Peripheral Nerve and Root Dysfunction
CASE
A 16-year-old male, right-handed high school student is out for the very first time with a girl at a double feature. He has his arm around her and even though it hurts, he doesn’t want to move it. After the show is over, he finds he has aching pain in the midhumerus and cannot extend his wrist or fingers.
Diagnosis
REFLEXES
Reflexes are diminished in root and peripheral nerve disease. There are four primary reflexes to remember, along with the particular roots and muscles necessary for their function. An easy way to learn the roots is to remember that going from ankle to triceps, the roots are numbered consecutively from 1 to 8 (Table 10.1).
ROOTS AND MUSCLES
Each muscle is supplied by two or more roots. Thus, weakness associated with injury to only one root is partial; as opposed to peripheral nerve injury, which may cause complete muscle weakness. Nevertheless, certain muscles tend to be preferentially supplied by certain roots, so that they are particularly affected by injury to the root. Table 10.2 describes the most useful muscles to
test for root injury, and which roots supply each muscle. Each root has a sensory distribution as represented on the standard dermatome chart (see Chapter 34). The most useful root dermatomes to remember are:
test for root injury, and which roots supply each muscle. Each root has a sensory distribution as represented on the standard dermatome chart (see Chapter 34). The most useful root dermatomes to remember are:
TABLE 10.1. Four Primary Reflexes | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
C2—over the posterior head.
C4—the shoulder.
C7—the middle finger.
T4—the nipple.
T10—the umbilicus.
L3—the knee.
S1—the lateral foot.
S3, S4, and S5—the anal region.
TABLE 10.2. Roots and the Primary Muscles They Supply | ||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
NERVES AND MUSCLES OF THE UPPER EXTREMITIES
Median Nerve
The median nerve (C6-T1) originates in the brachial plexus, and supplies two basic muscle groups:
Forearm: pronator of the forearm, radial flexion, and wrist abduction.
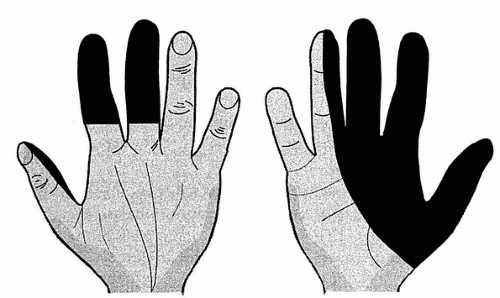
Hand: the first two Lumbricales (index and middle finger flexion at the metacarpophalangeal joint), thumb Opposition with opponens pollicis, Abduction with abductor pollicis brevis, and Flexion with flexor pollicis brevis (“LOAF” muscles). Sensory loss involves the thumb, index, and middle fingers and half of the ring finger (Fig. 10.1).
Clinical comment: A complete median nerve lesion (forearm and hand muscles) is usually secondary to traumatic injury in the axilla, or to a lesion affecting the median nerve at the elbow. Entrapment of the anterior interosseus branch causes weakness of thumb distal flexion, and flexion of the distal phalanx of the second and third digits. Entrapment at the wrist is common after wrist fractures. A clinical syndrome of median entrapment at the wrist with intermittent or progressive symptoms is called “carpal tunnel syndrome.” Patients with this syndrome often complain of numbness and tingling in the thumb and first two fingers. The hands typically “fall asleep” with use or at night (nocturnal paresthesias). The earliest weakness is a difficulty twisting jar lids open or a tendency to drop objects. Muscle wasting and obvious loss of
power occurs later. The diagnosis may be confirmed by nerve conduction studies. Carpal tunnel syndrome is often bilateral and may be associated with systemic processes; consider rheumatoid arthritis, hypothyroidism, diabetes, pregnancy, gout, acromegaly, and amyloidosis. Medical management includes treating the underlying disease, splinting the wrist, and injecting steroids into the carpal tunnel region. A single injection of steroids is beneficial in terms of pain and function at 3 months, but additional injections do not seem to be beneficial. Surgical decompression of the carpal tunnel may be necessary and is usually successful.
power occurs later. The diagnosis may be confirmed by nerve conduction studies. Carpal tunnel syndrome is often bilateral and may be associated with systemic processes; consider rheumatoid arthritis, hypothyroidism, diabetes, pregnancy, gout, acromegaly, and amyloidosis. Medical management includes treating the underlying disease, splinting the wrist, and injecting steroids into the carpal tunnel region. A single injection of steroids is beneficial in terms of pain and function at 3 months, but additional injections do not seem to be beneficial. Surgical decompression of the carpal tunnel may be necessary and is usually successful.
Ulnar Nerve
The ulnar nerve (C8-T1) supplies muscles and sensory areas on the palm not supplied by the median nerve. When ulnar nerve disease is suspected, think of little finger and hypothenar eminence. The ulnar nerve runs in the ulnar groove at the medial aspect of the elbow (“funny bone”) and supplies the following two muscle groups:
Forearm: ulnar flexion at the wrist.
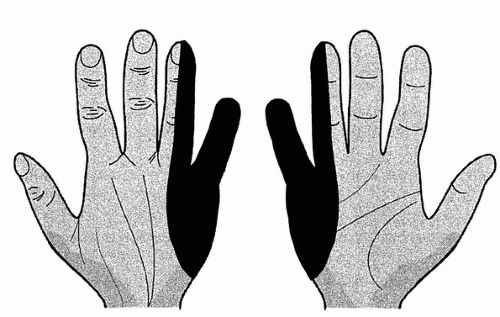
Hand: little finger abduction and opposition, thumb adduction, all the interosseous muscles (used to spread fingers apart and bring together), and third and fourth lumbricales (ring and little finger flexion at the metacarpophalangeal joint). Sensory loss involves half of the fourth finger and the little finger (Fig. 10.2).
Clinical comment: The ulnar nerve is commonly injured at the elbow, where it is most exposed. Look for muscle weakness as opposed to the prominent sensory symptoms seen in median nerve dysfunction.
Radial Nerve
The radial nerve (C5-C8) winds around the humerus in the spiral groove, then travels in the lateral aspect of the elbow. When there is a wrist drop, think of radial nerve injury.
The radial nerve supplies these muscles:
Supinator of the forearm; the brachioradialis reflex may be lost.
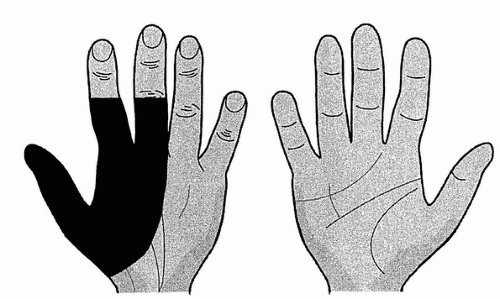
Extensors of the fingers, wrist, elbow (triceps), and thumb. Sensory loss involves the back of the hand and is not always present (Fig. 10.3).
Clinical comment: Injury to the radial nerve may occur in the axilla (e.g., after using crutches), giving inability to extend the elbow, and may include wrist drop. If the radial nerve is involved at the humerus, only wrist drop is found. Pressure palsies are common (e.g., “bridegroom’s palsy,” when the groom sleeps with the bride’s head on his arm).
In addition, the radial nerve is affected in diabetes and lead poisoning. In radial nerve palsy, the ability to spread the fingers apart (ulnar nerve function) may be weak because of the mechanical disadvantage caused by the wrist drop. Check with wrist resting on a flat surface (e.g., table) to overcome that handicap.
THORACIC OUTLET SYNDROME
The thoracic outlet syndrome refers to symptoms and signs that occur, because of compression of the subclavian vessels and brachial plexus at the superior aperture of the thorax between the first rib and the clavicle. Previously thought to be common, it is now clear that true neurogenic or vascular thoracic outlet syndrome is rare. Symptoms include:
Pain and paresthesias in the neck, shoulder, arm, and hand (C8, T1 distribution).
Weakness of the hand; change of color of the hand, including pallor of the fingers.
Aggravation of all symptoms by use of the upper limb.
Signs depend on whether primarily vascular or neural compression exists, and include supraclavicular bruit, loss or diminution of radial pulse, weakness and sensory loss in the hand, and reproduction of pain by pressure in the supraclavicular fossa or by traction on the arm. The diagnosis of thoracic outlet syndrome should be made only when definite nerve conduction or electromyogram data support the neurogenic form, or when there is evidence of vascular disease supporting the vascular form.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree