Anterior, middle, and posterior cranial fossae
Microvascular Decompression
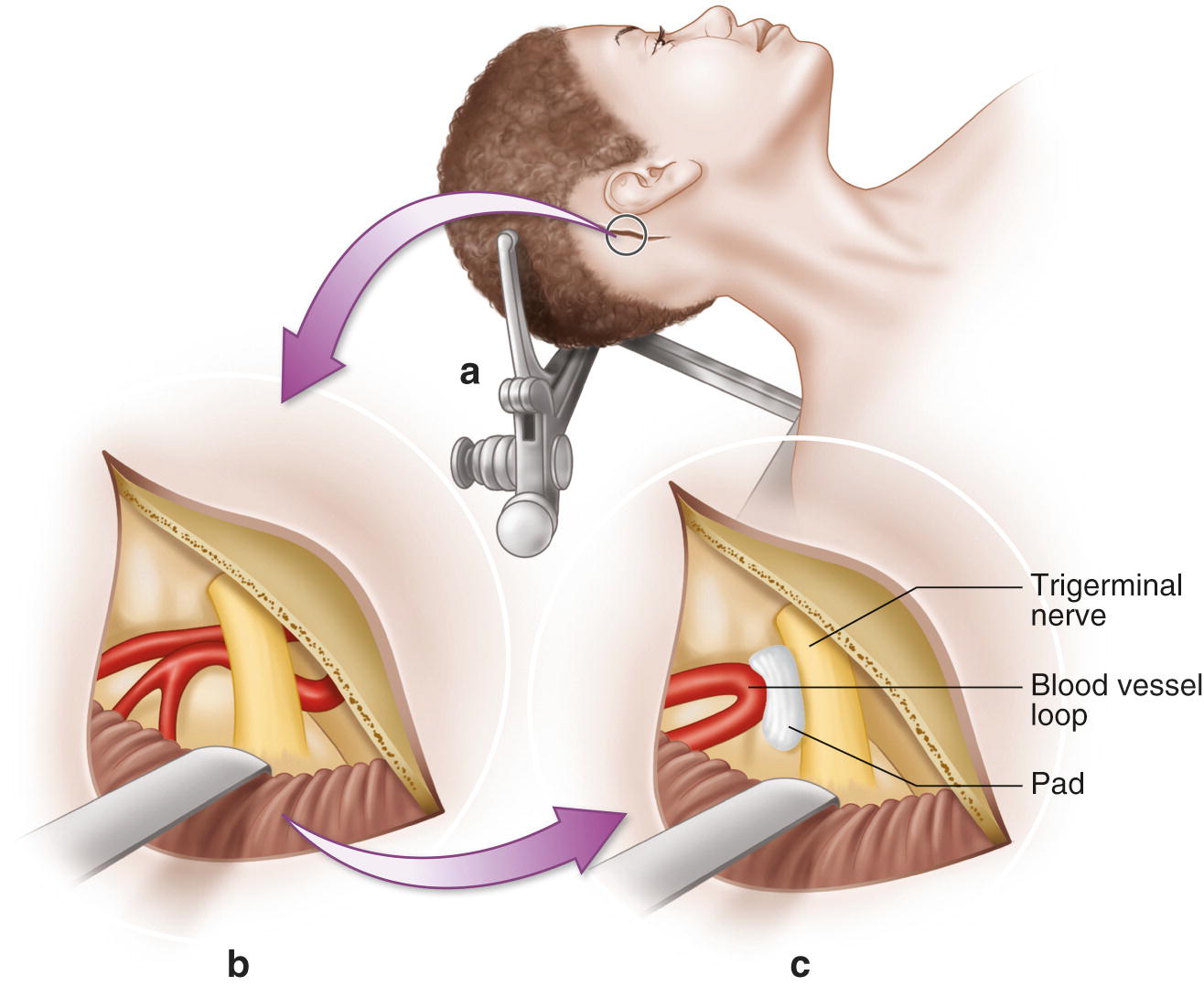
Microvascular decompression. (a) Access to the trigeminal or facial nerve is accomplished through a posterior fossa craniotomy. (b) The cerebellum is retracted exposing the nerve and the offending blood vessel. (c) A Teflon pad is placed between the nerve and vessel, decompressing the nerve
During surgery to address cranial neuralgias, surgeons typically opt to monitor the trigeminal nerve (CNV) and the facial nerve (CNVII), using free-running EMG and triggered EMG. The trigeminal nerve is monitored by placing needle electrodes in the masseter or temporalis muscle. Facial nerve monitoring is accomplished by placing electrodes in the muscles of the five main branches of CNVII that control facial expression: temporal, zygomatic, buccal, marginal mandibular, and cervical. EMG monitoring is helpful in locating the cranial nerves and determining adequate decompression. A complication of MVD surgery is ipsilateral hearing loss from injury to the vestibulocochlear nerve. Brainstem auditory evoked potentials (BAEPs) are used to help prevent injury to CNVIII due to traction, ischemia, or cautery. BAEPS are also utilized when there is a risk of brainstem ischemia associated with manipulation of the cerebellum.
Trigeminal neuralgia , also known as tic douloureux , is an inflammation of the trigeminal nerve causing extreme pain and muscle spasms in the face. The trigeminal nerve functions in sensing facial touch, pain, and temperature, as well as controlling muscles used for chewing. Attacks of intense, electric shock-like facial pain can occur without warning or be triggered by touching specific areas of the face. The trigeminal nerve has three major branches. The ophthalmic, or upper, branch supplies sensation to most of the scalp, forehead, eye, and eyebrow. The maxillary, or middle, branch passes through the cheek, upper jaw, top lip, teeth and gums, and to the side of the nose. The nerve’s mandibular, or lower, branch passes through the lower jaw, teeth, gums, and bottom lip. More than one nerve branch can be affected by the disorder. The superior cerebellar artery (SCA) is the vessel most often responsible for neurovascular compression of the trigeminal nerve root, although other arteries or veins may be the culprit vessels [1]. BAEPs and EMG for CNV and CNVII are typical modalities used for monitoring of MVD to relieve trigeminal neuralgia. The t-EMG response for CNV can easily be confused with CNVII responses. The latency of a t-EMG response from the trigeminal nerve should be around 5 ms, while a facial nerve response is seen around 7 ms when stimulated near the exit point from the brainstem. This should be very easy to remember!
Hemifacial spasm (HFS) is characterized by intermittent, involuntary twitching of the muscles in one side of the face, which lasts from a few seconds to several minutes. Spasms occur spontaneously and without warning. They are often exacerbated by stress or fatigue but can also be triggered by stimuli like sunlight, touch, chewing, and talking. Spasms do not cause pain, but can cause discomfort, impaired vision, social distraction, and embarrassment. HFS is most often caused by a branch of the posterior inferior cerebellar artery (PICA) or anterior inferior cerebellar artery (AICA), pulsating against the facial nerve root as it leaves the brainstem, resulting in hyperactivity of the facial nerve [1, 2]. Similar to the treatment for trigeminal neuralgia, in order to relieve HFS symptoms the facial nerve must be moved away from the offending vasculature.
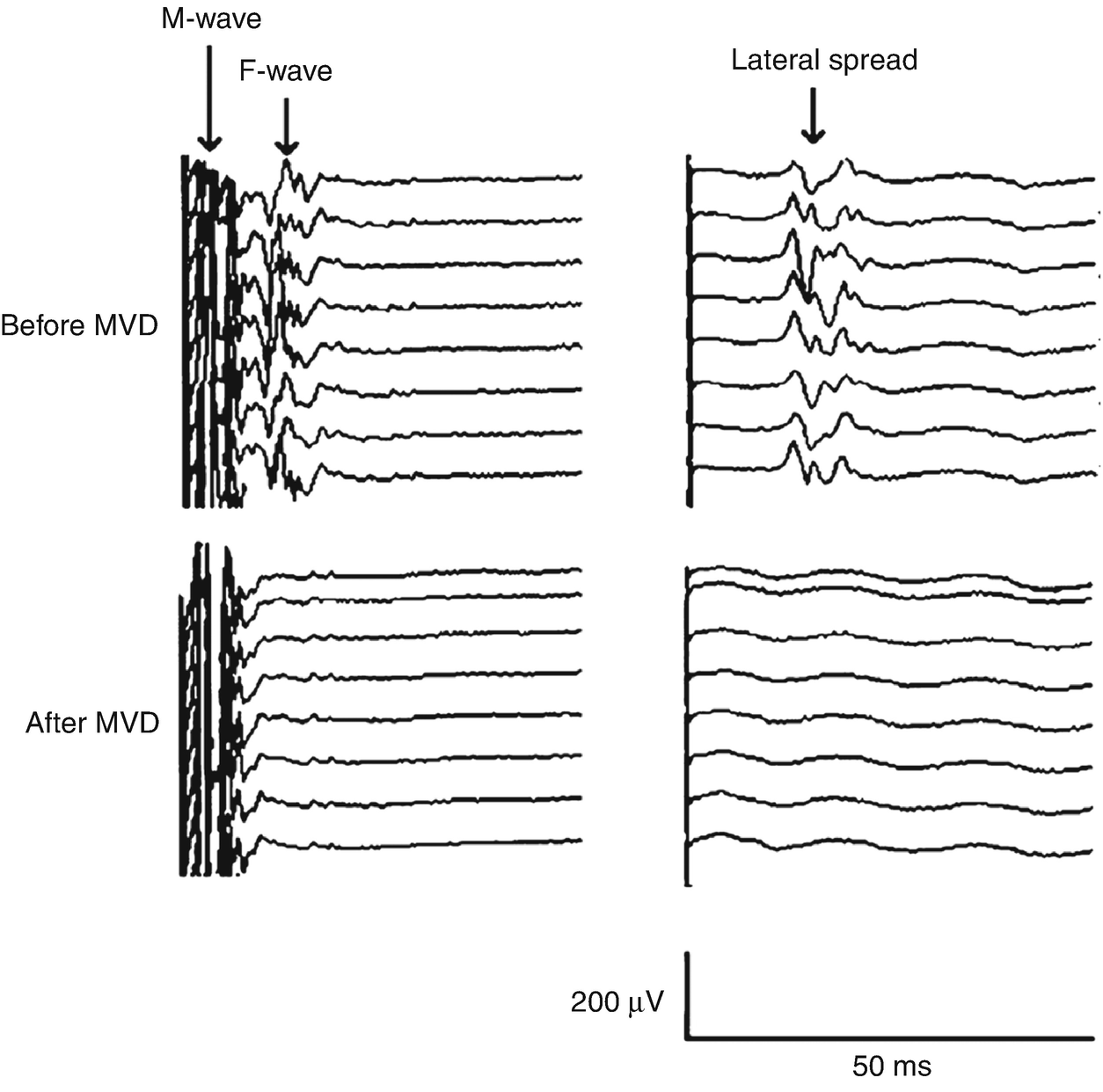
Recordings of LSR and F wave were obtained after direct stimulation of marginal mandibular branch (left column) showing LSR to the orbicularis oculi muscle (right column). Simultaneous disappearance of the LSR and F wave after MVD was achieved. (Reprinted with permission from Fernández-Conejero et al. [16])

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







