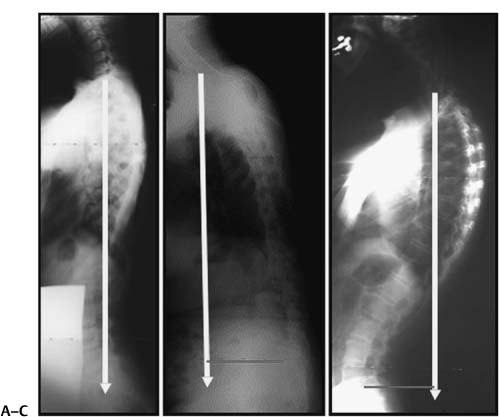
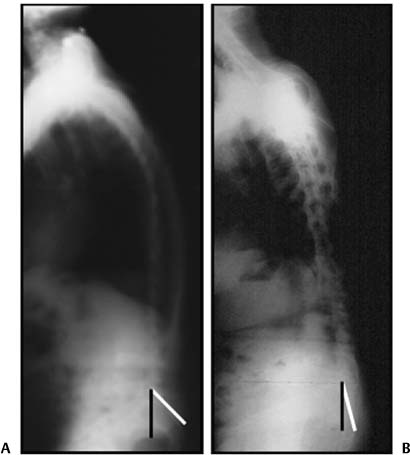
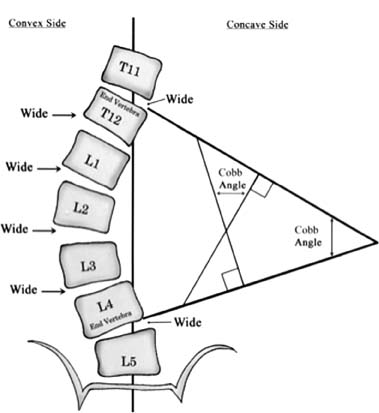
Chapter 7 The spine is a three-dimensional structure that can be defined in coronal, sagittal, and axial planes, and its motion can be described as translation, rotation, or angulation. In the coronal plane, the spine is typically straight except for an infinitesimal right thoracic convexity, which is likely relating to the aorta. Whereas the coronal plane is fairly easily defined, the normal sagittal plane is variable.1 These planes define posture. Gait and posture work best when the head and trunk fall over the pelvis. In this position, the bony center of mass falls over the femoral axis balancing the body in an upright posture. The coronal plumb line is drawn from C2 and the sagittal plumb line is usually drawn from C7 to avoid issues with the lateral radiographic quality of the dens. Thoracic kyphosis and lumbar lordosis should be directly proportional to each other,2 thus balancing the spine. A positive sagittal balance is when the C7 plumb line falls more than 2 to 4 cm in front of the sacrum. Negative sagittal balance is when the C7 plumb line falls behind the sacrum3(Fig. 7–1). At birth the spine is kyphotic,4 and with bipedal locomotion, the spine develops secondary lordotic curves in the cervical and lumbar spine. This allows balanced bipedal locomotion. An intact abdominal wall is also necessary for sagittal balance.5 Posture changes with age as muscles, tendons, ligaments, nerves, and bones undergo degenerative change. We get more cervical lordosis and thoracic kyphosis and less lumbar lordosis with age. This is typically due to osteoporotic wedging of the thoracic vertebrae and a loss of lumbar disk height. Lumbar disks account for the lordosis by not only making up one third of the lumbar height but also by being larger in the front. With degeneration, lumbar disks flatten causing a loss of lordosis. If the spine cannot compensate and adapt to these changes, the hips and legs try to compensate. Iatrogenic alterations to the spine’s alignment can accelerate this process. Because the ribs add more rigidity to the thoracic spine, it is harder to change the thoracic curve, making the lumbar spine more vulnerable to alteration, which is often a reduced lordosis. In addition, pelvic angulation has great impact on the lumbar spine. The pelvis and its rotation is the most potent compensatory structure in the spine. Figure 7–1 Sagittal alignment of the spine is typically defined as the alignment of C2 and C7 relative to the sacrum. This alignment is considered normal if C7 lies over the sacrum as in (A). It is positive if C7 falls more than 2 to 4 cm anterior to the sacrum as in (B) and negative if it falls behind (C). The relationship of C2 is still not well defined. One of the most important functions of the spine is to position the head in space, as well as allow for our bipedal locomotion. The body will attempt to return its center of gravity over the hips through hip extension, knee flexion, and posterior pelvic angulation. Ignoring the sagittal plane can produce accelerated junctional disk degeneration, bone-implant failure, flat back, and pain and degeneration in the sacroiliac, hip, knee, and ankle joints. Attention to sacral inclination is important. Leaving a patient with a vertical sacrum places them at maximum compensation with no reserve to compensate for any new imbalance. It is important that the sacrum be restored to a near normal position of ~40 degrees (Fig. 7–2). Specifically defined, sagittal balance is the alignment of C7 to the posterior superior aspect of S1 on an upright long cassette radiograph. This line is drawn from the center of C7 and should be plus or minus 2 to 4 cm from the sacral promontory. Sagittal balance is a summary picture of cervical lordosis opposing thoracic kyphosis, which opposes lumbar lordosis. The lumbar lordosis then opposes sacral inclination, and pelvic and hip angulation, to maintain a center of gravity. The film used to assess sagittal balance is a standing lateral x-ray on a 3-ft-long cassette. The patient stands upright with their arms positioned with the fingers along their clavicle and their head facing forward. The x-ray tube is positioned 6 ft from the patient. Different techniques can deal with the potential for the shoulder and pelvis to obscure the spine. Measurements used to discuss parameters associated with sagittal balance are often drawn by hand directly onto these films, but one can also use specially designed software.6 Changes in the joint angles of the lower extremities can change sagittal balance measurements, so it is important to have standardized controls for patient x-ray positioning. This can be especially difficult in the ankylosing spondylitis population, many of who undergo sagittal balance corrective procedures.7 Tight hamstrings can lead to continued imbalance even after spinal correction. This may have developed as a previous compensatory mechanism.8 Regardless, proper assessment of sagittal balance requires that the knees be fully extended and the sacrum be in a neutral rotation at 40 degrees. There are several measurements and terms used when discussing sagittal balance concepts. Kyphosis and lordosis are measured by the Cobb angle, which has been a standard. Observer and film-quality contribution have variability in measurement error of 2 to 3 degrees.9 The Cobb angle is the angle of the perpendiculars drawn from lines at the top and bottom of a curve in the spine (Fig. 7–3). Figure 7–2 The sacral orientation can dramatically affect sagittal balance. (A) A normal alignment and (B) a maximally compensated vertical alignment. Figure 7–3 The method of Cobb is a method of measuring a curve angle that has inter- and intraobserver validation to 3 degrees of accuracy and is an international standard. The sacropelvic area is key to understanding the forces and responses to sagittal balance problems. Sacral inclination is the angle between the line along the posterior border of S1 and the vertical lateral edge of a lateral standing radiograph. The center sacral line is the vertical line in an AP radiograph that goes through the center of the sacrum, through S1. Pelvic obliquity is the angulation of the pelvis from the horizontal in the frontal plane (Fig. 7–4). Pelvic inclination is the angle from a line drawn from the top of the sacrum to the top of the pubis and a horizontal line perpendicular to the lateral edge of the standing film. This can be altered by hip joint contraction. Pelvic incidence is the sum of sacral inclination and pelvic tilting.10 The pelvic incidence appears to be the main axis of the sagittal balance of the spine.10 Our bipedal standing posture is made possible by hip extension and lumbar lordosis, the latter of which is correlated with the pelvis. The pelvic incidence angle increases until age 10, then it stabilizes.11 As mentioned, the pelvic incidence correlates with sacral slope and lumbar lordosis, ensures a good standing position, and is important to sagittal balance. This depends partly on the sagittal anatomy of the sacrum, which is established as children learn to stand and walk. The sacral anatomy of spondylolisthesis patients is similar to that of infants, with more curvature and a larger incidence angle, revealing the sacral bone’s integral role to sagittal balance.12 In addition, the hyperlordosis and horizontally positioned sacrum in isthmic spondylolisthesis causes tensile forces that may result in lysis.13 A person’s posture may or may not allow them to achieve balance in the sagittal plane. Balance is defined by the C7 plumb line and its relationship to the axis of rotation about the hips, so the position of the hips on the standing x-ray film is important. In normal or congruent sagittal spin-opelvic balance, the thoracic kyphosis and lumbar lordosis balance each other. If the loss of lumbar lordosis is not associated with a reduction in thoracic kyphosis, the hips and pelvis try to correct for this, and these patients are in uncompensated balance.3 Normal cervical lordosis is 40 degrees 9.7 degrees. Some feel the occipitocervical junction is in kyphosis and the majority of lordosis occurs between C1 and C2. The lower cervical spine has an average lordosis of 6 degrees. Normal thoracic kyphosis is 20 to 50 degrees. The upper thoracic anatomy is often hard to measure on the 3-ft films, but the kyphotic apex should be at T7 or T8. Although T12-L1 usually is in 3 degrees of lordosis, it often appears flat.3 Lumbar lordosis ranges from 31 to 79 degrees, with the largest component (two thirds) being at L4-S1, and the apex at L3-L4. The degree of variability in this definition depends on whether one measures down to L5 or S1, and that varies depending on physician preference and film quality. In addition, the morphology of L5, sacral inclination, and pelvic characteristics can change the measurement of lumbar lordosis. Maintaining lumbar lordosis is very important and is the basis for the biomechanics of shaping interbody spacers and the lordotic position maintained by the Jackson table. Wedge-shaped cages increase segmental and regional lumbar lordosis, restoring sagittal alignment.14
Principles of Sagittal Plane Deformity
♦ Sacral Slope
♦ Pelvic Tilt and Obliquity
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree