Pediatric Spinal Cord Injury
Amer F. Samdani
Steven W. Hwang
Mary Jane Mulcahey
Randal R. Betz
Management of children with spinal cord injury (SCI) presents unique acute and long-term medical, surgical, and rehabilitative challenges. Advancements in medicine, technology, and public policy related to disabilities have combined to increase the life expectancy of these children (1,2). In this chapter, the authors review the epidemiology, classification, acute management, and medical/orthopaedic concerns for children with SCI.
EPIDEMIOLOGY
While they are likely underrepresented, approximately 3% to 5% of the reported SCIs each year in North America occur in individuals younger than 15 years of age, and about 20% occur in those younger than 20 years of age (3,4). Although boys more commonly sustain SCI than girls during childhood or adolescence, the frequency of SCI in boys and girls under 5 years of age is comparable (5). The level and category of the neurologic injury vary as a function of age, with younger children more likely having paraplegia or complete injuries (3,6,7). Life expectancy for children and adolescents with SCI is somewhat less than the general population and, like their adult peers with SCI, is a function of neurologic level and category. The less severe the SCI, in respect to level and completeness, the longer the expected survival (1).
The Trauma Audit Research Network Database spanning 1989 to 2000 includes 19,538 children younger than 16 years. Of these children sustaining some kind of trauma, 1.54% (301/19,538) suffered a cervical spine injury. Of these 301 children, 71% sustained a spinal column injury only, 21.9% sustained cervical column and SCI, and an additional 7% manifested spinal cord injury without radiographic abnormality (SCIWORA). Both cord injury and SCIWORA were much more common in children younger than 8 years of age (8).
Using another database, Patel et al. (9) found an incidence of cervical spine injury of 1.5% (1,098/75,172) in the National Pediatric Trauma Registry. The mean age of the study group was 11 years, and 61% were boys. As expected, lower cervical spine injuries occurred mostly in children older than 8 years. However, upper cervical injuries were prevalent in all age groups. Neurologic injury occurred in 35% of the children and was complete in 24%. SCIWORA occurred in 17% of these children. Except for fractures associated with birth trauma, children younger than 3 years rarely incur fractures below C2.
COMPLETE VERSUS INCOMPLETE
MECHANISM OF INJURY
The mechanism of injury varies with the age of the patient. However, motor vehicle accidents cause the highest percentage of injuries. In children aged birth to 5 years, violence and falls contribute the next highest number of injuries. In the age group 6 to 15 years, sports and violence are major culprits (3). Diving is most commonly associated with cervical spine injury, followed by football, gymnastics, and wrestling (12). In neonates, the leading cause of cervical injury is birth trauma. MacKinnon et al. (13) reported that the injury occurred from C0 to C4 in 64% of patients. Other etiologies of SCI in children and adolescents include child abuse and transverse myelitis (14, 15 and 16).
SCIWORA
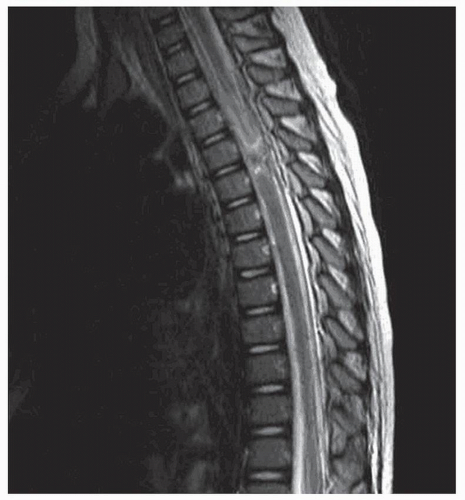
In 1982, Pang and Wilberger popularized the acronym SCIWORA for “SCI without radiographic abnormality” (17). These children sustain traumatic myelopathy with no radiographic evidence of bony injury. Four mechanisms of injury have been clearly implicated in the pathogenesis of SCIWORA: hyperextension, hyperflexion, distraction, and ischemia. The incidence of SCIWORA varies widely in the literature, from 5% to 67% (17, 18, 19 and 20). The wide variability is partly explained by inconsistent definitions of SCIWORA employed in the literature. At the time of the original report by Pang in 1982 (17), magnetic resonance imaging (MRI) was not widely available, and the definition relied solely on normal plain films and computed tomography (CT). Recently, with the widespread use of MRI, some authors have questioned the relevance of the term SCIWORA (19,21) (Fig. 34.1). Some, including ourselves,
are promoting the term “SCIWONIA”—SCI without neuroimaging abnormality.
are promoting the term “SCIWONIA”—SCI without neuroimaging abnormality.
The pediatric spine demonstrates numerous properties that make it susceptible to SCI without bony pathology. The high water content of the intervertebral disks and annulus allows for marked stretching. The neck muscles and uncinate processes are underdeveloped. The vertebral bodies are wedged ventrally, allowing for enhanced forward slippage. The facet joints are shallow with a horizontal orientation, rather than oblique as found in adults, which allows translational mobility both laterally and in flexion/extension. In addition, the ligaments and facet capsules permit significant stretching (22, 23, 24 and 25). This explains the phenomenon in young children of pseudosubluxation, or seemingly excessive angulation between C2 and C3 (26). These factors in combination with a high head-to-torso ratio increase the chances of injuring the inelastic spinal cord without obvious bony injury.
Delayed onset of neurologic deficit following SCIWORA has been reported (18,27, 28, 29 and 30). This usually occurs within 48 hours of injury and may be preceded by transient weakness or sensory impairment. Postulated mechanisms remain speculative and include occult spinal instability leading to repeated spinal cord trauma (28) or an ischemic etiology (31). Recurrent SCIWORA has also been reported in the literature (17,18,27,32,33), although some suggest the incidence may not be as high as first thought (19). Pollack et al. (32) reported that 8 of 18 patients sustained a more severe recurrent SCIWORA. The majority of the patients had a mild initial SCIWORA. Subsequently, four of the eight patients sustained permanent neurologic deficits. They attributed this recurrent SCIWORA to occult spinal instability and recommended a hard cervical collar for 3 months following the initial injury. Bosch et al. (19) in a follow-up report on the experience at the University of Pittsburgh suggest the rate of recurrent SCIWORA is lower than initially reported.
MRI findings correlate with recovery potential following SCIWORA (18,28,34). MRI evaluates the extraneural elements such as ligaments, disks, and soft tissue, as well as the spinal cord. A normal MRI portends an excellent recovery, whereas, increasing magnitude of spinal cord edema and hemorrhage implies more severe SCI. A study by Liao et al. (35) showed that imaging patterns on MRI correlated with neurologic recovery in children less than 8 years of age.
ACUTE MANAGEMENT
As with any trauma, maintaining strict adherence to Advanced Trauma Life Support protocol is vital for a successful outcome. A trauma patient is assumed to have an SCI until proven otherwise; this is particularly true in the pediatric patient in whom neurologic assessment may be difficult. Thus, the patient must be immediately immobilized and transported carefully to avoid exacerbating neurologic injury. The head-to-chest ratio for young children is high, and transportation on a regular backboard induces cervical kyphosis (36, 37 and 38). At age 8 years, the chest attains 50% of its adult size, and this discrepancy normalizes. Until then, a blanket or a 2 to 3-inch pad placed under the chest area or an occipital recess in the transport board help maintain cervical alignment.99 The use of tape and sandbags provides superior immobilization of the cervical spine compared with a hard collar. In patients wearing a helmet, removal ideally occurs in the emergency department while the head is manually stabilized. One must always be cognizant of the basic principles of emergency care, particularly because many children with cervical level injury have compromised respiratory function. Route of intubation, either orotracheal or nasotracheal, does not appear to cause neurologic injury when performed in a controlled manner (39).
The role of steroids in the pediatric population remains unclear. Bracken et al. reported that methylprednisolone improved spinal cord recovery up to five motor points if administered within 8 hours of injury. Most treating physicians use methylprednisolone in children, although only 15% of patients in the study were between 13 and 19 years old (40).
The injured child should undergo an expedited, yet thorough, history and physical evaluation, as the incidence of associated injuries is very high (41). Cardiac, abdominal, renal, and bladder injuries are often detected after the initial trauma evaluation. Patients with upper cervical injury may have cardiopulmonary arrest. Head injury occurs with SCI in 25% to 50% of patients (7,36). On palpation of the spine, one must assess spinous process step-off and tenderness, as these may indicate underlying injury. Torticollis is another indication of cervical spine injury. The neurologic examination must be repeated at short, regular intervals to ensure the rapid detection of deterioration. It is important to determine the presence of transient neurologic symptoms. At the time of examination, the patient
may not manifest any deficits; however, these patients may have occult instability, which if not detected may have catastrophic consequences.
may not manifest any deficits; however, these patients may have occult instability, which if not detected may have catastrophic consequences.
CLASSIFICATION OF NEUROLOGIC INJURY
The International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) provide a method for the examination of myotomes and dermatomes and classification of the neurologic consequence of SCI (42) (Tables 34.1 and 34.2). Although it is a routine technique for assessing pediatric patients with SCI and is considered the gold-standard assessment for both prognosis and outcomes, there has been little work in establishing the reliability of the ISNCSCI data with children and youth.
To date, Mulcahey et al. (43, 44, 45 and 46) have conducted the only reliability study of the ISNCSCI in children; results showed strong test-retest reliability of the ISNCSCI in a sample of 74 children and youth with chronic SCI. Despite high reliability, the majority of children under 10 years of age had difficulty with the pinprick exam, and the majority of children injured prior to being toilet trained had difficulty with the anal contraction exam. Child-friendly modifications to the ISNCSCI are needed. Replacing the safety pin with another sharp but less anxiety-provoking instrument and establishing the reliability of the new instrument for pinprick are needed. This modification may not have any bearing on reliability of the pinprick exam, but, importantly, the exam process may be much less stressing to children. The anal exam also requires modification for children. Children who have not experienced volitional control of their bowels had difficulty understanding and performing the anal examination. Often, children overcompensated for paralysis, resulting in abdominal muscle contraction as opposed to contraction of the anal muscles. Adolescents had an equally difficult time with the anal exam for reasons associated with privacy, sexuality, and self-image.
Until infant/toddler motor and sensory modifications to the standards are established, motor and sensory levels of children under 4 years of age should be approximated. Because severity of the injury (complete vs. incomplete) is not able to be tested in infants and toddlers, classification of the lesion by the standards definition is not appropriate. Therefore, documentation should clearly state that testing for neurologic severity will be done at a future time when cognitive abilities support the testing procedure. Parents should also be educated that their infant’s or toddler’s neurologic classification cannot be determined until they are older and able to understand the test instruction for the S3-S4 exam. Importantly, repeat neurologic testing in young children should be done annually or until there is confidence in an accurate exam.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree