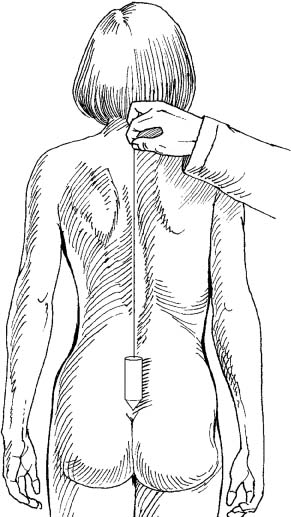
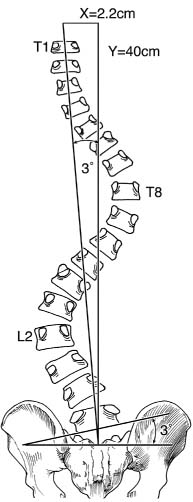
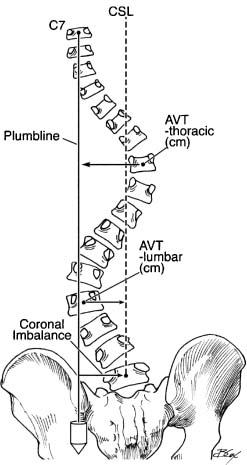
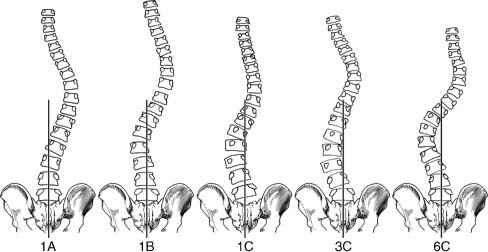
Chapter 8 Correction and preservation of truncal balance is a critical component in the surgical treatment of spinal deformities. Since the recognition of iatrogenic flat-back syndrome, recent discussions have largely been directed at imbalance in the sagittal plane. This chapter will focus on the surgical correction of imbalance in the coronal plane. Spinal decompensation or imbalance is caused by the inability or loss of ability of the normal portion of the spine to compensate for a structurally abnormal primary deformity. The primary deformity can be of any origin—idiopathic, congenital, neuromuscular, post-traumatic, and so forth. In cases where the primary deformity is not severe and the normal portions of the spine (above and/or below the primary deformity) are able to form a compensatory curve, the spinal axis remains balanced with the head centered over the sacrum. In cases where the primary deformity is so severe that the remainder of the spine is unable to fully compensate, an imbalance occurs. An imbalance will also result in cases where, due to age-related changes, the normal portion of the spine becomes structurally abnormal or loses its ability to keep pace with the progressive primary deformity. Patients with coronal plane deformities often have associated sagittal and axial plane deformities. Although this chapter brings attention to the surgical restoration of coronal balance, we stress that the coronal plane deformity should not be evaluated or treated in isolation but in the context of the accompanying sagittal and axial plane deformities. The majority of spinal deformity literature highlights the amount of correction of Cobb angle magnitudes. Although correction of the primary deformity is important, the amount of correction obtained should be secondary to the achievement of coronal and sagittal balance. Balanced nonprogressive deformities in the coronal plane are usually well tolerated by patients. It is when the spine becomes unbalanced that symptoms arise. Coronal imbalance is of primary concern in five categories of spinal deformity: adolescent idiopathic scoliosis with major thoracic-compensatory lumbar curves, adult idiopathic scoliosis, degenerative scoliosis, congenital scoliosis, and complex rigid multiplanar deformities. The surgical restoration of coronal balance for each of these categories will be discussed. The evaluation of a patient with a spinal deformity begins with a detailed history. The onset of the deformity and prior treatments are necessary details to elicit. It is important to determine whether pain is associated with the deformity and whether the pain is axial or related to neural compression. Axial pain in spinal deformity can be related to muscle fatigue, degenerative disk disease, or facet arthrosis. The patient with symptomatic spinal imbalance (coronal or sagittal) will usually experience fatigue-related axial pain. Dissatisfaction with appearance is a common complaint. Patients with coronal imbalance may also experience a sensation of unequal leg lengths (even though measured leg lengths are equal) and an uneven pelvis during sitting and standing. Many patients with mild coronal imbalance can be asymptomatic, however. The amount of coronal imbalance that is tolerated prior to onset of symptoms is not well defined. Coronal imbalance can be readily recognized with careful physical examination. The patient is asked to stand straight and is viewed from four directions. From the front and back views, the shifting of the trunk and relative heights of iliac crests and shoulders are noted. A plumb line is dropped from the palpable spinous process of C7 (or T1). The deviation of the plumb line from the gluteal cleft denotes the amount of clinical imbalance (Fig. 8–1). From the side views, signs of sagittal imbalance such as loss of lumbar lordosis or hip/knee flexion are noted. The patient is then asked to forward bend and is viewed again from four directions to look for thoracic hump and lumbar asymmetry. Lateral bending in the standing position can give the surgeon a sense of how flexible the curves are and whether pain or radicular symptoms are reproduced. The remainder of the clinical evaluation is completed with a thorough neurologic examination. Figure 8–1 A plumb line is dropped from the palpable spinous process of C7 (or T1). The deviation of the plumb line from the gluteal cleft, measured in centimeters, denotes the amount of clinical imbalance. (From Albert TJ, Vaccaro AR. Physical Examination of the Spine. New York: Thieme, 2005, with permission.) To assess spinal deformity, standing posterior-anterior and lateral views of the entire spine are viewed on long 36-in. cassettes. Cobb angle magnitudes of all curves are measured. Pelvic obliquity in the standing or sitting positions is determined. To evaluate shoulder balance, the horizontal tilt of T1 and the clavicle angle should be measured. The clavicle angle is formed by the intersection of the horizontal line and the tangential line connecting the highest two points of each clavicle. This angle has been shown to correlate best with shoulder balance.1 If present, the lumbosacral fractional curve is important to evaluate. A lumbosacral fractional curve creates an uneven foundation for the entire spine. If not compensated by another fractional curve, a curve of only a few degrees can lead to coronal imbalance. For example, in a patient with an uncompensated lumbosacral fractional curve of 3 degrees and an average spinal column length of 40 cm, a coronal decompensation of 2.2 degrees would result (Fig. 8–2). Figure 8–2 A lumbosacral fractional curve creates an uneven foundation for the entire spine. For example, in a patient with an uncompen-sated lumbosacral fractional curve of 3 degrees and an average spinal column length of 40 cm, a coronal decompensation of 2.2 cm would result. To determine if a coronal plane deformity is balanced, a vertical plumb line is drawn from the spinous process or midbody of C7 (or T1) toward the floor. In a coronally balanced spine, this line should pass within 1 cm of the center of the sacrum or the spinous process of S1. The amount of lateral deviation of this line away from the middle of the sacrum (measured in centimeters, toward the left or the right) denotes the radiographic coronal imbalance (Fig. 8–3). Alternatively, some authors report coronal imbalance as trunk shift. To measure trunk shift, the center sacral line (CSL) is constructed as a vertical line extended cephalad from the spinous process of S1. A second vertical plumb line is constructed from the midbody of C7 or T1 toward the floor. The horizontal distance between these two lines denotes the trunk shift. Bending views to assess the flexibility of the primary and compensatory curves are mandatory for preoperative planning. Some surgeons prefer supine left and right bending views, whereas others prefer push-prone techniques.2 The push-prone film is obtained by placing the patient prone on a 36-in. cassette. A firm medial translational force is applied to the portion of the torso that corresponds with the apex of the primary curve. Counterforces are then applied to the opposite side of the body in the axilla and pelvis by an assistant to create a three-point corrective force. Figure 8–3 To determine if a coronal plane deformity is balanced, a vertical plumb line is drawn from the spinous process or midbody of C7 (or T1) toward the floor. The amount of lateral deviation of this line away from the middle of the sacrum (measured in centimeters, toward the left or the right) denotes the radiographic coronal imbalance. The central sacral line (CSL) is constructed as a vertical line extended cephalad from the spinous process of S1. The apical vertebral translation (AVT) is the distance of the apical vertebra of the thoracic curve from the plumb line and lumbar curve from the CSL. Also to assist with preoperative planning, the neutral, stable, and apical vertebrae are identified on the standing and bending films. The stable vertebrae is the segment most closely bisected by the CSL. The neutral vertebrae are the nonrotated vertebrae at the caudal extent of the curvature. It is usually the segment just proximal to the stable vertebrae. The apical vertebrae have the greatest translation from the midline for each curve. The magnitude of translation and rotation of each apical vertebra are noted. As each of the clinical categories of coronal imbalance are discussed, the role of these radiographic findings in the surgical decision-making process will be described. In a subset of adolescent idiopathic scoliosis patients with thoracic and lumbar double curves, the thoracic curve is the primary deformity whereas the lumbar curve is merely compensatory. For this type of curve (previously classified as King-Moe II, now known as Lenke 1B and Lenke 1C; Fig. 8–4), King and Moe found that arthrodesis of only the thoracic curve with Harrington distraction instrumentation resulted in excellent outcome.3 Postoperatively, the nonfused compensatory lumbar curve spontaneously corrected itself to balance the remaining fused thoracic curve. This accomplished the primary goal of a balanced spine with the fusion mass centered over the pelvis while minimizing the number of lumbar levels needed to be fused. King and Moe remarked that the caudal extent of fusion should include the stable and rotationally neutral vertebrae to ensure the achievement of a balanced stable spine.3,4 Figure 8–4 To avoid postoperative coronal imbalance in thoracic and lumbar double curves, it is first critical to correctly identify the curve patterns suitable for selective thoracic fusion. A thoracic and lumbar double-curve pattern may be classified as either Lenke Type 1, 3, or 6 curves. In the late 1980s, modern segmental instrumentation was introduced. This brought an initial wave of excitement because of the ability of the newer instrumentation systems to exert powerful derotational and translational corrective forces. However, when King and Moe’s principles of selective thoracic fusion were applied to these curves using modern segmental instrumentation, postoperative coronal decompensation resulted in as many as 20% of patients.5 Since the emergence of this problem, several factors have been cited as causative, including incorrect identification of curve patterns, lumbar curve magnitude or stiffness, relative position and rotation of the apical vertebrae, use of “derotational” maneuvers, overcorrection of the thoracic curve, and choice of fusion levels. Various authors have made conflicting recommendations regarding the proper management of these curve patterns. To avoid postoperative coronal imbalance in thoracic and lumbar double curves, it is first critical to correctly identify the curve patterns suitable for selective thoracic fusion. A thoracic and lumbar double-curve pattern may be classified as either Lenke Types 1, 3, or 6 (Fig. 8–4). Lenke Type 6 curves are thoracic and lumbar double curves where the lumbar curve is the major curve (i.e., having the largest Cobb angle measurement). Lenke Type 6 curves should not be considered for selective thoracic fusion. In Lenke Type 1 and Type 3 curves, the thoracic curve is the major curve. Lenke Type 1A curves (formerly classified as King-Moe III) are thoracic-only curves where the lumbar vertebrae do not cross the midline and the CSVL falls between the lumbar pedicles up to the stable vertebrae. Lenke Type 1A curves are readily recognized and can undergo selective thoracic fusion with no problems of postoperative coronal imbalance. Lenke Types 3A and 3B are extremely uncommon and will not be considered here.6 Therefore, in all practicality, when faced with a major thoracic and minor lumbar double curve, we are left to consider categorizing the curve as either Lenke Type 1B, 1C, or 3C. Lenke Types 1B and 1C are the so-called false double-major curves where the thoracic curve is structural and the lumbar curve is only compensatory. Lenke Type 3C curves, on the other hand, are the so-called true double-major curves where both the thoracic and lumbar curves are structural. To distinguish between Lenke Types 1B/1C and Lenke Type 3, side-bending films are required. If the lumbar curve has a persistent Cobb angle of >25 degrees on side-bending films and/or if there is >20 degrees of kyphosis from T10 to L2, the lumbar curve is considered structural. The presence of a structural lumbar curve distinguishes a Lenke 3C from a Lenke 1B/1C. Lenke Types 1B/1C are amenable to selective thoracic fusion, and fusion of both the thoracic and lumbar curves should be strongly considered in Lenke Type 3C. Lenke Types 1B and 1C can be distinguished from each other by the lumbar modifier. In lumbar modifier B, the CSVL falls between the concave pedicle and the lateral margin of the lumbar apical vertebral body, whereas in lumbar modifier C, the CSVL falls medial to the lateral margin of the lumbar apical vertebral body. Both Lenke Types 1B and 1C are amenable to successfully balanced selective thoracic fusion. After identification of the curve type as Lenke 1B or 1C, the specific characteristics of the curves should be determined to assess the risk of postoperative coronal decompensation after selective thoracic fusion. On the coronal standing radiograph, the magnitudes of the thoracic and lumbar curves, the rotation of the thoracic and lumbar curves using Nash-Moe criteria, and the translational distance of the apices of the curves from the plumbline (thoracic curve) and the CSVL (lumbar curve) can be measured. If the ratio of the thoracic to lumbar curve magnitude is >1.2, the ratio of the thoracic to lumbar apical vertebral rotation is >1.0, and the ratio of the thoracic to lumbar apical vertebral translation is >1.2, selective thoracic fusion can be performed successfully. If any or all of these ratios are less than 1, both the thoracic and lumbar curves should be instrumented. In Lenke and Bridwell’s report that defined these guidelines,7 there was a 50% incidence of postoperative coronal imbalance when these criteria were not met. In contrast, there was no postoperative coronal decompensation when these guidelines were followed. Once the proper curve has met the strict criteria for selective thoracic fusion, it is critical to apply appropriate instrumentation principles intraoperatively. In posterior selective thoracic fusion, it is safest to fuse to the stable vertebrae. King and Moe’s classic criteria of fusing to the neutral and stable vertebrae have been shown to still be valid with use of modern instrumentation.8 Compressing between the stable and neutral vertebrae with a claw configuration on the concave correcting rod may help avoid coronal decompensation.9 “Derotation” maneuvers should be avoided. Thompson et al.,10 using pre- and postoperative CT for rotation assessment, found that derotation of the thoracic curve transmitted the rotational forces into the lumbar curve, potentially reducing the lumbar curve’s ability to spontaneously correct. The use of pure translational maneuvers, instead of rotation, has been shown to prevent postoperative coronal imbalance.11
Principles of Coronal Plane Deformity
♦ Clinical Evaluation of Coronal Balance
♦ Radiographic Evaluation of Coronal Balance
♦ Coronal Balance in Adolescent Idiopathic Scoliosis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree