Chapter 25 Posterior Approach to the Thoracic Spine
TOTAL EN BLOC SPONDYLECTOMY—THORACIC SPINE
INDICATIONS
En bloc spondylectomy is the treatment of choice for solitary and oligometastatic spinal metastases, with biologically favorable histological findings.1 In appropriately selected patients, neurological outcome, pain control, and oncological control are significantly better after en bloc spondylectomy compared with radiation therapy. Oncological outcomes also exceed those of intralesional techniques. Total en bloc spondylectomy (TES) decreases the rate of local recurrence and can provide long-term survival in selective patients with spinal metastasis.2
SURGICAL TECHNIQUE
Total spondylectomy is performed through the posterior procedure alone or through the anteroposterior combined procedure. The TES technique consists of two steps: en bloc resection of the posterior element and en bloc resection of the anterior column.1,3
En Bloc Resection of the Posterior Element of the Vertebra by Posterior Approach
Exposure
The patient is placed in a prone position over a four-poster frame to prevent compression to the vena cava. A straight, vertical, midline incision is made over the spinous processes and is extended three vertebrae above and below the involved segments. The paraspinal muscles are dissected from the spinous processes and the laminae, and then retracted laterally over the facet joint. After a careful dissection, a large retractor is applied. The surgical field must be wide enough on both sides to allow for dissection under the surface of the transverse processes. In the thoracic spine, the ribs on the affected level are transected 3–4 cm lateral to the costotransverse joint, and the pleura is separated bluntly from the vertebra. To expose the superior articular process of the uppermost vertebra, the spinous and the inferior articular processes of the neighboring vertebra are osteotomized and removed with dissection of the attached soft tissues, including the ligamentum flavum (Fig. 25-1). After the spinous process, lower part of lamina, and inferior facet are removed, the dorsal dura is exposed.3,4
INTRODUCTION OF THE T-SAW GUIDE
Using blunt-tipped dissectors, the soft tissue attached to the inferior aspect of the pars interarticularis is dissected and removed to prevent damage to the corresponding nerve root. A c-curved, malleable, T-saw guide is then introduced through the intervertebral foramen in a cephalocaudal direction.3 In this procedure, the tip of the T-saw guide should be introduced along the medial cortex of the lamina and the pedicle so that the spinal cord and the nerve root are not injured. After the T-saw guide is passed, its tip at the exit of the nerve root canal can be found beneath the inferior border of the pars interarticularis. In the next step, a flexible threadwire saw (0.54 mm in diameter) is passed through the hole in the T-saw guide and is clamped at each end. The T-saw guide is removed, and tension on the threadwire saw is maintained. This procedure also is applied to the contralateral side.
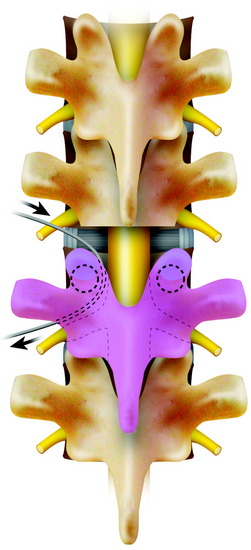
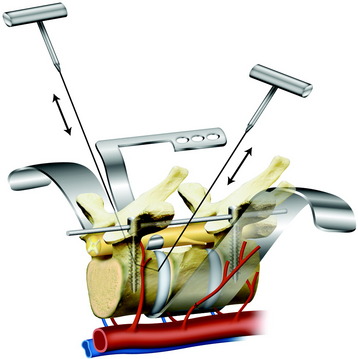
CUTTING THE PEDICLES AND RESECTION OF THE POSTERIOR ELEMENT
While tension is maintained, the threadwire saw is placed beneath the superior articular and transverse processes. With this procedure, the saw placed around the lamina is moved to around the pedicle. With a reciprocating motion of the saw, the pedicles are cut, and then the whole posterior element of the spine (the spinous process, the superior and inferior articular processes, the transverse process, and the pedicle) is removed in one piece (Fig. 25-2). The cut surface of the pedicle is sealed with bone wax to reduce bleeding and to minimize contamination by tumor cells.
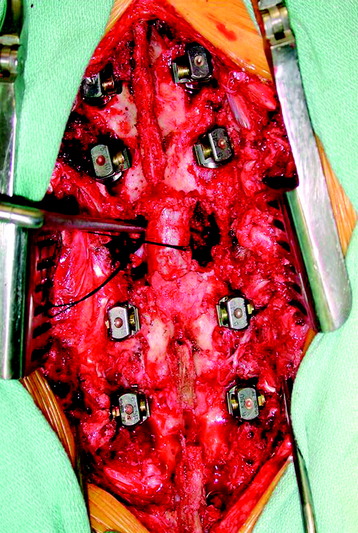
If the unilateral pedicle is affected by the tumor, osteotomy is performed through a healthy lamina, and the cut surface is blocked with bone wax immediately after osteotomy. The threadwire saw is passed under the lamina in a sublaminar fashion after carefully dissecting a passageway for it in the epidural space. If the tumor invades the bilateral pedicles and the pedicle and lamina, an electric cautery knife is inserted into the affected pedicle to coagulate tumor tissue inside the pedicle before pediculotomy to prevent tumor cell contamination. In these cases, the nerve root involved sometimes has to be ligated and included into the tumor mass. If the affected pedicle or vertebral body markedly compresses the nerve root, the more severely affected side is sacrificed. In the thoracic regions, the nerve root can be sacrificed without any functional deficit, except for the T1 nerve root.5 After the posterior bony column is removed, the epidural and foraminal vessels are meticulously coagulated using bipolar coagulator. Before the anterior column is resected, a posterior instrumentation should be performed (Fig. 25-3).
En Bloc Corpectomy By Posterior Approach
POSTERIOR LIGAMENTOUS RELEASE OF THE VERTEBRAL BODY
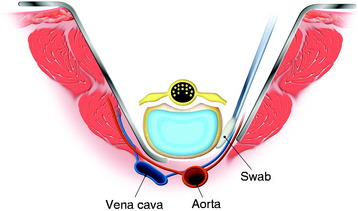
At the beginning of the second step, the segmental arteries must be identified bilaterally. The spinal branch of the segmental artery, which runs along the nerve root, is ligated and divided. This procedure exposes the segmental artery, which appears just lateral to the cut edge of the pedicle. In the thoracic spine, the nerve root is cut on the side from which the affected vertebra is removed. The blunt dissection is performed anteriorly on both sides through the plane between the pleura (or the iliopsoas muscle in lumbar spine) and the vertebral body. Usually, the lateral aspect of the body is dissected easily with a curved vertebral spatula. Then the segmental artery should be dissected from the vertebral body. To aid with retraction of paraspinal structures, cottonoids or rolled gauze pads can be inserted between the vertebra and laterally dissected tissue. By continuing dissection of both lateral sides of the vertebral body anteriorly, the aorta is carefully dissected posteriorly from the anterior aspect of the vertebral body with a spatula and the surgeon’s fingers. After dissection of the lateral surface, the dural sac is freed from the posterior longitudinal ligament (PLL), and the medial portion of the annulus fibrosus is sharply divided with a knife under direct visualization (Fig. 25-4). For the anterior release of great vessels from the anterior longitudinal ligament, blunt finger dissection is applied. After the potential space has undergone finger dissection, a series of spatulas, starting from the smallest size, is inserted sequentially to extend the dissection. A pair of the largest spatulas is kept between the anterior surface of the vertebral body and great vessels to maintain the dissected space and to make the surgical field wide enough for manipulating the anterior column.
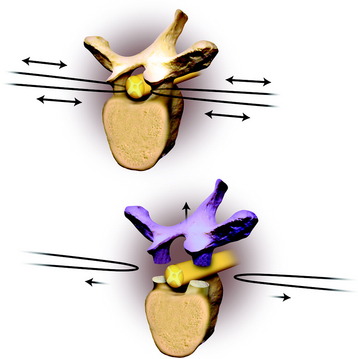
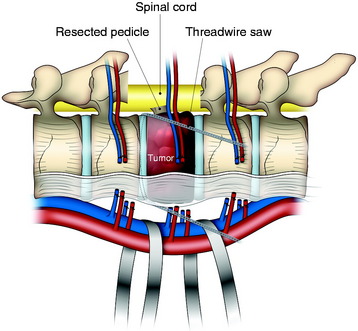
DISSECTION OF THE SPINAL CORD AND REMOVAL OF THE VERTEBRA
Using a cord spatula, the spinal cord is mobilized from the surrounding venous plexus and the ligamentous tissue. The cord protector, which has teeth on both edges to prevent the threadwire saw from slipping, is then applied. The anterior and posterior longitudinal ligaments are cut by the threadwire saw. After cutting the anterior column, the mobility of the vertebra is checked again to ensure a complete corpectomy. The freed anterior column is rotated around the spinal cord and removed carefully. With this procedure, a complete anterior and posterior decompression of the spinal cord (circumferential decompression) and total en bloc resection of the vertebral tumor are achieved (Fig. 25-5).
Corpectomy With Anterior Approach
Anterior column removal can be done with a separate incision after position change.
If the posterior ligamentous release procedure is complete, the anterior procedure is easy. The lateral approach is favored. The ipsilateral segmental vessels are identified and dissected off from the vertebral body. The elevation of the segmental vessels makes it easy to dissect the great vessels from the anterior longitudinal ligament. After the great vessels are away from the anterior longitudinal ligament, contralateral segmental vessels are seen. They can be dissected away from the vertebral body surface. All the vascular structures are kept off the vertebral body, which means the vertebral body is freed from the surrounding structures. Proximal and distal discs are removed with a knife or threadwire saw (Fig. 25-6).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree