♦ Preoperative
- Consider motor, visual, and language deficits that will result from surgery
- Worsening of motor deficit unlikely if damage occurred before age 4
- Completion of total hemianopia is unavoidable and part of informed consent
- Language deficits considered if incomplete transfer to contralateral hemisphere
- Worsening of motor deficit unlikely if damage occurred before age 4
- Timing of surgery
- Severity of epilepsy and age of patient determine timing; safe to perform after 4 months of age
- When hemisphere is damaged before age 3, as in perinatal infarct, there is minimal risk of long-term worsening of deficit
- In later onset cases, such as Rasmussen encephalitis, severity of seizures may necessitate hemispherectomy before transfer of language
- When hemisphere is damaged before age 3, as in perinatal infarct, there is minimal risk of long-term worsening of deficit
- Severity of epilepsy and age of patient determine timing; safe to perform after 4 months of age
- Preoperative preparation
- Give antiepileptic drugs, dexamethasone, intravenous antibiotics
- Type and cross for two units of packed red blood cells
- Preoperative coagulation parameters
- Give antiepileptic drugs, dexamethasone, intravenous antibiotics
- Special equipment
- Ultrasonic aspirator
- Frameless stereotaxis
- Ultrasonic aspirator
- Thiopental induction and maintenance with remifentanil and isoflurane
- Foley catheter
- Arterial line
♦ Intraoperative
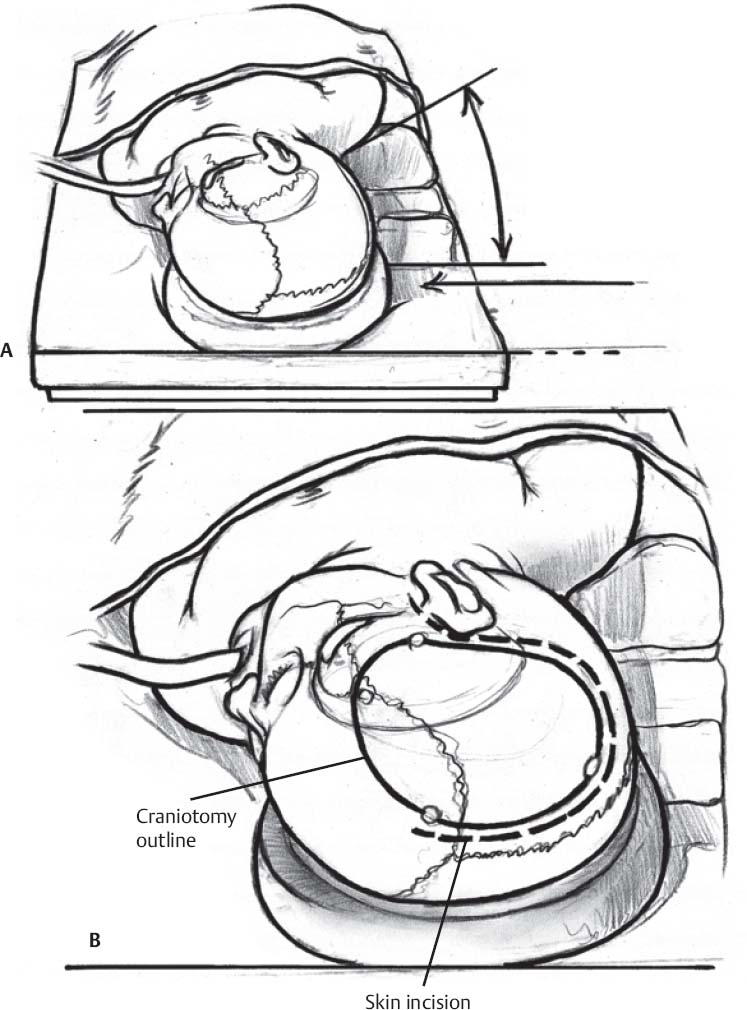
- Positioning: lateral decubitus or supine with the ipsilateral shoulder raised (Fig. 167.1A)
- The frontotemporal region is parallel to the floor and the vertex tilted inferiorly
- Opening: craniotomy is centered over the insula
- Skin incision is 10 to 12 cm extending from root of zygoma, curving posteriorly, then anteriorly to hairline (Fig. 167.1B)
- Bone flap is 7 × 5 cm: rostral extent at plane of corpus callosum, caudal extent 1 cm below level of ascending M1 branch; anteroposterior extent depends on length of Sylvian fissure (Fig. 167.1B)
- Skin incision is 10 to 12 cm extending from root of zygoma, curving posteriorly, then anteriorly to hairline (Fig. 167.1B)
- Dural opening and dissection of the Sylvian fissure
- Cruciate opening of dura
- Dissect sylvian fissure under microscope, sparing middle cerebral artery branches
- Expose insula and circular sulcus, retracting frontal and temporal opercula
- Cruciate opening of dura
- Amygdalohippocampectomy:
- Open temporal horn via inferior circular sulcus, through ~1 cm of tissue in a lateral and basal direction, to expose hippocampus
- Perform amygdalohippocampectomy in subpial fashion
- Disconnect deep white matter following temporal horn to atrium
- Open temporal horn via inferior circular sulcus, through ~1 cm of tissue in a lateral and basal direction, to expose hippocampus
- Suprainsular intraventricular disconnection
- Follow superior limb of circular sulcus anteriorly to disconnect corona radiata fibers passing lateral to the ventricle
- Ipsilateral ventricular system is now exposed
- Follow superior limb of circular sulcus anteriorly to disconnect corona radiata fibers passing lateral to the ventricle
- Corpus callosotomy
- Aspirate through roof of lateral ventricle through corpus callosum to pia of cingulate gyrus
- Follow pericallosal arteries from posterior to anterior to ensure completion of callosotomy
- Aspirate through roof of lateral ventricle through corpus callosum to pia of cingulate gyrus
- Frontal disconnection: connect the interior frontal horn to the frontobasal white matter anterior the middle cerebral artery
- Occipital disconnection: posterior end of the callosal section is extended inferiorly through splenium and occipital white matter
- Insular removal: subpial removal of insular cortex with ultrasonic aspirator
- Closure: standard craniotomy closure
♦ Postoperative
- Intensive care unit
- Continue antiepileptic drugs
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree