Penetrating Craniocerebral Injuries
Although not as common as closed head injuries, pediatric penetrating craniocerebral injuries (PCIs) account for significant morbidity and mortality within the pediatric population. Neurosurgeons are often presented with difficult management decisions when treating children with PCIs. Although many neurosurgical techniques and principles apply, several unique factors require further consideration. In this chapter, we summarize the current epidemiology, pathogenesis, diagnostic evaluation, and treatment measures available to the pediatric PCI population. Special attention is directed toward surgical management and the prevention and treatment of complications.
54.1 Epidemiology
Emergency neurosurgical admissions for pediatric PCIs are on the rise in the United States. A recent study reported a 138% increase in pediatric PCIs in the last decade, as well as a 4% rise in pediatric gunshot wounds to the head.1 The true incidence is hard to quantify because of several factors, including the lack of a centralized database and the likelihood that victims incurring PCIs may die before reaching the emergency department (ED).2 Additionally, many of these patients have been excluded from studies of head injuries, which tend to focus on closed head injuries. A study from Ontario, Canada, of all deaths from blunt or penetrating head injury in children younger than 16 years of age during the period from 2001 to 2003 found that only 12 of 234 deaths were caused by penetrating injuries.3 PCIs can be attributed to five overall causes: (1) accidental injury with sharp or semisharp objects, (2) warfare, (3) accidental discharge of firearms, (4) suicide, and (5) homicide.
In the pediatric population, PCIs can be attributed to countless random objects. Case reports have been written of PCIs caused by pencils and chopsticks,4 broom handles,5 metal strips, plant branches, kitchen knives, dinner forks, wires, nails, spikes, scissors, screwdrivers,6 and even a potato peeler.7 Often, flying debris during automobile accidents is a mechanism of PCI.8 Furthermore, low-velocity projectiles, such as arrows, BBs, and pellets discharged from pneumatic “toy” weapons, can be included in the category of causes of accidental injury.9,10 There are two key factors to consider in the management of impalements: first, penetration through thin calvarial regions is frequently associated with a high risk for vascular or cranial nerve damage, and second, retained foreign bodies (especially radiolucent objects) increase the risk for infection.
Throughout history, the pediatric population has been plagued by warfare, with countless injuries to both innocent children and young soldiers. Two Iranian series of traumatic aneurysms, detailing the effects of military PCIs on the pediatric population, reported that 25% of patients were 18 years of age or younger.11,12 Furthermore, a recent study of a field hospital in Iraq found 52% of pediatric consultations to be related to PCIs.13 It is of note, however, that unlike most civilian PCIs, those incurred during warfare are caused mainly by shrapnel rather than bullets, and when they are caused by bullets, the bullets tend to be high-velocity bullets associated with a much higher mortality.14 Therefore, when the treatments and outcomes of PBI are studied, it is worth distinguishing between military and civilian populations. Because of the practical applications of this textbook, emphasis will be placed on civilian PCIs.
An alarmingly high number of PCIs in children can be attributed to the accidental discharge of firearms. Of all reported PCIs, 70% occur in the home setting.15 An increasing number of American households, 38% in a recent study, keep loaded weapons, allegedly for security reasons.16 However, in a series of 450 patients with PCIs from Cook County Hospital (Chicago, Illinois), only six firearm incidents were related to criminal invasion of a home.17 Furthermore, a study from the state of Washington stated that only 23% of firearm-related deaths were considered justifiable defensive homicides.18 Although it is less frequent in children, the practice of Russian roulette falls between the categories of accidental discharge and suicide, tending toward suicide,19 often resulting in lethal damage to the brain (▶ Fig. 54.1). More than 75% of the guns used in suicide attempts and in unintentional injuries of 0- to 19-year-olds were stored in the residence of the victim, a relative, or a friend.20
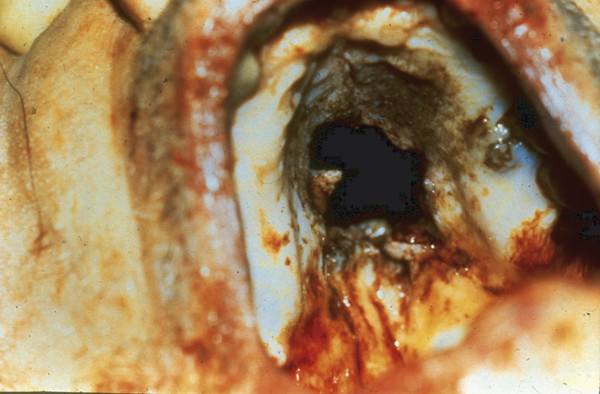
Fig. 54.1 Penetrating injury sustained during Russian roulette, with the bullet entering through the victim’s palate.
Firearms continue to be a popular method for committing suicide, especially among men. Although the elderly remain the fastest-growing group affected by suicide,21 there has been a threefold increase in childhood suicide during the past 40 years.22–24 The exact reasons for these increases are unknown; however, the situation likely reflects an increase in violence, poverty, and the availability of weapons.25 Suicide is currently the third leading cause of death in young Americans, with a rate of 13.1 per 100,000.25 The most common means of suicide in American youth age 15 to 19 years is firearms, accounting for 736 deaths (3.4 per 100,00).26 Hispanic women have the highest incidence of failed attempts, whereas rural Caucasian men have the highest completion rate.25,27–29
Of concern are two societal factors, often interconnected, that are affecting children at an increasing rate. The growth of criminal activities surrounding the illicit drug culture and the growth of gangs in urban, suburban, and even rural communities increasingly threaten the pediatric population (▶ Fig. 54.2 and ▶ Fig. 54.3).30

Fig. 54.2 Photograph of gunshot injury and associated gang tattoo.

Fig. 54.3 Plain anteroposterior skull film of a 20-year-old man demonstrating diffuse extracranial and intracranial shrapnel. This resulted from a shotgun blast at approximately 20 ft.
Furthermore, the abundance and ready availability of powerful weapons being used with lethal intentions add to the toxicity of the situation. Homicide is the second leading cause of death in children in the United States after unintentional injuries, accounting for 11.4% of all deaths in 2011 and 12.1% of all deaths in 2010.31 The 8-year (1994 to 2002) homicide mortality rate per 100,000 persons was 26.4% for children aged 0 to 14 years.32 In 2009, firearms were involved in 84.5% of all homicides of people aged 15 to 19 years.26 The fifth most common cause of death among patients aged 1 to 18 years reported in 2010 was firearm injury.33 More than 11% of pediatric patients who were shot in 2011 did not survive.34 In Tennessee, 47.8% of gunshot wound patients were between the ages of 14 and 25 years, whereas only 13.7% of the population of Tennessee falls within this age group.35 In Harlem (New York City), a reported 40% of childhood gunshot victims were the intended targets, with 60% of their assailants children.36 During 1991 in Los Angeles, California, 25% of all shooting victims, 412 of whom died, were younger than 18 years of age. Although traffic accidents are the leading cause of childhood deaths in the United States, gunshot homicides remain the leading cause of death among children in Los Angeles.30
An exponential increase in gang-related activities can be seen throughout many areas of the country. The best data have been compiled in the city of Los Angeles. As of 2005, there were at least 1,108 identified gangs in Los Angeles County with 85,298 members, according to the CALGANG System of the California Department of Justice. Gang-related murders in Los Angeles increased from 271 in 1985 to 597 in 2001. In 1993, a study of 105 children treated for PCI at the LAC+USC Medical Center over an 8-year period found that 76% of the injuries were gang-related.37 Likewise, Ordog et al38 reported that 80% of the childhood victims in their series past the age of 10 years were involved in gang-related violence. Statistically, most shootings have involved African-American young men; however, homicides are in fact the second most frequent cause of death in girls of all ages.39 Although gang-related and non–gang-related gunshot wounds show statistically significant differences in demographics and entrance sites, they do not differ in respect to survival and outcome.40
While prevention of such devastating injuries is the overall goal, it seems drastic societal changes will be necessary to reverse the trend of gang-related childhood fatalities. In any case, neurosurgeons must be prepared to treat pediatric PCIs.
54.2 Clinical Presentation, Diagnostic Studies, and Early Treatment
The initial assessment and treatment of PCIs occur at the site of injury. An effective and expansive emergency medical system has been established in most communities in the United States; therefore, emergency medical technicians and paramedics generally provide initial care. Appropriate resuscitation and stabilization attempts combined with prompt transport to EDs have positively influenced outcomes.41,42 Through communication with initial emergency response teams, the neurosurgeon is often a participant in these activities and should be familiar with assessment and stabilization procedures at the early stages of treatment.
Immediate attention must be given to the fundamentals of airway, breathing, and circulation (ABCs). Furthermore, PCIs are not limited to the cranium and can often involve the face and skull base. Obstruction of airways can be caused by blood, mucus, and posterior prolapse of the victim’s tongue. Brainstem injury can cause alterations in breathing. If the patient‘s respiration is effective, an orally inserted airway protective device should be inserted under direct visualization. If ventilatory support is required, oral intubation should be performed. A short-acting, nondepolarizing neuromuscular blocking agent (e.g., vecuronium, 0.01 mg/kg every 15 to 30 minutes) and sedative agent (thiopental, 4 mg/kg, or midazolam, 0.07 mg/kg) may be administered to the semiconscious victim to minimize rises in intracranial pressure (ICP). Nasal intubation should be avoided because of the increased risks for raising ICP and for iatrogenic injury. Although the role of hyperventilation in acute management has not been clarified, the administration of 10 L of supplemental oxygen per minute at a rate of 24 breaths has been recommended.43 Pulse oximetry and end-tidal carbon monoxide monitors are becoming standard equipment on ambulances and can be used to optimize patients’ ventilatory status.
Despite the often dramatic appearance of PCIs, life-threatening hemorrhage is rare; local pressure is generally sufficient to control bleeding in the field. Saline-moistened gauze sponges should be used to cover wounds. Exposed impaling objects should be left intact. A rigid collar should be applied before transportation if the possibility of concurrent cervical injury exists. Although routinely carried by transport teams, corticosteroids are not beneficial. The acceptance of patients for interhospital transfer is another common situation encountered by neurosurgeons, especially those at regional trauma or referral centers. Although all of the above issues still apply, it is necessary to ascertain if nonneurosurgical injuries have been fully diagnosed and properly stabilized. Consultations with a general or trauma surgeon at one’s home institution may be indicated; however, transfer should not be delayed to obtain diagnostic studies. Although availability has increased, it remains unclear if transport via helicopter or fixed-wing aircraft positively affects patient outcome.44,45 In fact, some studies indicate that the time for initial transport is inversely correlated with outcome, possibly because unstable patients with a worse prognosis are often transported more rapidly than stable ones.46,47
Upon the patient’s arrival at the neurosurgeon’s institution, the first step is the collection and documentation of essential information. This includes vital signs, Glasgow Coma Scale (GCS) score, a basic general and neurologic examination with the patient fully unclothed to survey all body surfaces, and a description of visible injuries. The location, size, and appearance of all wounds should be recorded. Creating a photographic record is recommended.
Ongoing management of the airway and circulation is essential. Hypoventilation (PCO2 > 40 mm Hg) and hypoxemia (PO2 < 80 mm Hg) need be avoided, as well as excessive hyperventilation (PCO2 < 25 mm Hg), which can adversely affect cerebral blood flow. An orogastric tube should be placed to decompress the stomach. A euvolemic state can be maintained by the judicious use of isotonic crystalloid fluids (normal saline) titrated to urinary output, accurately measured via a Foley catheter. Hemoglobin and hematocrit should be determined and type- and cross-matched blood obtained. An extremely low hematocrit can be caused by massive hemodilution via resuscitative efforts or by large blood loss, the latter resulting either from a laceration of a major vessel or from internal or external hemorrhage at other locations. This can lead to sudden and unheralded cardiovascular collapse, mandating aggressive correction of hypovolemia and anemia. In the young infant, enough blood can be sequestered in the scalp or cranial vault to result in hypovolemic shock without obvious external blood loss. Insertion of a central venous catheter is indicated for the assessment of intravascular volume status in the hemorrhaging patient.
The management of raised ICP or lowered cerebral perfusion pressure (CPP) may be necessary, either empirically in patients with deteriorating neurologic status or objectively in patients with intracranial monitors in place. Although potentially life-saving in a herniating patient, the effect of such management on outcome beyond the initial resuscitative period is yet to be fully established. Some adult studies report improved outcome when the blood pressure and ICP can be controlled to ensure a CPP above 70 mm Hg48,49 however, pediatric studies replicating these results are lacking. Pediatric studies have established a correlation between CPP below 40 mm Hg in patients younger than 10 years and high mortality rates.50,51 Appropriate measures may include mannitol (0.5 to 1 g/kg intravenously every 2 to 4 hours to a maximum serum osmolality of 310 mOsm/L), furosemide (0.5 to 1 g/kg every 1 to 2 hours), and boluses of 3% NaCl (2 to 5 mL/kg initially followed by 2 mL/kg every 6 hours) and pressor agents, such as dobutamine. Elevation of the patient’s head may slow hemorrhage from wounds but may adversely lower the CPP.43
Disseminated intravascular coagulation (DIC) can occur any time after significant cerebral injury as a consequence of the release of brain tissue thromboplastin and initiation of the coagulation/thrombolytic cascade. It is directly correlated with the amount of brain injury and likely happens as frequently in the pediatric population as in adults. The prothrombin time, partial thromboplastin time, level of fibrin degradation products, and platelet count should be followed serially to identify this form of consumptive coagulopathy. The replacement of appropriate blood components (fresh frozen plasma, cryoprecipitate, platelets) should be initiated to prevent uncontrollable hemorrhaging. Furthermore, DIC indicates a poor prognosis in the adult population52 and may be a similarly ominous sign for infants, having been shown to be a predicting factor in the Glascow Outcome Scale score53 and associated with poor outcome.54
54.3 Diagnostic Imaging
Computed tomography (CT) of the head is strongly recommended to evaluate the patient with PCI.55 In addition to axial views of bone and soft tissue, coronal sections may be useful in patients with skull base or high convexity involvement. In selected cases, plain films may help to delineate skull fractures and bullet fragments; however, the CT scout alone is generally sufficient (▶ Fig. 54.4). Routine magnetic resonance (MR) imaging is not generally recommended in the early evaluation period.55 Serial 5-mm CT cuts should be obtained from the vertex to the foramen magnum, with windowing to image bone, blood, and brain. Rescanning at different gantry angles can be helpful if large metallic fragments create markedly distorted images.
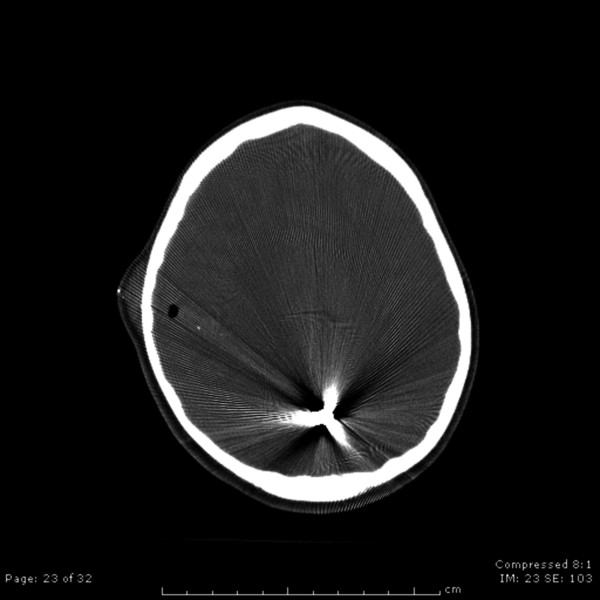
Fig. 54.4 Axial computed tomographic scan showing extensive cerebral damage from the bullet.
Subgaleal hematomas, common among children with PCIs, may be responsible for a significant loss of circulating blood volume. Skull fracture patterns can be used to distinguish entry and exit wounds and the paths of projectiles. Entry sites are characterized by small holes, in-driven fragments, and beveled edges; exit wounds tend to be larger and irregular. The paranasal sinus should be studied for the presence of air–fluid levels. Although extradural hematomas are rare in PCIs, their rapid identification and surgical removal offer improved survival rates compared with those of subdural hematomas and subarachnoid hemorrhages commonly associated with PCIs. On CT scans, cerebral contusions and parenchymal hematomas may appear bright, dark, or of mixed density based on the proportions of hemorrhage and edema. Isodense contusions occur with some frequency and are better imaged with MR imaging, if necessary. Potential findings also include intraventricular blood, shear injury (e.g., blood or edema along the corpus callosum), obliteration of the basal cisterns, and loss of gyral patterns.
Follow-up CT is warranted in selected cases because of the possible delayed development of intracranial hematomas. One study reported the highest rate of intracranial hematomas at 3 to 8 hours after initial injury. The development of a hematoma or further cerebral edema can present as acute deterioration, and therapeutic intervention may be required. Ischemic injuries, such as bilateral hippocampal, cerebellar, or watershed distribution infarction, may be seen on later scans.
MR imaging may play a role in evaluating injuries in several situations. First, it may be useful to ascertain cerebral contusion and shear injuries in patients whose neurologic examination is worse than would be predicted by CT scans. Second, MR angiography may be used to screen for traumatic aneurysms; however, in many cases in which vascular injury is suspected. conventional cerebral angiography is recommended. CT angiography may be beneficial as well. Third, gadolinium-enhanced MR imaging is more effective than contrast-enhanced CT when it comes to detecting cerebritis or the early development of extra- or intracranial abscesses, and it may be indicated in the evaluation of the febrile patient. Last, MR imaging may be useful in evaluating injuries from penetrating wooden or other nonmagnetic objects.55
Although MR imaging can be done safely in the majority of cases with retained metallic objects, neurosurgeons must exercise caution when ordering images. An in vitro and clinical study revealed that most bullets produced in the United States and shotgun pellets used in domestic and police situations are nonferromagnetic and can be exposed to contemporary MR imaging magnets (1.5-tesla range) without risk for rotational injury.56 Another recent study has indicated that common, commercially available bullets manufactured in the United States are safe in MR imaging scanners up to 7 tesla; however, armor-piercing rounds with steel cores are not.57 Additionally, a study focused on fragments resulting from combat and terrorist attacks found these artifacts to be safe at 1.5 tesla.58 ▶ Table 54.1 summarizes the ferromagnetic properties illustrated in these studies. Almost all metallic objects will distort and degrade images and can reduce the diagnostic yield of a study. As described in the ophthalmology literature, and of particular relevance to the pediatric neurosurgeon, BBs and pellets fired from many pneumatic weapons are generally made of steel and have the potential to move in strong magnetic fields.59 The best approach is to have an expert, such as a police officer, examine the weapon, spent casings, unfired ammunition, or any relevant evidence retrieved from the patient to determine the composition of the projectile. If the composition of the projectile cannot be confirmed, the neurosurgeon must weigh the benefits of MR imaging against the potential for injury to neural or vascular structures if the object moves during imaging.
| Object | Composition | Movement potential | Artifact potentiala |
| Shrapnel (bombs and artillery shells) or zip gun | Steel, lead, or mixed | ++ to +++ | 0 to +++ |
| Bullets | Bronze projectile | 0 | + to +++ |
| Lead projectile | 0 | ++++ | |
| Lead projectile; steel- or copper-jacketed | ++ | +++ | |
| Steel core; copper-plated, steel-jacketed | ++ | +++ | |
| Shotgun ammunition | Lead shot | 0 | + |
| Steel shot | + | + | |
| Pneumatic gun ammunition/BBs | Steel pellets | + | + |
| Source: From Eshed et al,58 Zheutlin et al,59 and Kim and Zee.60 aArtifact potential rated from 0 (least) to ++++ (most). | |||
Although useful, prognostication based on radiographic imaging is imprecise. Without an initial GCS score, no single radiographic finding can be independently predictive of outcome.60 Still, several observations have been noted, including elevated mortality rates with multiple-lobe,61 bihemispheric,62,63 multiplanar,64 and transventricular injuries62,64,65 (▶ Fig. 54.5), as well as subarachnoid hemorrhage,66,67 intraventricular hemorrhage,68 intracerebral hematomas,62 and basal cistern effacement.69 Furthermore, poor outcome associated with bihemispheric injuries has been reported in two groups, and occipital entrance wounds are usually fatal.70,71
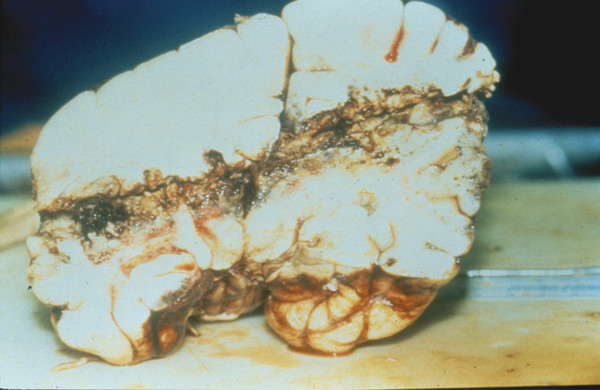
Fig. 54.5 Autopsy brain specimen of a through-and-through penetrating cerebrocranial injury with ventricular compromise following discharge of a rifle at short range. Note the discoloration of the tract and multiple areas of cavitation.
54.4 Surgical Treatment
Although most neurosurgeons would decline to operate on a patient without neurologic function, the choice for surgical intervention can be complex. When a low GCS score4,72,73 is combined with an ominous sign, such as nonreactive pupils or refractory hypotension, the decision to withhold surgery seems warranted.74 Upon review of the neurosurgical literature, the benefit of operating on patients with post-resuscitative GCS scores of 3 to 5 at the time of presentation remains unclear because of a mortality rate higher than 80% and a rate of poor outcomes that approaches 100%, with significant yet infrequent exceptions.75 The issue becomes more complex in the pediatric population because predictive pediatric models are nonexistent. Furthermore, the emotional overlay of tragedy is often compounded when children are involved, putting an overwhelming burden on parents when it comes to decision making. Under these circumstances, decisions must be individualized and based on an analysis of the clinical and radiologic factors, as well as discussion with colleagues and family members. In light of these complexities, neurosurgeons should generally err on the side of aggressive treatment with pediatric patients who have PCIs.
Kaufman74 has suggested three primary reasons to operate: (1) to remove foreign objects (e.g., missile fragments, bone) to prevent secondary complications, such as infection, posttraumatic aneurysms, and seizures; (2) to remove necrotic brain to prevent further hemorrhage, edema, and scar formation; and (3) to eliminate mass effect, especially that associated with hematomas, on viable brain. Other indications for operative management include debridement and closure of scalp wounds, repair of vascular injuries, and placement of a device to monitor ICP. Unfortunately, the data are insufficient to show the impact of these procedures on clinical outcome with accuracy. In any case, the current understanding of traumatic pathophysiology and standard of care would suggest that such procedures are often appropriate.76
Certain issues warrant further discussion. First, the timing of surgery is an important consideration. Certainly, hemodynamically unstable, multiply traumatized patients and those with DIC must be stabilized to avoid high operative morbidity and mortality rates. Although early and aggressive debridement has been the standard treatment in military PCIs,77,78 prompt but locally confined debridement is considered sufficient in civilian PCIs.74,79 For patients presenting more than 24 hours after injury, more aggressive debridement would be indicated because of an increased risk for infection. Scalp and skull wounds should always be explored for necrotic skin, hair, and bone fragments that can be safely removed. Dural and vascular injuries should be repaired and copiously irrigated. No evidence indicates that extensive parenchymal debridement or the removal of deeply penetrating bullet fragments or bone prevents infection. Two studies suggest that retained fragments may increase the incidence of late seizure development and traumatic aneurysm formation11,12; however, this must be weighed against the risk for further neurologic injury during operative manipulation. Most neurosurgeons recommend the prompt removal of “significant” hematomas; however, the minimal volume has not been established.74 Despite recommendations for a more aggressive approach with posterior fossa wounds, because of the small volume of this compartment and poor tolerance of compression, two series have found that pediatric patients with occipital entry wounds have poor outcomes despite surgical intervention.70,71
In most cases, standard craniotomy techniques should be applied. An important consideration in the design of the scalp flap is the excision of contaminated and heavily damaged soft tissue. Bone from the scalp and entrance sites can be removed if small local debridement is anticipated. Although some authors have advocated osteoplastic flaps, no reduction of the infection rate has been shown with this technique.52,80 Debridement of the parenchyma should be performed with the use of copious isotonic fluid irrigation and controlled suction. The primary goals are to remove large, easily accessible foreign objects at the entry and exit sites, remove hematomas, and control hemorrhage. The insertion of small-diameter red rubber catheters followed by irrigation to assist with the removal of deeper hematomas is rarely warranted. If necessary, a hemostatic agent such as peroxide or oxidized regenerated cellulose can be employed. Intraoperative ultrasound can be effective in localizing bone, metal, and clots. Objects as small as 1 mm have been detected when a 7.5-Hz probe was used. (However, deeply embedded objects should probably be left in place, regardless of size.74) Repair of a transgressed dural venous sinus is indicated if there is active hemorrhage, but the bleeding can often be controlled with tamponade. The anterior sagittal sinus may be ligated as far posteriorly as the entrance of the first major cortical vein.
The dura mater may be closed primarily or reapproximated. One recent military series reported a reduction in the incidence of cerebrospinal fluid (CSF) leaks and infectious complications with dural closure81; another study stressed watertight closure of wounds (with a graft if necessary) and closure of the scalp in layers.77 In general, if the wound can be debrided and irrigated and the scalp can be closed to prevent external leakage of CSF, then a dura mater approximation with absorbable suture material should be sufficient. The application of fibrin glue to the suture line can be considered because it is safely used in nontrauma situations to effectively prevent CSF leaks.52 When large defects are closed, suitable dural substitutes include vascularized pericranium, temporalis fascia, and fascia lata, although one author found that the latter did not prevent infection.82 Silastic (Dow Corning, Midland, MI) and other nonabsorbable materials should be avoided because they have been implicated in infections and remote hemorrhages.83 In many cases, dural defects can be managed with the application of a large piece of gelatin film between the exposed dural edges and the cortical surface plus the placement of oxidized cellulose on the external surface of the exposed dura mater.
Cleansed bone should be replaced unless highly contaminated. Although wire mesh can be safely used, acrylics should be avoided because of their tendency to harbor bacteria in their porous matrix. In one series of patients undergoing elective cranioplasty with methylmethacrylate, 22% developed infections if the mucosa of the frontal sinus was exposed.84 A delay of 6 to 12 months has been recommended if an extensive cranioplasty is required.75
If possible, the scalp should be closed in two layers, with absorbable sutures approximating the galea and a second suture line to appose the skin edges. A rotational flap may be necessary in cases of large defects. The prophylactic insertion of a lumbar drain to promote sealing of dural tears is not indicated; however, this method may be employed if a CSF leak develops.
The risk for infection and CSF leak is increased in patients who sustain transorofacial wounds, and thus special consideration is necessary.74 The assistance of plastic, head and neck, and/or oral surgeons may be warranted. Aggressive debridement of all cavities communicating with the intracranial compartment, exenteration of the frontal sinus mucosa, and dural repair are the standard treatments. Also of importance in these cases is perioperative broad-spectrum antibiotic coverage for gram-positive, gram-negative, and anaerobic organisms.
The insertion of an ICP monitor at the time of operation should be considered, based on the extent of the injury. Delayed edema occurs regularly in patients with PCIs, and rapid increases in the ICP may indicate the onset of progressive cerebral edema, hydrocephalus, or hematoma formation. Although ICP monitoring is indicated for all patients with severe closed head injuries,41,42 fewer than half of surveyed neurosurgeons reported routinely monitoring the ICP of patients with severe PCIs.85 Ventriculostomies can provide an advantage over extraventricular monitoring systems by allowing CSF drainage for the management of increased ICP or impaired CSF circulation. The efficacy of measures to lower the ICP in both adult and pediatric PCI victims is yet to be determined.
54.5 Complications
54.5.1 Infections
The specific rate of extracranial and intracranial infections in children with PCIs has not been reported; however, broader studies have shown high infection rates ranging from 25 to 50%.86,87 Some of the possible infectious complications include scalp cellulitis and abscess formation, osteomyelitis, epidural and subdural empyemas, meningitis, ventriculitis, cerebritis, and brain abscess. Based on studies of the general population, several factors are apparent when infectious complications are treated. First, the speed of the penetrating object is important. Although generally seen in a military setting, PCIs from high-velocity bullets tend to have a lower rate of infection, in the range of 5 to 7%.77,79,80,82,85,88–90 A study of low-velocity injuries in a pediatric population showed an alarmingly high rate (43%) of infectious complications.6 In the report of 54 cases, 14 patients developed brain abscesses, 6 meningitis, 2 scalp infections, and 1 calvarial osteitis. In almost all of the cases, infection was caused by Staphylococcus aureus. Second, there is a positive correlation between the infection rate and the level of contamination as well as delay in treatment. In-driven hair, scalp, and superficial bone in volumes larger than 1 mL are significant risk factors for infectious complications.89,91 Third, concomitant injuries (e.g., skull fractures with CSF leakage, paranasal sinus fractures that communicate intracranially, and oral injuries) have been historically associated with increased infectious complications. Fourth, the composition of the penetrating object correlates with infection rates, especially in instances in which foreign material is retained. Although most bullet fragments are hot, inert metals, many organic materials, especially wood, can harbor many pathogenic microorganisms. In a study of 42 patients (80% of them pediatric patients), almost 50% developed an infectious complication.87 Finally, surgical exploration and debridement play an important role in infectious complications. Although the removal of gross superficial contamination is important, the removal of deeply embedded bone and projectile fragments does not decrease the incidence of infection. Several authors reported good results with little or no retrieval of foreign objects.63,88,92 Some recommend serial CT if a minimalist surgical approach has been taken; however, careful clinical surveillance is generally sufficient on a long-term basis.
Prophylactic antibiotics do not ensure the avoidance of infection, nor has the role of prophylaxis been full clarified. Many authors support the need for the early administration of broad-spectrum antibiotics65,68,93 however, others recommend that intraoperative cultures be obtained and that antibiotics be administered only when the cultures are positive. One study reported a 10% incidence of meningitis and wound infection despite the use of antibiotic coverage.94 A variety of appropriate antibiotics are available; these range from single, semiselective agents like cefazolin to third-generation cephalosporins plus antipseudomonal and anaerobic agents. Antimicrobial therapy is given intravenously for 5 to 14 days with or without additional oral agents for a similar period. To reduce the rate of bacterial resistance as well as cost, the nature of the contamination should be considered when an antibiotic is chosen. We recommend that a 7- to 10-day course of cefazolin be administered to minimally contaminated patients, and that a 7- to 14-day course of ampicillin, gentamicin (or third-generation cephalosporin), and metronidazole be given to heavily contaminated patients. In the presence of methicillin-resistant S. aureus, vancomycin should be used instead of ampicillin. Furthermore, the debridement site should be cultured intraoperatively, as one study found a 76% correlation between wound cultures and brain abscesses in patients in whom this complication developed.91
Evaluation for infection should definitely be undertaken in the case of patients with PCIs who have fever, a change in mental status, or new focal neurologic deficits. Although laboratory studies, such as white blood cell count, C-reactive protein, and erythrocyte sedimentation rate, can be correlative, obtaining an imaging study is a priority. CT offers the benefits of speed and affordability, but contrast MR imaging may have better diagnostic abilities. MR imaging can discern soft tissue, bone, and brain infections in their earliest stages. T1-weighted images will show sulcal effacement with mass effect, whereas T2-weighted images show increased signal of cerebral edema associated with early cerebritis.95 It should be noted that during attempts to distinguish between an infectious process and simple posttraumatic cytotoxic edema, paramagnetic contrast enhancement will generally be present in developing cerebritis and abscesses, although exceptions have been found early in the process.96 When imaging is ambiguous, empiric antibiotic coverage should be considered and a study repeated 7 to 10 days later to determine if a characteristic ring-enhancing lesion has developed. In patients with meningitis, fine-cut CT, CT cisternography, or MR imaging of the skull base can help evaluate potential sites of CSF leakage. Appropriate medical and/or surgical intervention should be undertaken as directed by the imaging and is discussed elsewhere.
54.5.2 Seizures
Cases of seizure, including early-onset seizure (less than a week), late-onset seizure (after a week), and epilepsy (chronic seizure disorder), are not well documented in children with PCIs. If one considers the nature of the central nervous system in pediatric patients with closed head injuries, which has been studied, one would expect the rate of seizures to be high after PCIs.97 In series of adults with PCIs, the incidence of early seizures ranged from 1 to more than 30%, considerably higher than the incidence in patients with closed head trauma, and the incidence of late seizures has been reported to be as high as 54%.98 In most cases, late seizures occur four to eight times more often than early seizures, implying that the two conditions may have a different pathogenesis.96 The data, however, are confounded by the variable administration of prophylactic anticonvulsant medications.63,93,97–99
To better understand the incidence of seizures in the pediatric population with PCIs, it is necessary to evaluate the literature on traumatic brain injury that is restricted to this age group. Despite the fact that the vast majority of patients sustained closed head injuries, several studies have reported incidence rates of early seizures of 5 to 15%.100–109 One series of patients with low-velocity PCIs reported a 17% incidence of early seizures.6 The long-term follow-up of pediatric patients with PCIs is poor; likewise, the incidence rates of late seizures and epilepsy have been reported infrequently. However, larger series with small numbers of children suggest that late seizures and epilepsy are more frequent than early seizures.
Some authors have attempted to identify the clinical characteristics that are predictive of posttraumatic seizures in children following PCI.103–106 Possible predictors include a GCS score of 3 to 8, diffuse cerebral edema, acute subdural hematoma, prolonged loss of consciousness, and depressed skull fracture. The strongest indicator is a persistently low GCS score, with up to 53% of children in this category manifesting early seizures. However, in one retrospective analysis of seven children with PCI and a low GCS score, none manifested early seizure activity.106 Overall, the identification of predictive factors for posttraumatic seizures in the pediatric population remains incomplete.
Although earlier literature suggested no benefit,107–110 prospective and retrospective studies including both adults and children generally affirm the efficacy of phenytoin for the prevention of seizures in the first week after injury.98,102,106,111,112 In one survey, 84% of neurosurgeons reported the routine use of prophylactic anticonvulsant medication for patients with severe head injuries.84 In a prospective adult trial, the reduction in the rate of seizures was nearly fourfold, from 14% in the placebo group to 4% in the treated group. Still, in studies, the rates of late seizures and epilepsy have not been reduced, suggesting that prophylaxis is not effective on a long-term basis.
Overall, based on a summary of the literature, prophylactic anticonvulsants in the first week after injury would be recommended for most pediatric patients with PCIs. Seizure-related increases in ICP and other secondary injuries may then be reduced. Withholding prophylactic anticonvulsant medications from children with minor injuries and high GCS scores would also be an acceptable protocol. After the first week of hospitalization, the decision to continue anticonvulsants should be made on an individual basis. However, the occurrence of early seizures does not bode well for patients, who remain at high risk for the development of epilepsy requiring long-term anticonvulsant medications.101
Although phenytoin is the most commonly used anticonvulsant medication in published series, other medications should be considered. Phenytoin, when administered orally or intravenously, is highly effective and generally safe. For very young children, or those who may need extended therapy, phenobarbital is a good choice; however, it can cause adverse behavioral changes. During the acute period, intravenous administration is crucial, especially in the case of infants, who have poor enteral absorption of many anticonvulsant medications. If intravenous access is not possible, the rectal route is acceptable for phenytoin and the benzodiazepines; hospital pharmacies can generally prepare the medications quickly if needed. The key factors in safety and effectiveness are administration of the loading dose and surveillance with frequent serum levels. Assessment of the levels is necessary every 2 to 3 days, especially because significant fluctuations in phenytoin levels are observed in severely injured patients with unstable serum protein levels.113
Discontinuation may be possible after 3 to 6 months if the patient remains seizure-free; however, little guidance has been found in the literature regarding this matter. If seizures have developed in a child more than a week after injury, anticonvulsant medication should be continued for at least 2 years, at which point the recurrence rate is still expected to be high. Furthermore, over time, the clinical and electroencephalographic (EEG) manifestations may change, with one study showing an evolution from early generalized to later focal types based on the site of injury.97 The treatment of focal seizures, which can be difficult to control, may require the help of a pediatric neurologist. Before anticonvulsant medications are withdrawn, an EEG is often sensible.
54.5.3 Traumatic Aneurysm Formation
The formation of cerebral aneurysms after PCIs is an uncommon yet well-known event, occurring in up to 5% of patients with PCIs in all age groups.11,12 Although the incidence in pediatric PCIs is unknown, some suggest it is more common among the pediatric population that in adults.114 A study at Children‘s Hospital Los Angeles found 7 cases of pediatric traumatic aneurysm over a 17-year period, one of which was secondary to PCI.114 In a military series from Lebanon, 13 of 40 victims in whom aneurysms developed after injury to the head from high-velocity projectiles were 18 years of age or younger.11,12 Low-velocity injuries can also cause aneurysms, as shown in a study of 54 patients, 2 of whom developed traumatic aneurysms after impalement or pellet wounds.6
Pseudoaneurysms are the most common lesions and are thought to result from damage of the arterial adventitia and media within hours or a few days after injury. Pseudoaneurysms can evolve along the length of any damaged cerebral artery, including the intracavernous carotid, can involute or enlarge unpredictably, and may hemorrhage early or many years later, with potentially devastating outcomes. Behavioral and neurologic changes have been linked to these lesions.114 Acknowledged predictors for the development of traumatic aneurysms include: (1) course of a projectile or bone fragment through areas of dense vasculature or the skull base, (2) impalement of an object through the above-mentioned regions, (3) trans-hemispheric passage of a projectile, (4) large intracerebral hematomas associated with an entrance wound, (5) multiple fragments with scattered paths, and (6) heavy arterial bleeding during initial debridement.11,12,67 Cerebral angiography at 7 to 10 days after injury should be seriously considered in the presence of any of the above-mentioned factors. Because immediate surgical treatment is considered safe and effectively eliminates the risk for hemorrhage, aneurysms of any size should be clipped, excised, or wrapped. Similarly, abnormal vessels should be treated at the time of initial debridement.
54.5.4 Wandering Fragments and Lead Poisoning
Several case reports exist of wandering metallic fragments along the neuraxis. Reports have been made of the migration of shotgun and air rifle pellets into the anterior and posterior cerebral circulation through both intra- and extracranial wounds, creating cerebral infarctions.115 One author describes cerebral softening, leading to the migration of large bullet fragments. The high specific gravity of metal compared with that of brain, and the sink action of the CSF flowing through the cerebral ventricles, may contribute to this condition.116 Both fatal migration into the brainstem and the development of hydrocephalus when fragments occlude the cerebral aqueduct have been documented.117–119
Another uncommon complication of retained metal fragments is lead poisoning.120 Several weaknesses in the analysis of the data for this topic have been reviewed.120 Well-documented cases exist of victims with an extensive amount of shotgun pellet throughout the body. Unfortunately, urine lead levels may be unreliable. Furthermore, the latent period of lead poisoning can vary from 6 months to many years, and the signs and symptoms are generally erratic and indistinct, including weakness, dizziness, headache, abdominal pain, constipation, and vomiting. Because of the decline in the use of lead in ammunition, the already infrequent problem of lead poisoning should wane even further.
Considering the above factors, if surgical removal is contraindicated because of potentially worsening neurologic injury, retained fragments near ventricles or major cerebral vessels should receive diligent surveillance. An immediate radiographic evaluation (either CT or cerebral angiography) should be undertaken at the onset of focal deficits or a deterioration in clinical status. Because of the potential for secondary hydrocephalus or neurologic injury, most intraventricular fragments should be removed. Locating the object radiographically in the operating room, before surgical exposure, is recommended because large bullets can move with positioning.116 When there are large amounts of retained lead fragments, the patient should be monitored clinically for signs or symptoms of lead poisoning. In the case of diagnostic evaluation and/or chelation, consultation with a hematologist or toxicologist is recommended.
54.6 Survival and Prognostic Factors
Any discussion of outcomes in children with PCIs is plagued by problems that include early and high mortality rates compounded by the overall small number of victims, so that predictive analysis is difficult. As mentioned earlier, withholding care from a patient presenting with a GCS of 3 and fixed pupils after initial resuscitative efforts seems wise. Likewise, one series121 noted that no pediatric patient with a traumatic brain injury and concomitant protracted anoxic insult regained useful consciousness, suggesting that supportive care alone is appropriate in this group. Aggressive neurosurgical management should be pursued in patients with GCS scores of 12 to 15 and limited parenchymal injuries because they often have excellent functional recoveries.
The dilemma most commonly associated with PCIs is the management of patients with moderate to severe injuries. Many seriously injured children can survive with aggressive surgery; however, quality of life is often greatly compromised. One series of patients presenting with GCS scores of 3 to 5 reported that 99% of nonaggressively treated patients died. Although the majority of patients who underwent surgery survived, 90% had severe long-term disabilities, with families and physicians often questioning the good of the intervention.122 Other series report a multitude of lasting complications, including persistent vegetative state, functional dependency, blindness, paralysis, seizure disorder, and profound neuropsychological alterations affecting memory, language, and behavior.71,123,124 An analysis of war veterans who were young adults at the time they sustained PCIs found a substantial decrease in life expectancy correlated with posttraumatic seizure disorder in comparison with the general population.125
Most studies of children with craniocerebral trauma focus on those with closed head injuries, and one must be careful when applying their findings to children with PCIs. Regardless, studies of outcome in children with severe craniocerebral trauma create a disconcerting image. One study found that long-term survival is much more common in children with prolonged periods of unconsciousness or vegetative state than in adults.121 At least one study has connected GCS score with neurobehavioral outcome, showing that patients with an initial score of 5 or less, as well as those who had a slow improvement in their GCS score, demonstrated substantial long-term impairments in intellect, adaptive problem solving, memory, academic performance, motor performance, and psychomotor problem solving.126 Still, even children with less severe injuries have been found to have significant limitations in physical health and behavioral problems and can require special educational intervention in comparison with the general pediatric population. Contrary to the belief that children fare better than adults, the analysis of Kaufman et al123 of a small group of patients with PCIs found similar incidences of problems regardless of age, including functional disability, need for special education, and extreme emotional lability. Generally, if improvement occurs in moderately or severely injured children, it usually plateaus after the first year following injury.121–127 In some children with less severe injuries, the harmful consequences for cognition, behavior, and psychosocial adjustment may not be fully realized until adulthood.128,129 One study found that only 23% of adults who sustained traumatic brain injury in their preschool years were able to work, and only 36% lived independently in the home setting.129 Another study of PCIs, focusing on patients presenting with GCS scores of 3 to 8, concluded that although mortality rates are high, patients who survive to receive inpatient rehabilitation can achieve functional improvement.127 Long-term focal deficits can often be reliably predicted based on the location of an injury,130 but the heterogeneity of the PCI population makes further predictions and analysis quite challenging.
Pearls
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








