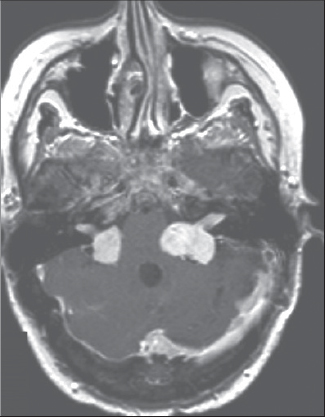
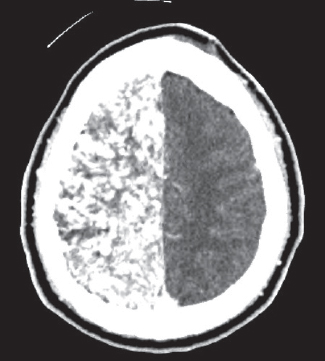
37 What is another name for neurofibromatosis type 1? Von Recklinghausen’s disease What is the incidence of NF1? Approximately 1 in 3000 to 4000 (>90% of NF cases) What is the mode of inheritance? Autosomal dominant What chromosome is the NF1 gene located on? 17q11.2 (mnemonic: 17 letters in “von Recklinghausen”) What is the protein product of the NF1 gene? Neurofibromin What are the three genes embedded within the NF1 gene? EV12A (role unknown), EV12B (role unknown), and OMPG How do somatic mutations affect the outcome of NF1? Segmental NF1; has the same features of NF1, except it is localized to a specific area What is OMPG? Oligodendrocyte myelin glycoprotein. It is found exclusively in the CNS at the time of myelination, and it has antiproliferative activity. What is the function of neurofibromin? • Tumor suppressor (suppresses the ras pathway); may be involved in cognitive and learning abilities It increases GTP hydrolysis, leading to inactivation of p21ras oncoprotein. What segment of neurofibromin inactivates RAS? GAP-related domain (GRD) or exon 23a What are some tumors associated with NF1? • Optic gliomas • Pilocytic astrocytomas • Ependymomas • Primitive neuroectodermal tumors • Malignant peripheral nerve sheath tumors • Hypothalamic gliomas Gliomas have a predilection for what areas? • Optic pathway • Cerebellum • Brainstem What are some other clinical manifestations associated with NF1? • Short stature • Café-au-lait macules • Axillary freckling • Lisch nodules • Macrocephaly • Scoliosis • Cerebrovascular abnormalities • Colonic ganglioneuromas • Hypertension • Epilepsy • Cognitive deficits • Learning disabilities Neurofibromas located at spinal nerve roots can cause what symptoms? • Pain • Muscle weakness • Atrophy • Radiculopathy • Decreased deep tendon reflexes What cerebrovascular abnormalities can occur with NF1? • Cerebral aneurysms • Moyamoya disease • Internal carotid stenosis • Cerebrovascular stenosis What are the variants of NF1? • Cutaneous (most common) • Subcutaneous • Nodular plexiform • Diffuse plexiform (least common) What is elephantiasis neurofibromatosa? A form of neurofibromatosis that is uncommon. A plexiform neurofibroma may grow and subsequently compress adjacent lymphatics and vasculature, causing enlargement of a limb. What cells compose neurofibromas? • Schwann cells • Fibroblasts • Mast cells • Perineural cells • Neurons What are café-au-lait macules? • Flat, hyperpigmented macules • May be present at birth • Usually increase in number as the patient ages What are Lisch nodules? Raised, pigmented hamartomas located in the iris. Two or more of the possible seven diagnostic criteria must be met to diagnose NF1. What are they? • Six or more café-au-lait macules >5 mm in prepubertal patients and >15 mm in postpubertal patients • Two or more neurofibromas of any kind or 1 plexiform neurofibroma • Axillary or inguinal freckling • Two or more Lisch nodules • Optic glioma • Osseous abnormalities • First-degree relative with NF11 What are some osseous abnormalities seen in NF1? • Sphenoidal dysplasia • Congenital tibial pseudoarthrosis • Idiopathic vertebral dysplasia • Thoracic spinal dysplasia with meningocele • Thinning of the long bone cortex By what age is freckling normally seen? By age 4 to 5 What areas are most likely to develop freckling? Most likely to develop in intertriginous areas, such axilla, groin, neckline, or inframammary areas What are cutaneous neurofibromas? Superficial tumors arising from the peripheral nerve sheath How do they present? Present as soft, fleshy, dermal lesions that appear around adolescence Are cutaneous neurofibromas malignant or benign? Benign Do cutaneous neurofibromas have malignant potential? No How do subcutaneous neurofibromas present? They usually present around adolescence as firm, tender nodules that run along with peripheral nerves. How do nodular plexiform neurofibromas present? These appear at proximal nerve roots and can be painful. Because of the close proximity to the spinal cord, growth can lead to vertebral erosion and subsequent compression of the spinal cord. How do diffuse plexiform neurofibromas present? These are considered to be congenital lesions that may have concurrent hyperpigmentation at the site of the neurofibroma. What are some possible complications of surgical debulking of a plexiform neurofibroma? • Due to the proximity of nerve roots and the spinal cord, excision or debulking of the neurofibroma can lead to nerve damage. • Propensity for neurofibromas to be extremely vascular; therefore, surgical debulking or excision can lead to excessive operative bleeding. Do plexiform neurofibromas have any malignant potential? Yes What do they transform to? Malignant peripheral nerve sheath tumors What is another name for malignant peripheral nerve sheath tumors? Neurofibrosarcoma. How do malignant peripheral nerve sheath tumors present? • Sudden change in level of pain • Increase in size • Change in consistency What is the best way to diagnose a malignant peripheral nerve sheath tumor? A biopsy of hypermetabolic areas shown by 18-fluorodeoxyglucose positron emission tomography (PET) scan What are possible treatments for malignant peripheral nerve sheath tumors? • Surgical excision • Radiotherapy to the operative site • Chemotherapy for metastases How are optic gliomas screened for? Patients with NF1 should undergo regular, thorough ophthalmologic examinations and growth assessment. Growth assessment is important because an optic glioma can involve the hypo thalamus and thus affect puberty. If a patient develops clinical signs suggestive of an optic glioma, MRI is indicated. Is screening with MRI for optic gliomas useful? Screening MRIs may be useful in certain age groups where a thorough ophthalmologic examination is difficult to conduct. What is an UBO? Unidentified bright object. UBOs are seen on T2-weighted images in patients with NF1. They are thought to be caused by an increase in fluid or myelin in an area of dysplastic glial proliferation. Where are UBOs found? Found in the cerebellum, basal ganglia, brainstem, and subcortical white matter Some researchers have claimed that UBOs are associated with what? The presence and severity of cognitive and intellectual impairment What form of leukemia are patients with NF1 at risk for? Chronic myeloid leukemia What is a rare renal complication associated with NF1? Renal artery stenosis What is the incidence of NF2? Approximately 1 in 30,000 to 40,000 What is the mode of inheritance? Autosomal dominant What chromosome is the NF2 gene located on? 22q11.2 (mnemonic: 22 characters in “neurofibromatosis type 2”) What is the protein product of the NF2 gene? Merlin Where is merlin found? Schwann cells, meningeal cells, peripheral neurons, eye lens What is the function of merlin? Tumor suppressor How does it work? It binds to CD44 and actin, contributing to cell-matrix interaction. These interactions are used to control cell growth via contact inhibition. A deficiency in physiological merlin leaves the cells insensitive to other cells and allows unregulated growth. What are some clinical features of NF2? • Bilateral vestibular schwannomas • Fewer neurofibromas than NF1 • Fewer café-au-lait macules than NF1 • Tinnitus • Hydrocephalus • Sensory deficits • Cataracts • Dysequilibrium2 Fig. 37.1 T1-weighted MRI with contrast showing bilateral vestibular schwannomas in a patients with NF2. What criteria are required to make a definitive diagnosis NF2? • Bilateral vestibular schwannomas, or • Positive FMHx plus unilateral vestibular schwannoma before 30 years of age, or two of the following: meningioma, schwannoma, glioma, neurofibroma, juvenile posterior subcapsular lenticular opacity, cerebral calcification2 What criteria are required to make a probable diagnosis of NF2? • Unilateral vestibular schwannoma before 30 years of age, plus one or more of the following: meningioma, schwannoma, glioma, juvenile posterior subcapsular lenticular opacity, or • 2 or more meningiomas plus unilateral vestibular schwannoma before 30 years of age or one of the following: schwannoma, glioma, neurofibroma, juvenile posterior subcapsular lenticular opacity, cerebral calcification2 What are some nonneoplastic lesions associated with NF2? • Meningioangiomatosis (proliferations of meningeal cells and blood vessels) • Glial hamartomata What are some associated tumors seen in NF2? • Cranial meningiomas • Spinal meningiomas • Ependymomas • Astrocytomas What is a Verocay body? Regions in between nuclear palisading that are relatively nuclear free This histological characteristic is found in what tumor? Schwannoma What are the variants of NF2? • Gardner (mild) • Melanotic • Multinodular plexiform • Wishart (severe) What is the genetic mutation causing Gardner? • Single codon mutation • Merlin retains some tumor-suppressing activity What is the genetic mutation causing Wishart? • Severe truncation of the gene • Symptoms usually develop before 20 years of age • Usually present with multiple tumors How does the Wishart variant differ histologically? No Antoni B or Verocay bodies How does NF2 mosaicism present? • Features localized to one area • Ipsilateral vestibular schwannomas • Ipsilateral meningiomas When should genetic testing for NF2 be offered? When there is confirmed NF2 mutation in the family or uncertainty about the diagnosis What tests should be conducted in the screening process for NF2? • Annual ophthalmologic examination • Annual neurological examination • Inspection of skin • Brain MRI every 2 years from 10 to 20 years of age and then every 3 years until 40 years of age • Spine MRI every 3 years if needed What is schwannomatosis? Multiple nonvestibular schwannomas caused by defect in INI-1 gene What criteria are required to make a definitive diagnosis of schwannomatosis? • Greater than 30 years of age • Two or more nonintradermal schwannomas • Histological confirmation of schwannoma • First-degree relative with schwannomatosis What criteria are required to make a probable diagnosis of schwannomatosis? • Less than 30 years of age, two or more nonintradermal schwannomas, histological confirmation • Greater than 45 years of age, two or more nonintradermal schwannomas, histological confirmation, and no CN VIII palsy What is the incidence? 1 in 40,000 What is the mode of inheritance? Autosomal dominant3 What is the mutated gene responsible for this syndrome? pVHL On what chromosome is this gene located on? 3p25–26 What is the function of the pVHL gene? • Tumor suppressor • Aids in protein degradation • pVHL is a regulatory subunit for elongin. Elongin normally pauses the normal transcription function of RNA polymerase II at multiple sites by binding with pVHL. Therefore, the VHL-Elongin complex acts as a tumor supressor by inhibiting transcription elongation. Mutations in pVHL allow unregulated transcription of growth factors. • pVHL also acts as a facilitator for ubiquitin-mediated degradation by tagging proteins with ubiquitin. pVHL targets transcription factors, which provides regulated transcription of growth factors. A mutated pVHL leads to an excess of transcriptions factors, leading to increased growth factors. What are some of the growth factors regulated by pVHL? • Hypoxia-inducible factor 1α • Vascular endothelial growth factor • Platelet derived growth factor-β • Transforming growth factor-α • Matrix metalloproteinases • Matrix metalloproteinase inhibitors • Atypical protein kinase C What are the screening criteria? • A relative diagnosed with VHL by gene analysis • Individual with a VHL-associated lesion and family history of VHL-associated lesions • Individual with two or more VHL-associated lesions What do VHL-associated lesions consist of? • Hemiangioblastomas • Retinal angiomas • Clear-cell renal cell carcinomas • Endolymphatic sac tumors of the middle ear • Neuroendocrine and serous cystadenomas of the pancreas • Papillary cystadenomas of the epididymis and broad ligament4,5 What is the most common VHL-associated lesion? Hemangioblastomas In relation to the tentorium, where do hemangioblastomas seen in VHL occur? Infratentorial Are they usually solitary or multiple? Multiple What are some possible complications of retinal angiomas? • Retinal detachment • Loss of vision • Glaucoma What are some possible sequelae of endolymphatic sac tumors of the middle ear? • Hearing loss • Tinnitus • Vertigo • Facial muscle weakness What is the most frequent cause of the death in VHL? Renal cell carcinoma There are multiple types of VHL. What are they based on? • Development of pheochromocytoma • Development of renal cell carcinoma What are the types? • Type I • Type IIA • Type IIB • Type IIC6 What are the characteristics of type I? • No pheochromocytoma • High risk for VHL-associated lesions What are the characteristics of type IIA? • High risk of pheochromocytoma • Low incidence of renal cell carcinoma What are the characteristics of type IIB? • High risk of pheochromocytoma • High incidence of renal cell carcinoma What are the characteristics of type IIC? Pheochromocytomas only For patients under the age of 11, annual examinations should include what? • Ophthalmological examination • Catecholamine levels For adolescents, annual examinations should include what? • Ophthalmological examination • Catecholamine levels • Abdominal CT for pheochromocytoma • MRI of brain and spine for hemangioblastoma For adults, annual examinations should include what? • Ophthalmological examination • Catecholamine levels • Abdominal CT • Abdominal MRI for renal cell carcinoma • MRI of brain and spine • Ear, nose, and throat with auditory examination What is the incidence of tuberous sclerosis? 1 in 6000 to 10,0007 What is the mode of inheritance? Autosomal dominant What gender is tuberous sclerosis most often seen in? No gender predilection What cardiac anomaly is associated with tuberous sclerosis? Rhabdomyomas What are the genes involved? • TSC1 • TSC2 What chromosome is the TSC1 gene located on? 9q34 What is the product of TSC1 gene? Hamartin What chromosome is the TSC2 gene located on? 16p13.3 What is the product of TSC2 gene? Tuberin Which gene, when mutated, causes a less severe form? TSC1 How does hamartin work? • Stabilizes tuberin • Activates GTPase Rho • Interacts with cyclins and cyclin-dependent kinases • Tuberin stimulates GTPase activity → hydrolysis of Rap1a (Ras-like protein) → inactivation of Rap1a → regulated cell growth • Interacts with cyclins and cyclin-dependent kinases What are the major features? • Facial angiofibroma or forehead plaque • Atraumatic ungual/periungual fibroma • Shagreen patch • Three or more ash-leaf spots • Multiple retinal nodular hamartomas • Cortical tubers • Subependymal nodule • Subependymal giant cell astrocytomas • Cardiac rhabdomyoma • Lymphangioleiomyomatosis • Renal angiomyolipoma8 What are the minor features? • Multiple dental enamel pits • Hamartomatous rectal polyps • Bone cysts • Cerebral white matter migration lines • Gingival fibromas • Nonrenal hamartomas • Retinal achromic patch • Confetti-like skin lesions • Multiple renal cysts8 Which features are needed to make a definitive diagnosis? Two major features, or one major feature and two minor features8 Which features are needed to make a possible diagnosis? One major feature and one minor feature8 Which features are needed to make a probable diagnosis? One major feature or two minor features8 What is a shagreen patch? • Subepidermal fibrosis • Orange peel-like texture • Usually in lumbosacral region What is an ash-leaf spot? • Hypomelanocytic macule • Usually elliptical in shape Another name for angiofibromas is? • Fibroadenomas • Usually with malar distribution What are seizures most likely caused by? Cortical tubers How do these seizures normally present? How do they progress? They initially present as myoclonic seizure but later progress to tonic-clonic seizure or partial complex seizures (depends on tuber location). What are five different renal lesions seen? • Benign angiomyolipoma • Renal cysts • Malignant angiomyoliposarcoma • Oncocytoma • Renal cell carcinoma What is Vogt’s triad? • Seizures • Mental retardation • Facial angiofibromas What are some vascular abnormalities associated with tuberous sclerosis? • Coarctation of aorta • Renal artery stenosis • Aortic aneurysm What is the most common renal abnormality? Angiomyolipomas Histologically, what are cortical tubers composed of? • Enlarged atypical neuronal elements • Glial elements • Astrocytosis Another name for cortical tubers is? Glioneuronal hamartomas Histologically, what are subependymal nodules composed of? • Atypical enlarged glial cells • Atypical enlarged neuronal cells What are the features of SWS? • Facial angiomas (port-wine stain) • Facial nevus • Glaucoma • Choroid hemangiomas • Conjunctival angiomas • Episcleral angiomas • Retinal detachment • Strabismus • Buphthalmos • Parieto-occipital leptomeningeal venous angiomatosis • Enlarged deep/collateral cerebral veins • Reduced/absent cortical veins • Seizures • Mental retardation • Hemiparesis • Visual field defects • Heterochromia of the iris • Focal neurological deficits Facial angiomas are usually found along what nerve distribution? V1 and V2 regions of the trigeminal nerve What are the characteristics of a facial angioma in a newborn? • Flat • Salmon colored How does the facial angioma change as the patient ages? • Dark red • Vascular ectasias • Nodularity • Superficial blebbing Facial angiomas involving upper and lower eyelids increase the possibility of what feature associated with SWS? Parieto-occipital leptomeningeal venous angiomatosis Fig. 37.2 Axial CT with contrast in patient with Sturge-Weber syndrome showing extensive serpentine leptomeningeal enhancement involving one hemisphere.
Phakomatoses and Neurocutaneous Disorders
37.1 Neurofibromatosis Type 1 (NF1)
37.2 Neurofibromatosis Type 2 (NF2)
37.3 Schwannomatosis
37.4 Von Hippel–Lindau Syndrome (VHL)
37.5 Tuberous Sclerosis Complex
37.6 Sturge-Weber Syndrome (SWS)
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






