures with high rates of operative and perioperative complications. The goals of deformity surgery are to obtain a solid fusion with a balanced spine, to relieve pain, and to prevent further deformity. A secondary goal is to achieve curve correction and in so doing to improve the cosmetic appearance. The first reported record of scoliosis was by Hippocrates. In ancient times, traction was attempted, unsuccessfully, to correct scoliotic deformity. In the 16th century, Ambroise Pare is credited with describing the first use of bracing to treat scoliosis. Pare used an iron corset to attempt to correct coronal plane deformity. In 1962, Harrington reported the first successful use of spinal implants in the correction of scoliosis.1 As such, the modern era of deformity correction with spinal instrumentation began. The Scoliosis Research Society, the oldest formal spine society, was established in 1966. Initially, spinal deformity correction was performed solely by orthopaedic surgeons. The early phases of deformity correction predominantly focused on correction of coronal plane scoliotic curvatures using distraction. Over time, it has become apparent that correcting coronal deformity with pure distractive mechanisms leads to an imbalance in the sagittal plane and the development of “flat-back” deformity.2,3 Spinal deformity consists of coronal plane deformations referred to as scoliosis and sagittal plane deformations that usually result in kyphosis. There is a dynamic process in the interaction between coronal and sagittal plane curvatures. Adult spinal deformity presents as curvatures that were present prior to skeletal maturity, which are termed persistent idiopathic curvatures, and curvatures arising later in life, as a result of degenerative changes.4 As a general rule, larger curves are generally less flexible than smaller curves.5,6 Prior to treating spinal deformity, it is essential to have an understanding of the natural history of untreated spinal curvatures. In a landmark study published by Weinstein and Ponseti, the natural history of scoliotic curvatures was determined with a mean follow-up period of 40 years. These authors determined that 68% of adolescent idiopathic curvatures progressed beyond skeletal maturity. Thoracic curvatures greater than 50 degrees progressed at an average of 1 degree per year, thoracolumbar curves progressed 0.5 degrees per year, and lumbar curves progressed 0.24 degrees per year. Thoracic curvatures of less than 30 degrees tended not to progress.7 Moe and Lonstein have estimated that there are 500,000 adults in the United States with curvatures exceeding 30 degrees.8 Significant differences are present between the curves affecting adolescents and adults. The presenting symptoms in adolescents are typically curve progression and cosmesis rather than pain.5,6,9,10 On the other hand, adults tend to present with pain and neurologic abnormalities. Curve progression and cosmetic issues tend to be less problematic in the adult population.5,6,9,11 In addition, adult patients are more likely to be anxious and depressed regarding their deformity.9 Axial pain and radicular pain are characteristic of adult deformity and much less frequent in adolescents.5,6 Adult deformity tends to be more rigid than curvatures of adolescents, and therefore, the surgical correction of these curves is more difficult.4–6,12 Accordingly, higher complication rates have routinely been reported in the correction of adult deformity.4,6,11 The successful treatment of deformity combined with pain, typically present in adults, is more challenging than the treatment of adolescent patients with idiopathic scoliosis.10 With adult curvatures, due to the rigidity of these curves, there is often the need to perform a release procedure followed by curve correction. Adolescent curvatures, which tend to be more flexible, can often be treated with curve correction procedures from either a single anterior or posterior approach. Whereas bracing may have a role in modifying curve progression in adolescents, there is no therapeutic role for bracing in altering curve progression in adults.11 The etiology of pain produced in adult deformity is a combination of muscle fatigue, trunk imbalance, facet arthropathy, and degenerative disk disease.11 The primary treatment goals of spinal deformity are to halt deformity progression, relieve pain, and improve function. The operative treatment goals include obtaining a solid fusion with a balanced three-dimensional spine as well as to prevent further deformity.10 The amount of curve correction obtained in adult patients is less important than producing a stable, balanced, and pain-free spine.11,12 The ultimate goal in deformity correction is to obtain a balanced spine in both the sagittal and coronal planes. Takahashi et al. compared adult patients over the age of 50 years with younger adult patients. They found that the radiographic results were less satisfactory in the older patients; however, pain relief was more reliable when compared with the younger adults with deformity.6 The surgical treatment of patients with spinal deformity is a major undertaking. Over the past two decades, spine surgeons from the disciplines of both orthopaedic surgery and neurologic surgery have made increasing advances in the evaluation and treatment of patients with spinal deformity. It is important to recognize that some patients with spinal deformity are not fit to undergo the extensive surgery often required for surgical correction. As a result, some patients with spinal deformity are best served with conservative, or palliative, treatment with methods such as exercises, braces, and medications. As with all medical disciplines, a unique set of terms are applicable to spinal deformity. Specific terms are used to describe vertebrae, angles, lines, and curves. The end vertebra is the most cephalad and most caudal vertebra of a curve for the curve’s inflection point (Fig. 1–1). This applies to measurements made in both the coronal and sagittal planes. A neutral vertebra is defined as having symmetric pedicles on a standing posterior/anterior (PA) radiograph (Fig. 1–2). The central sacral line is determined by first drawing a line connecting the superior-most aspects of the iliac crests. A perpendicular drawn from the midpoint of the S1 vertebra superiorly defines the central sacral line. The vertebra that is intersected at its midpoint by the central sacral line is referred to as the stable vertebra (Fig. 1–3). Many surgeons use the concepts of the stable vertebra and the neutral vertebra when determining which level to include in spinal stabilization constructs. Figure 1–1 Demonstration of the end vertebrae of a deformity curve. (A) Sagittal end vertebrae; (B) coronal end vertebrae. Plumb lines are used to determine coronal and sagittal balance. In the coronal plane, a plumb line is drawn from the center of the C7 vertebra to the center of the sacrum in a spine with normal alignment. Emami et al. have defined greater than 25 mm of deviation between C7 and the sacrum as evidence of coronal decompensation.2 In the sagittal plane, a line drawn from the center of the C7 vertebra should intersect the S1 vertebra on a standing 36 lateral radiograph.2,13,14 Because of its readily identifiable location on lateral radiographs Eck et al. have defined sagittal plane variations with respect to the anterior-most aspect of the S1 vertebra.14 Other authors have stated a plumb line from the center portion of the C7 vertebra should intersect the posterior-most aspect of the S1 vertebra.2,13 A deviation of greater than 40 mm has been defined as sagittal decompensation.2 By convention, when the C7 sagittal plumb line is anteriorly displaced, a positive value is assigned. A negative value is given for posterior displacements of the C7 sagittal plumb line (Fig. 1–4). With respect to naming of curves, a structural curve is a curve that does not demonstrate normal mobility on lateral bending radiographs. A nonstructural, or compensatory curve, is a flexible portion of a curve with normal mobility on lateral bending films (Fig. 1–5). This is typically present either above or below a structural curve. In the naming of coronal plane curvatures, the location of the convex portion of the curve determines its name. For example, a curve that has a convexity on the right side may be referred to as a dextroscoliosis, whereas a curve convexity on the left side is a levoscoliosis. Skeletal maturity is that point where no further longitudinal bone growth occurs. This typically occurs during adolescence. Female patients tend to achieve skeletal maturity at an earlier age than male patients. As a general rule, female patients will reliably achieve skeletal maturity by 18 months after the onset of menarche. Numerous grading scales are available for determining skeletal maturity in adolescent patients. Adult deformity refers to curvatures present in patients after skeletal maturity has been achieved. Figure 1–2 Identification of the neutral vertebra in a coronal plane deformity curve. The T10 vertebra is the neutral vertebra (arrow). Figure 1–3 Identification of the central sacral line and the stable vertebra in a coronal plane deformity curve. The T9 vertebra is the stable vertebra (arrow). Figure 1–4 A 29-year-old female with previously untreated scoliosis developed progressive back pain with leaning to her left side. Plumb lines drawn on 36 standing posterior/anterior (PA) and lateral radiographs obtained with the patient’s hips and knees extended. (A) Coronal view shows C7 to be 44 mm to the left of the center of the sacrum; radiograph demonstrates a right thoracic dextroscoliosis (36 degrees) and a left thoracolumbar levoscoliosis (41 degrees). (B) Sagittal view shows the vertical plumb line to be 38 mm dorsal to the posterior aspect of the L5-S1 interspace (by convention, kyphotic angulations are assigned a positive () value and lordotic angulations are assigned a negative () value; this curve measures 38 mm). Figure 1–5 Right and left lateral 36 bending views demonstrate curve flexibility. (A) On right bending, the thoracic dextroscoliosis corrects to 20 degrees (T4 to T10 levels). (B) On left bending, the thoracolumbar levoscoliosis corrects to 6 degrees (T10 to L3 levels). Deformity correction procedures, which relied on pure distractive forces, have been recognized to place the C7 vertebra in a positive sagittal location with respect to the sacrum. Doherty first described this phenomenon as “flat-back” syndrome in 1973.15 Smith has described flat-back syndrome as the symptomatic loss of sagittal plane balance secondary to a loss of normal lumbar lordosis. Symptoms of flat-back syndrome include pain and the need to bend the knees to maintain an upright position.3 In patients with flat-back, a lumbar lordosis of less than 30 degrees will be associated with anterior decompensation of the spine.2 Recognition of this flat-back syndrome has led to the development of segmental instrumentation in an attempt to prevent the development of this painful deformity condition. When sagittal decompensation occurs, there is a need to extend the hips and flex the knees to center the head over the sacrum in a sagittal plane.3,13 Bernhardt and Bridwell analyzed sagittal plane alignment in normal patients without evidence of deformity. They found average values of thoracic kyphosis measure 36 degrees and of lumbar lordosis measure 44 degrees.16 Significant variations do occur among normal, nondeformed, patients. In the lumbar spine, 67% of the total lumbar lordosis occurs at the L4-L5 and L5-S1 levels.16
Overview of Spinal Deformity
♦ Spinal Deformity Terms and Principles
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree