Figure 59.1. 2-(2-oxo-1-phenyl-5-pyridin-2-yl-1,2-dihydropyridin-3-yl) benzonitrile hydrate, M.W. 349.38 (perampanel).
PERAMPANEL PHARMACOLOGY
Glutamate is the major excitatory neurotransmitter in the CNS. Fast glutaminergic transmission is mediated predominantly by NMDA and AMPA receptors within the CNS. In vitro studies suggest that selective blockade of NMDA receptors has only minimal effect on hippocampal epileptiform activity, while AMPA receptors are quite important in initiating epileptiform discharges and mediating epileptic synchronization (3). AMPA receptors are glutamate-gated ion channels that are formed as tetramers of protein subunits. These receptors are widely distributed throughout the CNS and are found both in the postsynaptic membrane of excitatory neurons and in inhibitory interneurons as well.
Glutamate receptor antagonists have been evaluated to treat a variety of neurologic disorders, including hypoxic injury, amyotrophic lateral sclerosis, Parkinson disease, and epilepsy. NMDA receptor antagonists, however, produced unacceptable CNS depression. NMDA receptor gating is also necessary for induction of long-term potentiation, which is likely an important cellular process in memory formation. Blockade of NMDA receptors can abolish long-term potentiation and has been found to impair memory formation. In contrast, selective blockade of AMPA receptors does not appear to interfere with long-term potentiation, and animal studies suggest no impairment in memory formation, even at higher doses (4).
Based upon the growing understanding of the importance of AMPA receptors, a number of early competitive antagonists were developed. The quinoxalinediones such as CNQX demonstrated poor in vivo response due to lack of penetration across the blood–brain barrier. Subsequent analogs such as NBQX showed improved permeability and demonstrated in vivo anticonvulsant response in a number of seizure models.
Talampanel, a 2,3-benzodiazepine, is a selective noncompetitive AMPA antagonist that demonstrated good CNS penetration but only had modest potency. Although showing initial promise for treating localization-related epilepsy and ALS, this compound was not effective for treating malignant gliomas and was not further developed (5).
Perampanel—2-(2-oxo-1-phenyl-5-pyridin-2-yl-1,2 dihydropyridin-3-yl)benzonitrile hydrate (4:3) or benzonitrile, 2-(1′,6′-dihydro-6′-oxo-1′-phenyl[2,3′-bipyridin]-5′-yl)—was discovered via high-throughput screening program using [3H]AMPA-binding assay to find selective competitive displacers at the glutamate recognition site in rat cortical neurons (3,6,7). Perampanel was shown to inhibit AMPA-induced responses in a noncompetitive manner in cultured rat neurons, with little to no inhibition of NMDA receptors (6).
In keeping with in vitro observations, perampanel demonstrated efficacy in a variety of animal seizure models, including audiogenic seizures in DBA/2 mice, as well as maximal electroshock, pentylenetetrazol, and 6-Hz tests (7). Interestingly, this spectrum of efficacy across diverse seizure models differentiates perampanel (from a mechanistic perspective) from more traditional sodium channel–blocking AEDs, which are relatively inactive in 6 Hz or pentylenetetrazole models (6). Perampanel was not active, however, in the WAG/Rij rodent model of absence seizures (7).
PERAMPANEL PHARMACOKINETICS AND DRUG INTERACTIONS
Perampanel pharmacokinetics in humans has been delineated in 14 phase I studies in single doses ranging from 0.2 to 12 mg and in chronic once-daily doses ranging between 1 and 12 mg/day (8). Following oral administration, perampanel is rapidly and essentially completely absorbed with a median time to maximal peak concentration of 0.75 hours (0.5 to 1 hours). Perampanel does not appear to be a substrate for xenobiotic efflux transporters such as P-glycoprotein or breast cancer resistance protein (6). When given with food, perampanel absorption is slowed (tmax 3 hours later in fed vs. fasted state), and resulting maximal peak concentrations are reduced by about 28%, but the overall extent of drug absorption is not significantly altered. Perampanel absorption is linear, and plasma concentrations are dose proportional. Perampanel is approximately 95% bound to plasma proteins, and its binding appears to be linear. Following oral administration, perampanel displays an initial decline in plasma concentrations over 12 hours, with a long elimination phase. Perampanel terminal elimination half-life has been reported to range between 53 and 136 hours, with an average half-life of about 100 hours in the noninduced subject.
Perampanel is extensively metabolized via CYP3A4, with the main metabolic pathway being oxidation at the pyridine, benzene, or benzonitrile rings and subsequent glucuronide conjugation. Although several metabolites have some activity at AMPA receptors, their potency is much weaker than the parent molecule, and their contributions to clinical activity in patients are likely minimal (6).
Consistent with its long elimination half-life, accumulation was evident with multiple-dose administration, and perampanel concentrations at steady state were substantially higher than after a single dose. Renal elimination of perampanel is minimal, with <0.12% of an administered dose eliminated unchanged in urine. In subjects with mild (Child–Pugh A) and moderate (Child–Pugh B) hepatic impairment, unbound systemic exposure was 1.8- to 3.3-fold higher, and half-life of perampanel was approximately twofold longer than that in healthy subjects.
Perampanel oral clearance is significantly influenced by the presence of concomitant enzyme inducing AEDs, such as phenytoin, oxcarbazepine, or carbamazepine, which can increase perampanel oral clearance by about two- to threefold. While concomitant administration will reduce perampanel elimination half-life, it is still sufficiently long enough to support once-daily dosing. Pharmacokinetic/pharmacodynamic analyses showed that increased steady-state perampanel plasma concentrations were related to decreased seizure frequency and increased probability of achieving ≥50% reduction in seizure frequency (9). This association between plasma concentration and improved clinical response was seen in patients enrolled in the clinical trials irrespective of whether or not they were receiving an enzyme-inducing AED (10). Although there was no apparent effect of enzyme inducers on the concentration–response curve, the dose–response curve may be shifted due to patients receiving concomitant enzyme-inducing medications having lower perampanel concentrations. Patients receiving inducing medications may require higher maintenance doses of perampanel than do noninduced patients.
Perampanel has few other pharmacokinetic interactions. Data derived from the clinical trials suggest that topiramate concentrations may be increased by 20% and oxcarbazepine concentrations increased by 35% (9). Perampanel 12 mg/day decreased levonorgestrel concentrations by 40%, and patients may require additional nonhormonal forms of contraception while taking perampanel. In that perampanel is extensively metabolized by CYP3A4, it is likely that inhibition of this isozyme will result in potentially meaningful changes in perampanel pharmacokinetics. Given its long elimination half-life, however, changes in perampanel plasma concentration in the presence of a strong CYP3A4 inhibitor, such as ketoconazole, are not likely to be evident in the short term but might develop slowly after chronic administration (11). Therapeutic plasma concentrations have not been established for perampanel, though the effective dose range of 4 to 12 mg/day was associated with a range in plasma concentrations of approximately 200 to 800 ng/mL (9). A pharmacokinetic/efficacy model of phase III study data showed expected effects of AED inducers in reducing median perampanel concentration (median Cavss approximately 200 and 300 ng/mL for perampanel 8 and 12 mg/day doses with inducers and 550 and 700 ng/mL for 8 and 12 mg/day perampanel doses without inducers). Predicted reductions in seizure frequency corresponded to increasing concentrations across these concentration ranges (12). Similarly, data are still insufficient to determine a “toxic” plasma level; however, analysis of the phase 3 data suggests that the incidence of certain adverse effects such as dizziness, somnolence, euphoric mood, irritability, gait disturbance, dysarthria, and weight increase did appear to increase at higher perampanel plasma concentrations (9).
CLINICAL EFFICACY
Perampanel was not effective in treating multiple sclerosis, Parkinson disease, or migraine prophylaxis when tested at low 0.5- to 4-mg/day doses. Two phase IIa studies showed, however, that most patients with localization-related seizures tolerated much higher doses of perampanel, and clinical development was done using 2- to 12-mg/day doses. A placebo-controlled “maximum tolerated dose” trial showed that nearly all patients with epilepsy tolerated 4-mg/day doses when given once a day or divided twice a day. In a subsequent dose-escalation trial, the majority of patients tolerated perampanel 8 mg/day; dose-limiting side effects—usually dizziness and somnolence—became more common at perampanel doses of 10 to 12 mg/day (13).
Subsequent epilepsy trials evaluated perampanel doses of 2 to 12 mg/day (compared with placebo), with the largest number of patients treated with 8-mg/day doses. The efficacy, safety, and tolerability of perampanel for treating localization-related seizures were evaluated in three large global trials and in several extension studies (Fig. 59.2) (14–18). Patients were adults and adolescents (≥12 years) with highly treatment-resistant epilepsy (≥4 or more seizures per month despite >80% taking two or three concomitant AEDs). In these pivotal dose-ranging trials, treatment with perampanel 4 mg/day, but not 2 mg/day, was effective and established the lower effective dose range for the medication. Doses of 8 and 12 mg/day were effective compared with placebo, but patients had only small increases in efficacy with 12 mg/day compared with 8 mg/day. A large proportion of patients treated with 12 mg/day had CNS-related adverse events, demonstrating an upper effective dose range. Responder rates (>50% seizure reduction) in the three pooled pivotal trials were 28.5% for 4-mg/day, 35.3% for 8-mg/day, and 35.0% for 12-mg/day doses (compared with placebo, 19.3%) (18). Reductions in patients’ median seizure frequency were similar: 23.3% for 4-mg, 28.8% for 8-mg, and 27.2% for 12-mg dose groups. One of the pivotal trials included several study sites in Latin America with unusually high placebo responses (15). The results from these sites were included in the primary efficacy analysis but were removed for several of the sensitivity analyses. Perampanel was tested in a large number of countries and ethnicities (Europe, the Middle East, South Africa, Southeast Asia, China, and North and South America), with similar overall treatment responses across various regions and ethnicities.
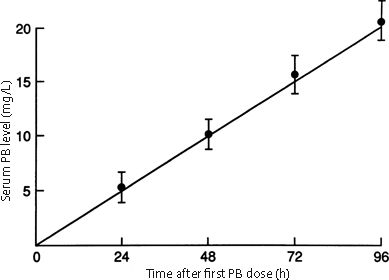
Figure 59.2. Efficacy of perampanel: proportions of 50%, 75%, and 100% responders (ITT analysis of pooled data for all partial seizure types). (Data from Steinhoff BJ, Ben-Menachem E, Ryvlin P, et al. Efficacy and safety of adjunctive perampanel for the treatment of refractory partial seizures: a pooled analysis of three phase III studies [published online ahead of print May 10, 2013]. Epilepsia. 2013;54(8):1481–1489.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








