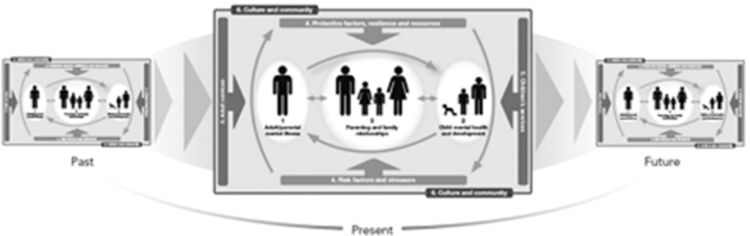
The Family Model (TFM) cross-sectional components
All components must be considered for comprehensive assessment and treatment. The aim of the model is to facilitate an understanding of the processes that underlie and influence how:
Adult/parental mental illness affects children (D(domain)1 → D2).
Mental illness can affect parenting and the parent–child relationship (D1 → D3).
Parenthood can precipitate and influence mental illness (D3 → D1).
Children’s mental health and developmental needs have an impact on parental mental health (D2 → D1) and on parenting and the parent–child relationship (D2 → D3).
Both risk and protective factors interact with parental mental illness, with child development and mental health, with parenting and the parent–child relationship, and with each other in a multidirectional manner (D4 and D1–3 and D4).
Service quality, access, and so on affect identification of families, assessment, and intervention and hence influence parental mental illness, child development and mental health, and parenting and the parent–child relationship, as well as a range of proximal and distal risk and protective factors (including culture and community networks) in a bi/multidirectional manner (D5 and D1–4 and D6).
Cultural and community factors (both proximal and distal environmental influences) interact with parental illness, child development and mental health, parenting and the parent–child relationship, and service contacts in a multidirectional manner.
How these core components interact with and influence each other determines the quality of individuals’ adjustment within their family, as well as the adequacy of the whole family’s adaptation to living with a mentally ill member.
As well as conveying the relevance of relationships within current family circumstances, TFM also conveys a dynamic perspective of relationship interactions over time (a longitudinal/developmental approach) – for example, how multiple factors within and between individuals and their environments interact across the life span and between generations (Figure 26.2). It does this by encouraging thinking about a retrospective (“looking back”) and a prospective (“looking forward”) approach to practice. Information about need, risk, and resilience is used to inform support strategies, treatment plans, and recovery. This is based on the evidence linking early adversity with later susceptibility to psychiatric disorder and difficulties in the transition to parenthood – the intergenerational transmission of risk and resilience (Bifulco et al., 2002).
TFM thus provides a comprehensive framework which illustrates the interactions between a parent’s illness, the quality of parenting, the parent–child relationship, the individual attributes and needs of a particular child, and the genetic liabilities, family factors, and broader social/community supports that will collectively determine the quality of a child’s adjustment at any time point. The interplay between individual, family, and environmental vulnerability and resilience will amplify or ameliorate the emergence of any difficulty or disorder over time.
A framework to inform practice and training
This approach is based on the author’s use of TFM in a variety of services, feedback from clinicians and managers, and the use of TFM in training and consultation. Those using TFM independently have provided feedback about the usefulness of this preparation, using The Family Model Handbook (Falkov, 2012) for family-focused conversations. Use of TFM in clinical settings is being formalized as part of a master’s degree course in mental health at the University of Oslo (HiOA). Evaluation of the regional implementation of family-focused practice, using TFM as a framework, is currently underway in Belfast, Ireland (Health and Social Care Board).
The main barrier reported has been lack of confidence among mental health staff to “take the plunge” and initiate the conversation, an issue well described in the literature (see Chapter 22 of this volume). Questions about when to use TFM and in what circumstances are also common.
Using TFM in clinical practice
Overview
TFM’s visual map helps clinicians identify ways in which family members are connected, in a nonblaming, nonjudgmental way when someone experiences a mental illness. These conversations can be undertaken in adult mental health, child and adolescent mental health, and children’s services. A broad definition of “family” is used, which includes single, blended, and same-gender subgroups and consideration of noncustodial parents. Children’s safety is paramount – TFM is not a substitute for child-protection training. TFM is applicable to all psychiatric diagnostic categories, and there is explicit emphasis on resilience, strengths, and protective factors in the recovery process. The broad aim is to use TFM as a tool to facilitate engagement and broader thinking about connections between symptoms, parenting, and people, in a balanced and understandable way, highlighting both strengths and difficulties.
The clinical encounter
Each person meeting in a clinical encounter is provided with a photocopy of TFM (or it is drawn on a whiteboard). The approach is flexible and can be used with the unwell parent individually or with other family members and children, according to circumstances, in single or multiple sessions.
Single sessions have tended to focus on broadening thinking about impacts on the person with the mental illness and others in the family, illustrating why it can be helpful to involve others, as part of care planning and psychoeducation. Multiple sessions have generally been organized around the six domains, linking theoretical aspects of TFM to the individual’s experience and family circumstances.
Specific objectives include open dialog to support acquisition of age-appropriate knowledge about symptoms, their consequences for individuals, and reciprocal roles within the family. A shared understanding helps communication, supports children in asking questions, and empowers parental capacity to respond. This also helps to devise practical, age-appropriate strategies so that all persons can respond in a way that is manageable for themselves and supportive of the unwell person. The focus on strengths as well as difficulties can be empowering for all family members.
Clinical content
The initial introduction is prefaced with a brief explanation of the evidence now available about the impact of mental illness on all family members. Stigma is acknowledged explicitly, as is the fear of children being removed from a parent’s care. The conversation is presented as an opportunity for earlier intervention, with appropriate adjustment for setting and stage of illness – topics include developing a family-focused care plan, informing predischarge planning, relapse prevention, problem-solving, and psychoeducation.
The six domains provide the foundation for discussing symptoms in a parent or child (or both); topics include the interplay between symptoms and parenting; vulnerabilities and strengths; practitioner and case manager roles; and issues related to broader family, neighborhood, and cultural context. The consumer and carer focus acknowledges the fragmented service landscapes and multiple barriers faced by family members in seeking and securing good services and support.
Domains 1 and 2 illustrate, in a balanced way, that children experiencing mental illness will have an impact on their parents, and that parents with a mental illness will have an impact on their children. This shows the validity of both adults and children’s needs and supports discussion about the collective guilt that so many family members experience. This includes parental fears about their children’s future, their parenting ability, and removal of children from their care. It also includes children’s guilt about feeling responsible for parental problems and fears that their parent may die, as well as shame and stigma. This helps to validate the burden parents and children experience and makes it permissible to express this.
Depending on when the conversation occurs, talking about symptoms could be part of the assessment, intervention, or review. Parents’ knowledge about symptoms and diagnosis is essential to supporting dialog with their children and enabling children to ask questions.
Domain 3 is an opportunity to endorse everyone’s role in the family, affirming that working together will help recovery and that sharing concerns can help solve problems. Bringing fathers into the picture, regardless of whether they are ill, are carers, or are not living with children (dialog with or about fathers), is crucial. Clarifying the level of burden for children in a caring role can also be done here.
Domain 4 discussion about vulnerability validates the difficulties being faced, not only by the affected person but also other family members. This is essential for credible engagement in the next step, which is focusing on strengths and protective factors. This balanced approach helps to empower family members and provide mutual support in managing their difficulties and developing and practicing recovery and relapse-prevention strategies.
Domain 5 provides an opportunity to reflect on the clinician’s role and support effective engagement. This domain is based on the premise that a parent’s prognosis is directly linked to the quality of the relationship between key members of the mental health team and the family. It is an opportunity to gather additional information, directly observe interactions, ask about or reflect on progress and areas of success or difficulty, and, in so doing, build trust. This is also the place to “map” the services involved, their roles, and service gaps. A coordinated approach might include a multiprofessional, interservice meeting and consideration of the family’s role.
Confidentiality is important. Clinician familiarity with good practice regarding information sharing, privacy, and confidentiality helps ensure a balanced approach to any competing needs in the family. Respecting an individual’s confidentiality is not in and of itself a barrier to thinking about and talking with family members. The vast majority of consumer feedback reflects the wish for more, not less, family involvement.
Domain 6 allows for consideration of the family’s experience of stigma and discrimination, neighborhood and community support including religious institutions, and employment status as part of family-focused recovery-informed practice.
The arrows connecting the six domains (as shown in Figure 26.1) help to integrate information and formulate the family’s “story” in an empathic, shared way, reflecting themes such as loss, adversity, and resilience. The aim is to describe the unique features and circumstances in a family’s story in a connected, less fragmented way. This helps to show how individual and shared experiences have contributed to identity and the ways in which symptoms and illness have influenced this.
The developmental/life-span perspective (Figure 26.2) ensures that, in addition to looking at past experiences, the emphasis is future oriented. Looking ahead ensures meaningful and respectful incorporation of family responses to care planning and recovery.
Scenario 1 – talking about family with parents experiencing mental illness
Ms. M, a 31-year-old married mother of two children (aged 4 and 14) from a previous relationship, with an 18-month history of depression and PTSD requiring one previous admission, was brought to hospital following an overdose. She needed admission due to vague psychotic symptoms and anxiety, which settled during a 3-week admission.
Prior to discharge, her community case manager reviewed the management plan because of concerns about marital discord and its effect on her mental state. The supervisor suggested gathering more information about this and about the children, including their safety. The case manager used TFM with Ms. M to show the relevance of other family members, including children, and to facilitate conversation about her partner.
At the next supervision session, the case manager provided positive feedback about Ms. M’s response to using TFM and her readiness to talk about other family members, including her partner’s recent loss of job, alcohol consumption, and consequent aggression. Ms. M had asked if her partner could come to her next appointment, stating: “He needs to see this stuff – what the drinking is doing to the rest of us.”
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree