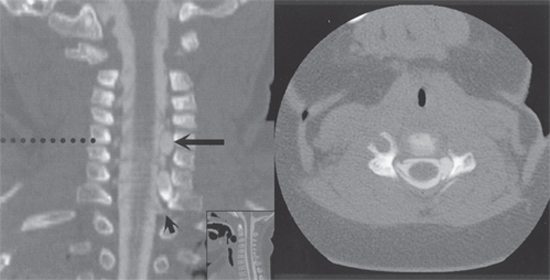
7 Pediatric Plexus Injuries A 4000 g female was born vaginally at term with a cephalic presentation. There was severe left shoulder dystocia, and the child was noted not to be moving the left arm, which was flaccid. When seen at 5 weeks of age, there was a left Horner syndrome, and the left arm remained flaccid without muscular contraction of any group. The hand appeared anesthetic. The remainder of the examination was normal. On electromyography (EMG), there was active denervation in muscles supplied by C5–T1 nerve roots, consistent with multiple root avulsions. Sensory nerve action potentials (NAPs) from the ulnar and median nerves of the affected limb were present (in concert with an anesthetic hand), in keeping with an intact ganglion cell–infragangli-onic pathway, again suggesting sensory root avulsion. The child failed to recover any function in the left upper limb over the subsequent 2 months. At 3 months, an iohexol computed tomographic (CT) myelogram suggested root avulsions within the dural sac involving all roots from C5 to T1. An anterior arachnoid cyst was present, displacing the cord posteriorly. The child proceeded to surgery at the age of 4 months. At surgery, exploration of the supraclavicular and infra-clavicular brachial plexus was performed. The roots of C5, C6, C8, and T1 were found to be related to an extremely neuromatous upper and lower trunk. The C7 nerve root could not be identified. Electrophysiological testing intraoperatively failed to identify somatosensory evoked potentials from any of the proximal nerve roots. A very delayed orthodromic muscle action potential was found from C5 to the axillary and musculocutaneous nerves. NAPs were recorded proximally to distally from the C6 and C8 roots. These findings confirmed an avulsion injury with an intact dorsal root ganglion of the affected sensory nerves. Exploration was extended to follow the proximal upper roots to the neural exit foramina, which were widened, and exploration of the thecal sac. The arachnoid cyst identified on preoperative myelography was decompressed. To examine the roots histologically, the C5 root was identified and divided. The root was found to be extremely neuromatous well into the proximal foramen. Having no motor drive from the plexus roots, the motor root of C4 and the distal accessory nerve were dissected and divided distally. An interposition graft from the accessory to the axillary nerve using harvested medial cutaneous nerve of the arm was fashioned. Similarly, the motor root of C4 was directed onto the musculocutaneous nerve via sural nerve grafts. On initial follow-up at 7 months after surgery, the child had shown some movement of the ulnar two fingers of the left hand, questionable flexion of the elbow, and some elevation and extension of the shoulder. No sensory function was noted. Gradually, the function of the left upper limb improved. At 3 years’ follow-up, the left arm was now used as a helper arm, having good biceps function, wrist extension, and some finger flexion. Abduction of the shoulder to 45 degrees was documented, with the abduction achieved by a combination of pectoralis major and deltoid muscle function. Severe brachial plexus birth palsy with multiple nerve root avulsions Shortly after delivery, the classical flail upper extremity may be observed by the obstetrician, midwife, or infant’s family. The entire plexus is affected in most infants at birth. By 2 to 6 weeks of age, however, the predominant level of the lesion should be well established. Traction on the brachial plexus is thought to be the predominant mechanism by which neurological injuries occur during maneuvers to clear the shoulder in a difficult delivery of a cephalic or breech presentation (Fig. 7–1). Non–traction related injuries are also recognized. Cephalic presentation accounts for over 90% of plexus injuries in the infant. The baby is typically large, weighing over 4000 g. Forceps or suction may or may not have been used during delivery. In this setting, the upper roots of the plexus are most affected. Plexus injuries may also occur in normal-sized infants without delivery-related trauma. In contrast, babies with plexus injury delivered as a breech presentation are usually small (less than 3000 g). Manipulation of the arm and extension of the neck for delivery result in lower root injury. Two classically described syndromes of brachial plexus injuries are seen. The upper plexus palsy (Erb paralysis) involves the C5 and C6 nerve roots with variable involvement of the C7 nerve root. The lower plexus palsy (Klumpke paralysis) involves the C8 and T1 nerve roots. In practice, isolated lower plexus injuries are rare (2 to 3%). Eighty percent of cases present as an upper plexus palsy with up to 10% involving both upper extremities. The remaining cases are combined total lesions. Figure 7–1 Cephalopelvic disproportion and shoulder dystocia during vaginal delivery cause traction to the brachial plexus, with avulsion of the lower spinal nerves and rupture of the upper plexus (C5 and C6 to the upper trunk and C7 to the middle trunk) elements. In the classic Erb paralysis (upper), the arm assumes a “waiter’s tip” position. The affected limb is extended with the shoulder internally rotated and adducted. The forearm is pronated and the wrist and fingers are flexed. The position results from paralysis of the deltoid, supraspinatus, infraspinatus, teres minor, biceps brachii, brachialis, brachioradialis, supinator, wrist extensors, and finger extensors. In upper plexus palsies, if the C4 nerve root is involved, phrenic palsy with secondary respiratory difficulties may exist. Unresolved conditions result in muscular atrophy with inferior shoulder subluxation, and wasting and atrophy of shoulder support muscles. The rare Klumpke paralysis (lower) is characterized by paralysis of the intrinsic muscles of the hand, wrist flexors, and long finger flexors. Patients present with a characteristic “claw hand” posture. The symptom complex represents C8 and T1 impairment. An associated ipsilateral Horner syndrome is often present from trauma to the sympathetic fibers that pass along the C8 and T1 nerve roots. Lower plexus injuries are usually not seen without some degree of upper plexus weakness. However, in contrast, upper plexus palsies may exist without lower plexus involvement. Shortly after delivery, the diagnosis of brachial plexus palsy is entertained by the observation of a flail upper extremity by the obstetrician, midwife, or infant’s family. The exam should then be repeated within 72 hours to more accurately assess the extent of injury, with special attention directed to the other extremity movements to evaluate for additional neurological injury beyond the brachial plexus. A good neurological exam at this point will also eliminate other causes of palsy such as brain injury, stroke, or spinal cord injury. It is important to rule out an upper extremity fracture or dislocation as a cause or contributory factor to the patient’s weakness. The initial evaluation of the injured infant should therefore also include x-rays of the shoulder (to exclude an epiphyseal fracture of the humerus), chest (to evaluate for a fracture of the clavicle), and elbow (to exclude a dislocation). The clinical examination remains the most important means of assessment. Precise examination of brachial plexus function in the infant is difficult and requires much patience and ingenuity. The cornerstone of examination remains simple observation, with note of the resting posture of the affected extremity. The child’s ability to reachand handle objects may give an insight to the extent of the injury. In the examination of the infant, both upper limbs and the trunk must be exposed. Dependent on the duration of the symptoms, the affected limb may or may not be atrophic. The child should be in a sitting position to assess the function of the key biceps and deltoid muscles against gravity. The affected limb is usually hypotonic and has absent deep tendon reflexes. The sensory examination is limited to identifying areas of anesthesia to painful stimuli in the severe cases. A Horner syndrome may be present. Examination may be more difficult in the overweight newborn. In addition to the clinical examination, EMG may help confirm the degree of brachial plexus injury and define the particular nerve roots affected. Evidence of reinnervation may be apparent with time, although correlation with clinical recovery may be poor. Somatosensory evoked potential monitoring may also help determine the level of injury but will not discriminate between incomplete root avulsion and intact roots. Radiological examination in evaluating brachial plexus injuries is useful primarily as a presurgical evaluation. CT and x-rays of the shoulder and neck will help exclude other causes such as fractures and mass lesions in uncertain cases. CT myelography is sensitive for revealing complete nerve root avulsions, with or without a pseudomeningocele (Fig. 7–2). At the current time, CT myelography provides a better definition of the nerve roots than does magnetic resonance imaging (MRI). However, MRI sensitivity is bound to increase, and this may aid in excluding other spinal cord or brachial plexus lesions. Spontaneous recovery is expected in a significant percentage of infants with brachial plexus injuries. Frequent review of each patient will give the surgeon insight as to the likely or unlikely requirement of surgical intervention. Given the favorable outcomes in conservatively managed cases, controversy surrounds the role and timing of surgical therapy. Irrespective of nonsurgical or operative management, a prominent role exists for gentle physiotherapy to prevent contractures and to document progress. The adjunctive role of muscle stimulation remains debated. In the Collaborative Perinatal Project, recovery occurred within 4 months of birth in 93% of patients having functional improvement after nonoperative management. Conversely, poor functional outcome had been reported in infants without signs of recovery at 3 months of age. The timing of surgery in patients without recovery remains controversial. Both early (3 months) and delayed surgery have been advocated with similar results. In a series of 50 patients who had failed to improve some motor function by 4 to 6 months and who underwent surgical repair, an improvement from the preoperative state in 85% at 1 year of follow-up was reported. Most of the reported literature have suggested an operative window of 4 to 6 months of age.
 Case Presentation
Case Presentation
 Diagnosis
Diagnosis
 Characteristic Clinical Presentation
Characteristic Clinical Presentation

 Differential Diagnosis
Differential Diagnosis
 Diagnostic Tests
Diagnostic Tests
 Management Options
Management Options
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



