Posterior Fossa Neoplasm, Pediatric
Susan I. Blaser, MD, FRCPC
DIFFERENTIAL DIAGNOSIS
Common
Pilocytic Astrocytoma
Medulloblastoma (PNET-MB)
Ependymoma
Brainstem Glioma, Pediatric
Less Common
Ganglioglioma
Schwannoma
Meningioma, CPA-IAC
Hemangioblastoma
Choroid Plexus Papilloma
Rare but Important
Anaplastic Astrocytoma
Atypical Teratoid-Rhabdoid Tumor
Choroid Plexus Carcinoma
Medulloblastoma Variants
Medulloepithelioma
Dysplastic Cerebellar Gangliocytoma
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Most common pediatric posterior fossa (PF) tumors
Medulloblastoma (PNET-MB)
Astrocytomas
Pilocytic astrocytoma (PA)
Infiltrating “glioma” (astrocytoma, WHO grade II)
Ependymoma
Imaging
Findings on conventional MR overlap
Location helpful in differential diagnosis
Tectum, cerebellum: PA
Pons: Diffusely infiltrating astrocytomas
Midline (vermis, fourth ventricle): PNET-MB, PA
Fourth ventricle + lateral recess/CPA mass: Ependymoma
DWI, MRS (normalized to water)
Can discriminate between pediatric PF tumors
PNET-MB, atypical teratoid-rhabdoid tumor (ATRT) show DWI restriction
Examine entire neuraxis in child with PF tumor prior to surgery!
T1 C+ essential (look for CSF spread)
History, PE (e.g., cutaneous markers) important
Helpful Clues for Common Diagnoses
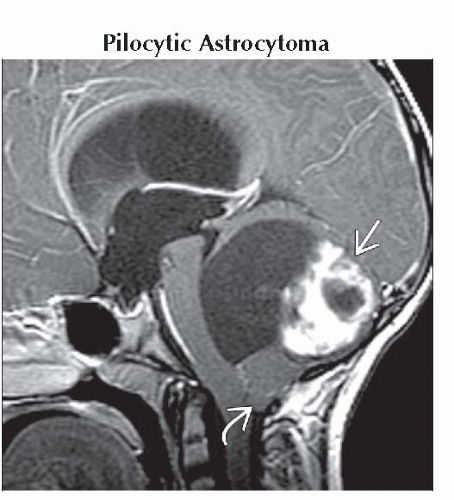
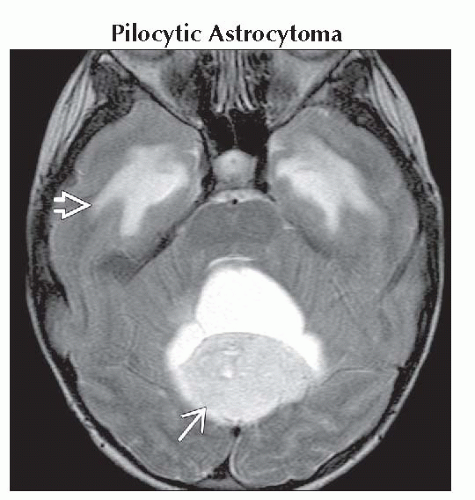
Pilocytic Astrocytoma
Child with cystic cerebellar mass + mural nodule
Solid component low density NECT, high signal T2
Medulloblastoma (PNET-MB)
Early childhood: Solid vermis mass extends into, fills, &/or obstructs 4th ventricle
Later onset: Lateral cerebellar mass
Hypercellular: ↑ Density on NECT, ↓ T2
DWI: Restricts
2-5% have nevoid basal cell carcinoma (Gorlin) syndrome (BCCS)
Typically seen with desmoplastic variant
Look for jaw cysts, bifid ribs, etc.
XRT can lead to induced basal cell carcinomas, other intracranial neoplasms within irradiated field
Ependymoma
Extrudes through 4th V outlet foramina into cisterns
Coarse calcifications
Diffusion restriction uncommon, may predict anaplastic behavior
Brainstem Glioma, Pediatric
Tectal plate glioma
NECT: Increased density progresses to Ca++
CECT/MR: Faint or no enhancement
Pontine glioma
Enlarged pons engulfs basilar artery
Enhances late in course, rarely at diagnosis
Dorsal exophytic glioma
Tumor protrudes into 4th ventricle
If large, may be difficult to differentiate from PA
Look for FLAIR signal change in dorsal brainstem or peduncles
Helpful Clues for Less Common Diagnoses
Ganglioglioma
Brainstem most common PF site
Look for expansion of nucleus cuneatus/gracilis
Schwannoma
Vestibular schwannoma (ICA/CPA) looks like “ice cream on cone”
T2 hyperintensity helps differentiate from meningioma
Multiple in NF2
Meningioma, CPA-IAC
Broad dural base, covers IAC
Variable signal, but T2 hypointensity common
Hyperostosis, tumoral calcifications
May have intra- or juxtatumoral cyst(s)
Hemangioblastoma
Late teen or adult
Intra-axial (cerebellum > medulla, cord)
Cyst + nodule > solid
Solid component shows flow voids, enhances avidly
Multiple lesions diagnostic of von Hippel-Lindau (VHL)
Avidly enhancing mural nodule abuts pia
Look for visceral markers of VHL in any child/young adult with hemangioblastoma
Choroid Plexus Papilloma
Frond-like 4th V or CPA tumor
Avidly enhancing
Hydrocephalus common
Helpful Clues for Rare Diagnoses
Anaplastic Astrocytoma
Infiltrating mass involves predominantly white matter
Enhancement none to sparse or patchy enhancement
Ring enhancement suggests progression to GBM
Atypical Teratoid-Rhabdoid Tumor
Imaging similar to PNET-MB plus
ATRT patients generally younger
Cysts, hemorrhages more common
CPA involvement more common
Frequent metastases at diagnosis
Both ATRT, PNET-MB show diffusion restriction
Choroid Plexus Carcinoma
Similar to CPP plus
Cysts, necrosis, bleeds
CSF/ependymal/parenchymal spread
Medulloblastoma Variants
Desmoplastic medulloblastoma (MB)
5-25% of all medulloblastomas
55-60% of PNET-MBs in children < 3 y
PNET-MB in older children, young adults often also desmoplastic variant
Desmoplastic subtype of MB in children < 2 is major diagnostic criterion for basal cell nevus syndrome (Gorlin syndrome)
Nodular collections of neurocytic cells bounded by desmoplastic zones
Lateral (cerebellar) location
MB with extensive nodularity (MBEN)
Formerly called “cerebellar neuroblastoma”
Usually occurs in infants
Gyriform or “grape-like” appearance
May mature → better prognosis
Medulloepithelioma
Rare embryonal brain &/or ocular tumor
Inhomogeneous signal, enhancement
Dysplastic Cerebellar Gangliocytoma
Diffuse or focal hemispheric mass
Thick cerebellar folia with “striated” appearance
Evaluate for Cowden syndrome
Image Gallery
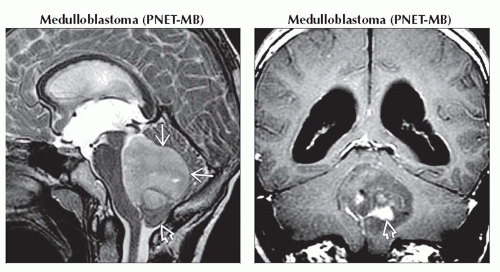 (Left) Sagittal T2WI MR shows a hyperintense mass
 filling and expanding the 4th ventricle. The tumor does not extend through the 4th ventricular outlet foramina. There is hydrocephalus with acquired tonsillar herniation filling and expanding the 4th ventricle. The tumor does not extend through the 4th ventricular outlet foramina. There is hydrocephalus with acquired tonsillar herniation  . (Right) Coronal T1 C+ MR shows heterogeneous enhancement . (Right) Coronal T1 C+ MR shows heterogeneous enhancement  of the 4th ventricular PNET-MB. of the 4th ventricular PNET-MB.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|