♦ Preoperative
Operative Planning
- Review imaging
- Computed tomography (CT)
- Severity of subarachnoid hemorrhage may indicate the degree of brain edema
- Presence of temporal lobe hematoma may indicate projection above the tentorial edge
- Presence and degree of hydrocephalus may indicate need for ventricular drain
- Location and size of the frontal sinus affect the design of the bone flap
- Severity of subarachnoid hemorrhage may indicate the degree of brain edema
- Computed tomography angiogram
- Demonstrates the sac size, presence of lobulations or daughter sacs, neck width
- Demonstrates dome projection lateral, posterior, or medial
- Location of the posterior communicator in relationship to the sac; presence or absence of an ipsilateral P1 segment to suggest a fetal or near fetal PCOM artery circulation pattern
- Presence of calcification/atherosclerosis within the neck/dome of the aneurysm
- Presence of additional aneurysms ipsilateral to the posterior communicator
- Demonstrates the sac size, presence of lobulations or daughter sacs, neck width
- Digital subtraction cerebral angiogram (DSA)
- Indicates the size, dome projection, aneurysm morphology with presence of daughter sacs, neck size
- Presence of fetal or near fetal circulation pattern
- Location of the anterior choroidal artery in relation to aneurysm neck
- Important to differentiate angiographically between PCOM artery aneurysm and superior hypophyseal artery aneurysm (proximal control may be more difficult in the latter; thus, consider prepping the extracranial carotid in the neck)
- Presence of additional aneurysms ipsilateral to the posterior communicator
- Indicates the size, dome projection, aneurysm morphology with presence of daughter sacs, neck size
- Computed tomography (CT)
- Tapered teardrop occluder suckers (Fukushima [PMT Corporation, Chanhassen, MN] type)
- Aneurysm clips, standard and fenestrated (Aesculap titanium)
- Temporary aneurysm clips
- Rhoton dissectors
- Bipolar and Bovie electrocautery
- Arachnoid knife (no. 10 Beaver blade)
- Intraoperative micro-Doppler
- Electroencephalogram/somatosensory evoked potential/motor evoked potential monitoring
- Intraoperative angiography (particularly with large complex aneurysms with fetal circulation anatomic configuration by angiogram)
Operating Room Set-up
- Operating microscope: mouthpiece for small focus adjustments during dissection; if observer head is used, consider the relationship of the microscope and the scrub nurse and the assistant to minimize interference
- Electric operating room table
Anesthetic Issues
- Mild hyperventilation, pCO2 to 30 to 32 mm Hg
- Intravenous (IV) dexamethasone (10 mg) prior to incision
- IV oxacillin 2 gm IV every 6 hours (alternatively vancomycin 1 gm IV every 12 hours) administered 30 minutes prior to incision
- IV mannitol 0.5 to 1 gm administered at the time of the skin incision for brain relaxation (consider lower dose in unruptured cases to avoid volume depletion)
- Continue anticonvulsants if started presurgery (loading in the operating room is not routine but based on clinical circumstances)
- Careful monitoring of blood pressure at the time of Mayfield head holder placement
- For patients with subarachnoidal hemorrhage (SAH) and no spasm or unruptured cases, systolic blood pressure is maintained at 120 to 140 mm Hg during the procedure
- Slightly increased pressure for patients at risk for or with evidence of vasospasm and for periods of temporary occlusion
- Routine placement of arterial line and Foley catheter
- Central line access for ruptured aneurysms or complex cases
- Anticipation of the pharmacological need for burst suppression in the setting of premature aneurysmal rupture or for routine temporary occlusion
♦ Intraoperative
External Ventricular Drain
- Can be placed prior to positioning for the pterional craniotomy once the craniotomy has been performed
- Inferior/middle frontal gyrus (Paine’s point) intraoperative external ventricular drainage (EVD)
- Create a triangle with a paper ruler 2.5 cm on a side. Place the base of the triangle along the sylvian fissure abutting the partially resected sphenoid wing.
- Insert the EVD at the apex of the triangle at a right angle to the cortex, cannulating the frontal horn of the ventricle at 4 to 5.5 cm depth
- Create a triangle with a paper ruler 2.5 cm on a side. Place the base of the triangle along the sylvian fissure abutting the partially resected sphenoid wing.
