Figure 81.1. Condensation in left lung base with pleural spill after cerebral tumor resection (Author’s personal archive).
Atelectasis. Central respiratory depression, injury of the cervical and thoracic spinal cord, hypoventilation because of pain, altered consciousness, bronchial blockage due to mucus plugs, and traumatic pulmonary compression due to pneumothorax, haemothorax and pleural effusion contribute to the formation of atelectasis. It is the main cause of immediate postoperative low fever (24 to 48 hours after surgery). Large areas of atelectasis are responsible for a scenario of serious hypoxemia. Treatment includes manoeuvres of alveolar recruitment (positive end-expiratory pressure [PEEP], increase of the inspiratory time) and physiotherapy. Inadequate resolution and respiratory insufficiency are indications for fibrobronchoscopy.
Respiratory insufficiency. Respiratory insufficiency is a life-threatening complication after neurosurgery. The neurological causes are the pathologies that determine altered level of consciousness or reduced ventilation. The level of consciousness is related to the loss of the ability to keep the airway open and compromises normal breathing. Reduced ventilation can result from a partial or complete loss of the diaphragm’s innervation (injuries of the upper cervical spinal cord) which reduces lung capacity. The pulmonary causes are atelectasis, pneumonia, gastric aspiration, pulmonary thromboembolism, bronchospasm, neurogenic pulmonary edema, and the adult respiratory dysfunction syndrome (ARDS).
In the immediate postoperative period, hypoventilation can occur due to the accumulation of anaesthetics in body fat, leading to renewed sedation. This occurs with halothane and opioids.
Cardiovascular System
Monitoring of mean arterial blood pressure is essential, since hypotension is the leading cause of secondary neuronal injury, and hypertension can lead to bleeding and increase cerebral edema and intracranial hypertension. Automatic non-invasive monitoring of arterial pressure is recommended in patients with hemodynamic stability. This technique has significant limitations in patients who present sudden fluctuations in arterial pressure. It is not indicated for patients in which accurate measuring of arterial pressure is important. The invasive arterial pressure monitoring detects sudden pressure changes and extreme blood pressure levels and facilitates the repeated collection of tests and arterial blood gas analysis. The average arterial pressure must be the value used for decisions in seriously ill patients. In the direct measure of arterial pressure an invasive line is necessary; however, the risk of complications is low. Placement of an invasive arterial pressure (usually in a radial artery) is recommended in the first 24 hours after neurosurgery.
In the immediate postoperative period the average arterial pressure must be kept between values considered normal (80-100 mmHg), while taking into consideration the age group, the nature and extent of the injury, and the previous blood pressure levels of the patient. Invasive monitoring of arterial pressure will continue after 24 hours postoperative in cases which hemodynamic instability is not reached.
The American Heart Association considers continued monitoring with ECG an intervention class I for all patients in intensive care. The incidence of arrhythmias after major surgery is high.
The urinary debit is usually voluminous with the use of mannitol, and blood volume replacement with crystalloids must be intensified to prevent depletion of the extracellular space.
Cardiovascular Complications
Arterial hypertension. Arterial hypertension is frequent in the immediate postoperative period and has been reported in 70-90% of patients. It is due to sympathomimetic stimulation caused by the increase of circulating catecholamines and oxygen consumption. Administration of sodium nitroprusside can be a powerful and safe way to treat serious hypertension. This drug is a cerebral vasodilator but causes a minimum rise of intracranial pressure. Esmolol, a fast-acting beta-blocker, can be used in a similar way, without the risk of increasing intracranial pressure. In patients with chronic hypertension, it seems appropriate to start previous oral anti-hypertensive medication at about half to the two thirds of the previous dose as soon as possible. Frequent rest and sedation reduce the hypertensive condition of a more delayed postoperative patient.
Cardiac complications. Cardiac arrhythmias appear in up to 28% of cases and most often they are supraventricular. Cardiac complications in any patient submitted to surgery may be anticipated thorough preoperative evaluation. The incidence in patients without previous cardiac disease is very low (<0.2%) and the detection of risk factors is of extreme importance. Studies identify risk factors of heart complications in patients not submitted to heart surgery. Evidence of heart attack of the myocardium in last the 6 months, diagnosis of unstable angina, presence of congestive cardiac insufficiency, chest X-ray with signs of pulmonary congestion, valve disease (mainly aortic stenosis), age >70 years, emergency surgery, arrhythmias, and generally unfavourable conditions are the main data to be collected and identified in neurosurgery patients in the preoperative period.
In patients who experience a heart attack of the myocardium in the last 3 to 6 months, the rate of having one again is 30%, whereas in those who suffered a heart attack more than 6 months earlier this rate falls to 5%. Reinfarction occurs in the first 72 hours after surgery, but it can appear until the sixth day after surgery. More than half of these heart attacks are quiet, in which case ECG and serial enzyme dosage are indicated until the sixth postoperative day in patients at high risk. ECG abnormalities are found in 40-60% of patients with subarachnoid hemorrhage due to aneurysm rupture. The most frequent are S-T segment alterations or arrhythmias. A heart attack secondary to subarachnoid hemorrhage has been reported, but it is extremely rare. These ECG alterations can come from injury to the hypothalamus and high levels of catecholamine.
Patients must have their medications optimized during the preoperative period, once 60% decompensated in the first postoperative hours. Left acute cardiac insufficiency can occur after subarachnoid hemorrhage due to aneurysm rupture, mainly in patients with the worst clinical severity.
In patients with heart valve disease, prophylaxis for bacterial endocarditis may be recommended. In those with valve prostheses and under anticoagulation, the therapy should be suspended during the preoperative period. The risk associated with discontinuation of anticoagulant therapy depends on the type of valve, the localization and factors of associated risks. In patients with only one aortic valve prosthesis and without associated risk factors, the anticoagulant is suspended 3 days before surgery. When the thromboembolism risk is high, intravenous heparin is initiated before surgery with INR <2 and suspended 8 hours before surgery. The TTPA has to be normal 6 hours after heparin suspension. Patients at higher risk of thromboembolism are those with mitral valve prosthesis, atrial fibrillation, previous thromboembolism, ventricular dysfunction, mechanical tricuspid valve or with more than one mechanical valve. A period of 5 to 7 days after-craniotomy is probably a safe break to restart anticoagulation.
Body Temperature
During the immediate postoperative period, hypothermia must be avoided since it causes tremors which increase oxygen consumption, cardiac debit and/or blood pressure. All these alterations favour brain hyperaemia which can contribute to delirium in older patients, difficult to control arterial hypertension and intracranial hypertension. The best way to limit the development of tremors in the postoperative period is to maintain normothermia.
Fever. Fever is very frequent in serious neurosurgery patients due the high risk of nosocomial infections. The role of hypothermia in neuroprotection remains uncertain, but there is consensus that hyperthermia negatively impacts on neurological recovery. Currently it is known that a gradient exists between central body temperature (oesophageal, rectal) and brain temperature. The brain temperature is underestimated, which increases the risk of secondary neuronal injury. An aggressive antithermic treatment for fever and general cooling measures are indicated.
Glucose Metabolism
Metabolic monitoring mainly involves blood glucose control. Glucose measurement every 4 hours is recommended to prevent a neurological catastrophe during the postoperative period. Prospective and randomized studies in critically ill patients have demonstrated that the evolution is better in the surgical group that receives insulin therapy and remains euglycaemic (80-110 mg/dl) than in those with glucose levels between 180 and 200 mg/dl. Hyperglycaemia (>200 mg/dl) worsens the neurological evolution. Hypoglycaemia can lead to irreversible neuronal injury and must be prevented to the maximum. In the postoperative period the objective is to keep the patient euglycaemic (≤140 mg/dl) without a significant increase in the risk of hypoglycaemia episodes.
Electrolyte Control
Much attention must be directed to prevent electrolyte disturbances in the postoperative period. Disturbances occur through alterations between extracellular volume and sodium concentration.
Hyponatremia. Hyponatremia is frequent in seriously ill neurological patients. The measure of serum sodium does not allow to distinguish between hyponatremia associated with hypervolaemia or hypovolaemia. Hyponatremia associated with hypo-osmolality contributes to the increase in intracellular volume which causes or aggravates cerebral edema and intracranial hypertension and with hyperosmolality can lead to cerebral infarction. The main causes of hyponatremia/hypovolaemia in the postoperative period are: diuretic, mannitol, vomiting, diarrhoea and mineralocorticoid deficiency. In these situations, arterial pressure, urinary debit and urinary osmolality can be low, but urea and creatinine will be raised. Replacement with isotonic solutions (physiological saline 0.9%) allows the correction of these electrolyte imbalances. Another important cause of hyponatremia is the cerebral salt loss syndrome, which causes the release of natriuretic factors leading to increased diuresis, natriuresis and hypovolemia with normal or raised urinary osmolality. Hyponatremia is corrected by the replacement of solutions with higher sodium concentration (physiological saline 3%). In the presence of hyponatremia in the postoperative period, the syndrome of inappropriate antidiuretic hormone secretion (SIADH) is always part of the differential diagnosis, since it demands management in the opposing direction from other aetiologies. This syndrome is caused by the inappropriate secretion of the antidiuretic hormone and is associated with water retention and hypervolemia with high urinary osmolality. The treatment of the SIADH consists of water restriction of 500 ml/day if sodium is <120 mEq/l and 1000 ml/day if sodium is 120-130 mEq/l. If sodium is <115 mEq/l, convulsions or a coma state caused by hyponatremia or in the presence of pathologies in which water restriction is contraindicated (period of vasospasm), a 3% saline solution can be administered.
81.2.2 Prophylaxis of Clinical Complications in the Postoperative Period
Beyond routine monitoring, care postoperative includes the prophylaxis of infection, deep venous thrombosis and upper digestive hemorrhage.
Prophylaxis of Infections
The utility of antibiotic prophylaxis has been widely discussed over the last decades. Controlled studies have finally demonstrated the effectiveness of appropriate antibiotic therapy. Prophylactic antibiotic therapy reduces the incidence of surgical site infections and meningitis during the postoperative period. Anti-staphylococcal agents are studied and recommended. In craniotomies (clean surgeries) the use of cefazolin is recommended in one dose 30 minutes before scalp incision or in special cases of 24-hour antibiotic treatment (ventriculoperitoneal shunt placement).
Prophylaxis of Deep Venous Thrombosis and Pulmonary Thromboembolism
Deep venous thrombosis (DVT) of the lower extremities occurs in 29-43% of neurosurgical patients and the incidence of pulmonary thromboembolism (PTE) is 15%. The risk factors are immobilization for prolonged periods, paralysis of the lower extremities, prolonged surgery (+4 hours), advanced age, neoplasia, direct injury lower limb veins, previous PTE, cerebrovascular disease, use of oral contraceptives, obesity, cardiac congestive insufficiency, hypercoagulability, and pregnancy. Due to the high morbidity and mortality of DVT/PTE, prophylaxis is essential. Some studies confirm the utility of pneumatic compression of the lower limbs before surgery until the patient can walk again. Early mobilization can prevent the formation of venous thrombi. Beyond mechanical support, the use of low-dose heparin or low-molecular-weight heparin is recommended. Low-molecular-weight heparin (enoxaparin 40 mg 1x/d SC, nadroparin 7500 U 1x/d SC) or non-fractionated heparin (heparin 5000 U SC 8/8 hours) initiated 24 hours after the procedure are more efficient in PTE prevention than compression therapy. There is a non-statistically and significant risk of bleeding with this therapy. The American College of Chest Physician places neurosurgery patients in the category of high risk for PTE in the perioperative period. The association of mechanical and pharmacological prophylactic treatments in these patients is indicated.
Prophylaxis of Upper Gastrointestinal Hemorrhage
Neurological patients are at an increased risk of gastrointestinal bleeding or gastric perforation. In an endoscopic evaluation of neurointensive patients, erosions of the gastrointestinal mucosa were seen mainly in patients with secondary intracranial hypertension to brain tumours, TBI or intracranial surgery. In a cohort study of neurosurgical patients in the ICU (excluding TBI) it was observed that 6.8% had gastrointestinal complications in the postoperative period. The majority presented bleeding but a small number evolved with bleeding and perforation. The main risk factors were: SIADH, coma before surgery, postoperative complications, age >60 years, and CNS infections. Corticoids, extensively used in the neurosurgery population, contribute to the formation of gastrointestinal ulcerations. The risk of developing ulcers is twice higher and intestinal perforation can occur in corticosteroid users. In these patients medical prophylaxis of stress ulcers is indicated. Sulcrafate provides efficient prophylaxis without excessively increasing gastric pH (less risk of ventilator-associated pneumonia). However, the difficulty to manage sulcrafate and the reduction in the absorption of anticonvulsants and other drugs delivered by nasogastric catheter make H2 blockers and proton-pump inhibitors the best alternatives for a short postoperative period. Probably, there is no need for pharmacological prophylaxis in patients on an oral diet. In pharmacological prophylaxis ranitine must be used in patients <65 years of age at a dose of 50 mg IV from 8/8 hours or 150 mg OD from 12/12 hours and in those >65 years a dose of 50 mg IV for 12/12h. Omeprazole at a dose of 20-40 mg/d IV or OD.
81.2.3 Monitoring and Diagnosis of Neurological Complications
The neuro-check is a quick neurological evaluation but it does not substitute complete neurological examination. It includes serial recording of the Glasgow Coma Scale (GCS), pupillary size, symmetry and photoreactivity, type of breathing and presence of focal neurological deficits. Any variation in this neurological evaluation must be interpreted as a signal of worsening of the patient and be followed by complete neurological examination and diagnostic and therapeutic measures. The frequency of neuro-check (Table 81.1) changes according to the pathology and clinical evolution of the patient. In the postoperative period, monitoring of the GCS and pupils every 15 minutes until extubation identifies neurological complications in a prompt and effective way. Over the next 6 hours after extubation, a complete neuro-check can be performed every 30 minutes and then every hour up to 24 to 48 hours after surgery. The indications for motoring of intracranial pressure after craniotomy are very varied and controversial.
Postoperative patient | Glasgow Coma Scale | Pupils | Breathing | Focal deficit |
Intubated | Every 15 minutes | Every 15 minutes | – | – |
Extubated (first 6 hours) | Every 30 minutes | Every 30 minutes | Every 30 minutes | Every 30 minutes |
Extubated (after 6 hours) | Every hour | Every hour | Every hour | Every hour |
Table 81.1. Frequency of neuro-check in the postoperative period.
Intracranial Hypertension
Elevated intracranial hypertension (ICH) causes injury to the brain by compression, herniation and ischemia. It is generally accepted that monitoring and aggressive treatment of ICH can reduce secondary ischemia and improve the neurological evolution. Intracranial hypertension is common after neurosurgery. A retrospective study monitored 514 patients after elective intracranial surgery and verified the presence of ICH in 18.4% of supratentorial surgeries and 12.7% of infratentorial interventions. Of these patients with ICH, clinical deterioration occurred in only 52.8%. The neurological examination does not always allow early diagnosis of hypertension. Hypertension is characterized by chronic headache, nausea, vomiting, reduced level of consciousness and neurological compromise. Some measures to control and prevent hypertension include: headboard elevated to 30 degrees; prevention and treatment of arterial hypertension; treatment for pain, nausea and vomiting; prevention and treatment of tremors; and maintenance of adjusted ventilation and oxygenation. The most common causes of hypertension in the postoperative period are: edema; hemorrhages; cerebral hydrocephalus; pneumoencephalus; and cerebral infarction.
Cerebral Edema
Apart from localization and type of neoplasia, the main focus in the immediate postoperative period is cerebral edema. The development of edema in the immediate postoperative period is associated with manipulation of deep structures and the removal of cerebral tumours. In response to direct trauma from surgical intervention and tissue retraction, there occur relative tissue ischemia, reduction in venous return and reduction in cerebral complacency. Cerebral edema can develop with increased intracranial pressure. The use of the electrocautery increases the local injury and is directly associated with cerebral tissue trauma.
Edema appears 4 to 5 hours after surgery and peaks within 48-72 hours (Figure 81.2).
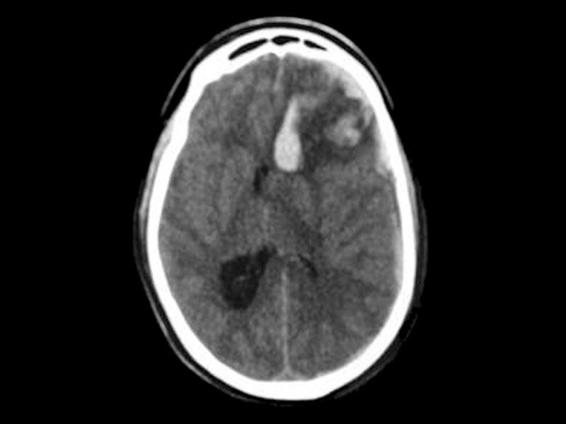
Figure 81.2. Cerebral edema in the left frontal region with minor bleeding. Immediate postoperative period after tumor resection (Author’s personal archive).
Clinical manifestations correspond to the cerebral area injured. Motor or sensory alterations of the mental state, deficits and paralyses of cranial nerves are common. Transtentorial herniation can occur, worsening the prognosis. Brain CT confirms the diagnosis and excludes such other complications as hydrocephalus and hemorrhage. The tomographic findings are: deletion of ridges; reduction of the size of the ipsilateral ventricle; midline deviation; hypodensity and deletion of the interface between the white and gray matter. After diagnosis with CT, treatment must be initiated. The main objective is to maintain cerebral perfusion pressure (CPP) >60 mmHg and ICP <20 mmHg. The headboard of the bed must remain high (30 degrees) to aid cerebral venous return. Adequate cerebral perfusion pressure is kept by the infusion volume and use of vasoactive drugs. PaCO2 must be kept around 35 mmHg. Hyperventilation (PaCO2 25-30 mmHg) is indicated when clinical signals of herniation are present. In patients with ICH on mechanical ventilation, sedation is mandatory (benzodiazepines, opioids, propofol). Corticoid administration (dexamethasone in 4 doses every 6 hours up to a dose of 10-40 mg) is recommended for patients submitted to brain tumour resection. The clinical response of cerebral edema to dexamethasone for primary malignant cerebral tumours is less dramatic than for metastasis, and meningomas less than gliomas. In patients with external ventricular derivation (EVD), cerebrospinal fluid drainage can assist in the control of ICP. The administration of mannitol at a dose of 0,25 to 1 g/kg must be quickly initiated and monitored with serum osmolarity (serum osmolarity kept <320 mOsm). The alternative to this osmotic therapy is hypertonic saline solution in bolus (physiological saline 3 20%), being mainly indicated in patients refractory to mannitol or in the presence of renal function loss. Decompressive craniectomy is indicated in patients with a persistent rise in ICP, despite optimized medical treatment. In the presence of unilateral cerebral edema following cerebral tumour resection, the removal of a great bone flap with dural plastic has had success in reducing ICP.
Hemorrages
The occurrence of hemorrhage in the immediate postoperative period and the development of epidural, subdural or intraparenchymal haematoma is always a feared complication, because it is a significant and potentially avoidable situation. Accurate estimation of the incidence of haematomas became possible with the advent of tomography in clinical practice. Currently, the incidence of extradural haematoma after neurosurgery varies between 0.9 and 7.1%, whereas the incidence of intracerebral haematoma is of 3.9%. Surgery for ventriculoperitoneal derivation is associated with a very small percentage of bleeding in the surgical site.
The diverse causes associated with this fearful complication are related to the surgical technique and clinical morbidities. Inadequate perioperative haemostasis, inadequate tissue suture, important tissue retraction, abrupt ventricular decompression, direct injury of the cerebral vessels, arterial hypertension and thrombocytopenia. Cerebral tumour resection (resection of malignant tumours) and craniotomy for haematoma draining are associated with a higher incidence of hemorrhage.
Clinical manifestations include chronic headache, new neurological deficit, convulsive seizures, reduced level of consciousness, signs of transtentorial herniation with hypertension, bradycardia and respiratory insufficiency. In patients with bleeding in the posterior fossa, the manifestations are related to the degree of compression of the brainstem and are predominantly related to cardiovascular and respiratory decompensation.
The diagnosis is based on head CT (Figure 81.3) and the treatment is emergency surgery for draining the haematoma and relief of intracranial hypertension.
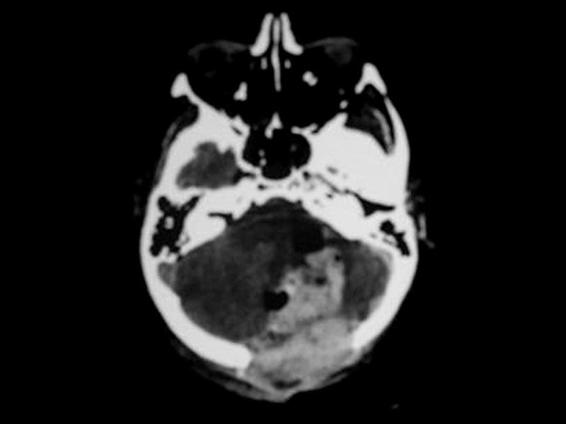
Figure 81.3. 68-year-old woman submitted to posterior tumor resection of the fossa. Deterioration of consciousness (GCS from 15 to 4) during the immediate postoperative period. Emergency CT showing major hemorrhage in the operative stream bed (Author’s personal archive).
Hydrocephalus
Surgery of the posterior fossa and intraventricular space are often associated with hydrocephalus in the postoperative period. Hydrocephalus can occur in patients with subarachnoid hemorrhage and intracerebral hemorrhage with or without intraventricular extension.
The initial manifestation can be chronic headache or paralysis of cranial nerves, especially cranial nerves III, IV and VI, but also it can present with rapid neurological deterioration.
Ventriculostomy, lumbar puncture and third ventriculostomy endoscopy are all viable methods for handling an acute hydrocephalus.
Ventriculostomy is the most commonly used technique: it can be a heroic measure; it can help to stabilize the patient and gains time for a definitive treatment or time for the base condition to resolve itself and CSF flow to return to normal.
Pneumoencephalus
Pneumoencephalus consists of intracranial air in the following compartments: epidural, subdural, subarachnoid and intraventricular. It is one of the causes of deterioration of consciousness after surgery of the posterior fossa and supratentorial procedures. The risk is higher when the patient is operated in a seated position. Air in the epidural space occurs after surgery involving the skull base where an extensive bifrontal craniotomy is made. Measures in the intraoperative period to prevention the development of pneumoencephalus include closing of the dura mater, reconstruction of the skull base, re-expansion of the intracranial contents and placing a drain in the epidural space. The clinical signals of hypertensive pneumoencephalus generally occur within 2 to 4 days after the operation. Accumulated air causes mass effect and has important clinical repercussion (Figure 81.4).
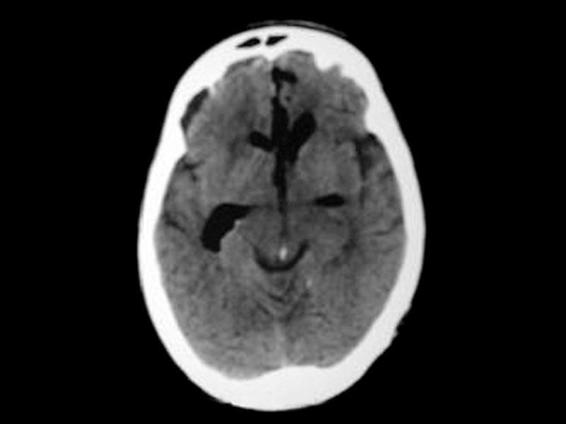
Figure 81.4. Patient submitted to cerebral tumor resection, with intense chronic headache in the immediate postoperative period but without focal deficit. Emergency CT showing major pneumoencephalus (Author’s personal archive).
The more common clinical manifestations are chronic headache (38%), nausea, vomiting and deterioration of the level of consciousness, with mental confusion or lethargy. It can evolve to coma without focal neurological signals. Hyponatremia is common and convulsive seizures can worsen the situation. Air is evident on the head CT up to 7 days after surgery. Simple pneumoencephalus does not require treatment. In the attempt to promote the reabsorption of pneumoencephalus, some authors suggest keeping the patient with the headboard flat for 48 to 72 hours and with 100% of oxygen. It is thought that ventilation with 100% allows a nitrogen exchange for oxygen of the intracranial air, which is quickly absorbed by the bloodstream. Hypertensive pneumoencephalus must be evacuated (aspiration or catheter placement) with urgency like intracranial haematoma. Surgery can be necessary to repair a skull base fracture or CSF fistula.
Cerebral Vasospasm
The main focus in the immediate postoperative period after clipping of cerebral aneurysm for subarachnoid hemorrhage is the prevention of vasospasm. Up to 70% of hemorrhage cases present vasospasm diagnosed through some complementary examination such as transcranial Doppler (Figure 81.5) or cerebral arteriography (Figure 81.6).
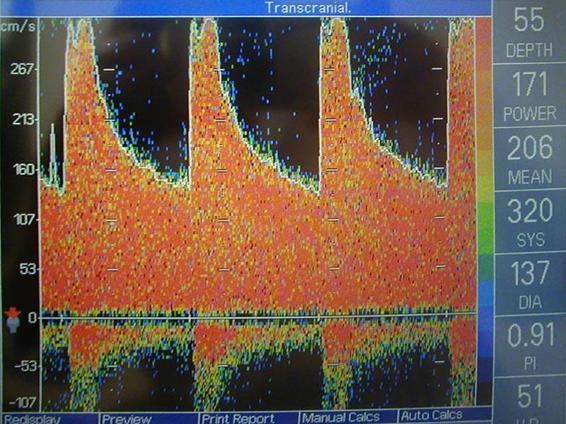
Figure 81.5. Transcranial Doppler showing severe vasospasm (average speed >200 cm/s) in the right middle cerebral artery.

Figure 81.6. HSA Hunt-Hess III. Arteriography showing vasospasm of the basal artery. (Author’s personal archive).
However, clinical vasospasm (cerebral ischemic deficit or cerebral infarction) occurs in up to 35% of patients with hemorrhage and is the leading cause of morbidity and mortality in survivors. The main risk factors of vasospasm are: higher clinical severity, greater blood volume on the CT scan, hypotension, hypovolaemia, hyponatremia, hyperthermia and hyperglycaemia. The use of nimodipine to prevent vasospasm has been vastly studied. A meta-analysis of 8 studies, evaluating 1574 patients with subarachnoid hemorrhage (Hunt-Hess I to III) evidenced that the use of the nimodipine improves the immediate prognosis, and in 3 months in 27% of cases, reduces the neurological ischemic deficit in 33%, reduces incidence of cerebral infarction on CT in 21%, and reduces the incidence of vasospasm on arteriography in 20%. The recommendation is administration of oral nimodipine at a dose of 60 mg every 4 hours (IV with greater hypotension) for 21 days. From a hemodynamic point of view, it is clear that hypotension and hypovolaemia worsen the prognosis and must be prevented in all patients after subarachnoid hemorrhage. However, there are no data supporting the prophylactic use of HHH therapy (hypertension, hypervolaemia, haemodilution) in patients with subarachnoid hemorrhage without clinical evidence of vasospasm.
Convulsions
The incidence of early convulsions (first 7days after surgery) varies between 4 and 19% of cases. When late convulsions are considered, the incidence increases up to 70%. They can be focal or generalized. The situations considered at risk for seizure occurrence include:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