Positioning
- The patient is supine with the head fixed in the Mayfield head holder, single pin in the contralateral frontal region, two pins in the occipital area, 60 to 80 pounds of pressure
- The head is rotated 20 to 30 degrees to the contralateral side and the neck is extended 10 to 15 degrees (rotation of the head > 30 degrees brings the temporal lobe more into the field and may necessitate temporal lobe retraction)
Pterional Craniotomy
Initial Dissection
- Goal: proximal control of the internal carotid artery (ICA)
- Steps
- Assemble and position self retaining retractor arm in anticipation of frontal lobe retraction
- Line the frontal lobe superior to the sylvian fissure with protective nonstick pledgets (Adaptic [Johnson & Johnson, New Brunswick, NJ] or Telfa)
- Under the operative microscope, with one hand controlling the regulated suction and the other manipulating the retractor, gently and gradually advance the retractor to elevate the frontal lobe, identifying the optic nerve
- Release with sharp dissection the arachnoid bands tethering the optic nerve to the frontal lobe using a no. 10 Beaver blade, a Rhoton no. 6 dissector, and fine bayoneted scissors
- Dissect laterally into the opticocarotid triangle medial to the carotid, releasing cerebrospinal fluid (CSF). Clear a space for the medial blade of a temporary clip.
- Dissect the arachnoid layer laterally over the carotid proximal to the posterior communicator for the lateral blade of the temporary clip
- Assemble and position self retaining retractor arm in anticipation of frontal lobe retraction
Initial Exposure of the Aneurysm Neck
- Goal: distal carotid exposure to the carotid bifurcation without undue stress on the aneurysm sac
- Steps
- Continue arachnoid dissection distally along the medial boarder of the carotid
- Gently reposition the retractor on the frontal lobe just medial to the carotid and stretch the thick bridging frontotemporal arachnoid bands, dividing them sharply
- Identify the origin of the middle cerebral artery at the carotid bifurcation
- Gently dissect from distal to proximal from the bifurcation along the lateral aspect of the carotid and identify the origin of the anterior choroidal artery
- Continue proximal dissection to identify the origin of the distal neck
- Start proximally along the lateral carotid just distal to the anterior clinoid and dissect distally until the origin of the proximal neck is identified
- Continue arachnoid dissection distally along the medial boarder of the carotid
Full Identification of the Relevant Anatomy Prior to Clipping
- Goals: identification of the posterior communicator, identification of the course of the anterior choroidal artery and clearing it from the path of clipping, and identification of the third nerve and clarifying its relationship to the neck
- Steps
- Deepen the arachnoidal dissection along the medial carotid to obtain a look posterior to the carotid
- With a no. 6 Rhoton or fine suction, gently retract the carotid laterally in an attempt to identify the PCOM artery and any medially projecting aneurysm sac
- Explore the distal neck with a no. 6 Rhoton dissector, developing a plane by gently mobilizing the carotid medially, which will provide a look at the distal posterior medial sac (Fig. 22.1). If the origin of the anterior choroidal artery is close to the neck, follow it deep, sweeping it away from the sac. It may be possible to get a look at the communicator through this dissection window.
- If the aneurysm projection is favorable, dissect laterally along the neck and deepen the dissection to identify the proximal third nerve
- Deepen the dissection plane proximally and identify the origin of the communicator by gently compressing the aneurysm sac just lateral to the proximal neck
- By dissecting carefully laterally from the identified origin of the communicator, the third nerve as it enters the tentorial dura can often be visualized. Temporary proximal clipping under burst suppression may assist in softening the aneurysm, allowing for a more complete look.
< div class='tao-gold-member'>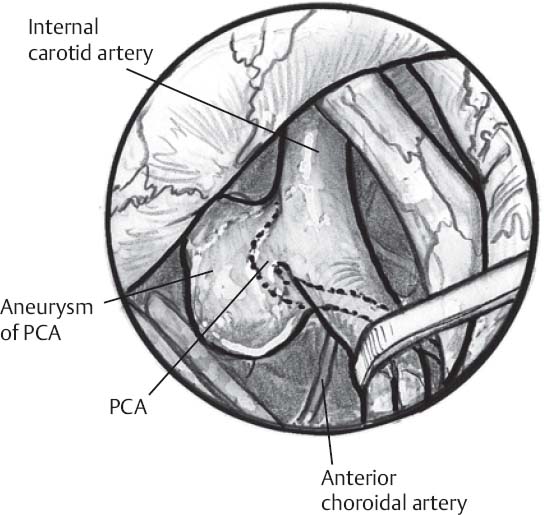 Only gold members can continue reading. Log In or Register to continue
Only gold members can continue reading. Log In or Register to continue
- Deepen the arachnoidal dissection along the medial carotid to obtain a look posterior to the carotid








