39 Quality of Life in Skull Base Surgery The World Health Organization defines quality of life (QOL) as an individual’s perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, standards, and concerns. It is a broad-ranging concept affected in a complex way by the person’s physical health, psychosocial state, level of independence, social relationships, and their relationships to the salient features of their environment.1–3 For several decades, skull base surgeons have struggled to improve survival rates. Recently, increasing attention has been paid to improving and evaluating QOL. However, the surgeon’s perception of the patient’s QOL is not sufficiently accurate to correctly estimate the patient’s QOL status.4 Therefore, a patient-reported measurement is important. A detailed understanding of the different aspects of QOL may help surgeons improve the assessment and management of patients before and after treatment, and provide a patient-centered guide to the choices of medical interventions.5 QOL questionnaires may help to compare the results of surgery.3 1. Anterior Skull Base Questionnaires (ASBQ)6–8 2. Sino-Nasal Outcome Test (SNOT-22)8,9 3. ASK Nasal Inventory-9 and ASK Nasal Inventory-12 (Anterior Skull Base Nasal Inventory-9 and -12)10–12 4. Functional Assessment of Cancer Therapy–Meningioma (FACT-MNG)13,14 5. Glasgow Benefit Inventory (GBI)15,16 6. Skull Base Inventory (SBI)17 1. Karnofsky Performance Status (KPS)10,18 2. The 36-Item Short Form Health Survey (SF-36)14 3. Functional Assessment of Cancer Therapy-General (FACT-G)3,19,20 4. Sickness Impact Profile (SIP) to assess quality of life3,14 1. Patients with anterior skull base tumors undergoing open skull base surgery: ASBQ6,7,10,21,22 (Table 39.3) 2. QOL after transnasal endoscopic surgery: ASBQ5,23–25, SNOT-228,24,26 (Table 39.3) 3. Comparison of QOL after transnasal endoscopic versus open skull base resection: a. Comparisons are complicated by the heterogeneity of the two populations, the inherently different indications for each approach, the varying proportions of malignant tumors included in studies, differences in the rates of radiotherapy, as well as the varying extents of surgical resection achieved by the two approaches.10 b. However, some authors have reported the following: • Improvements in QOL seem to appear earlier in the endoscopic group.10,27 • Patients better tolerated the endoscopic procedure than the microscopic procedure.28 • Patients who underwent endoscopic surgery had significantly better ASBQ scores in physical function and impact on emotions compared with patients who underwent open surgery.23 • Malignant histological type and adjuvant radiation therapy had a poor impact on QOL in patients undergoing open surgery, whereas such differences were absent in the endoscopic group.23 4. QOL of patients with skull base meningioma29 (Table 39.4) 5. QOL of patients with vestibular schwannoma (Table 39.4) 6. QOL of patients with chordoma14 (Table 39.4) Table 39.3 Summary of QOL Questionnaires for Use in Skull Base Surgery Patients
 Definition of Quality of Life
Definition of Quality of Life
 Evaluation of QOL in Patients with Skull Base Tumors
Evaluation of QOL in Patients with Skull Base Tumors
 QOL Assessment
QOL Assessment
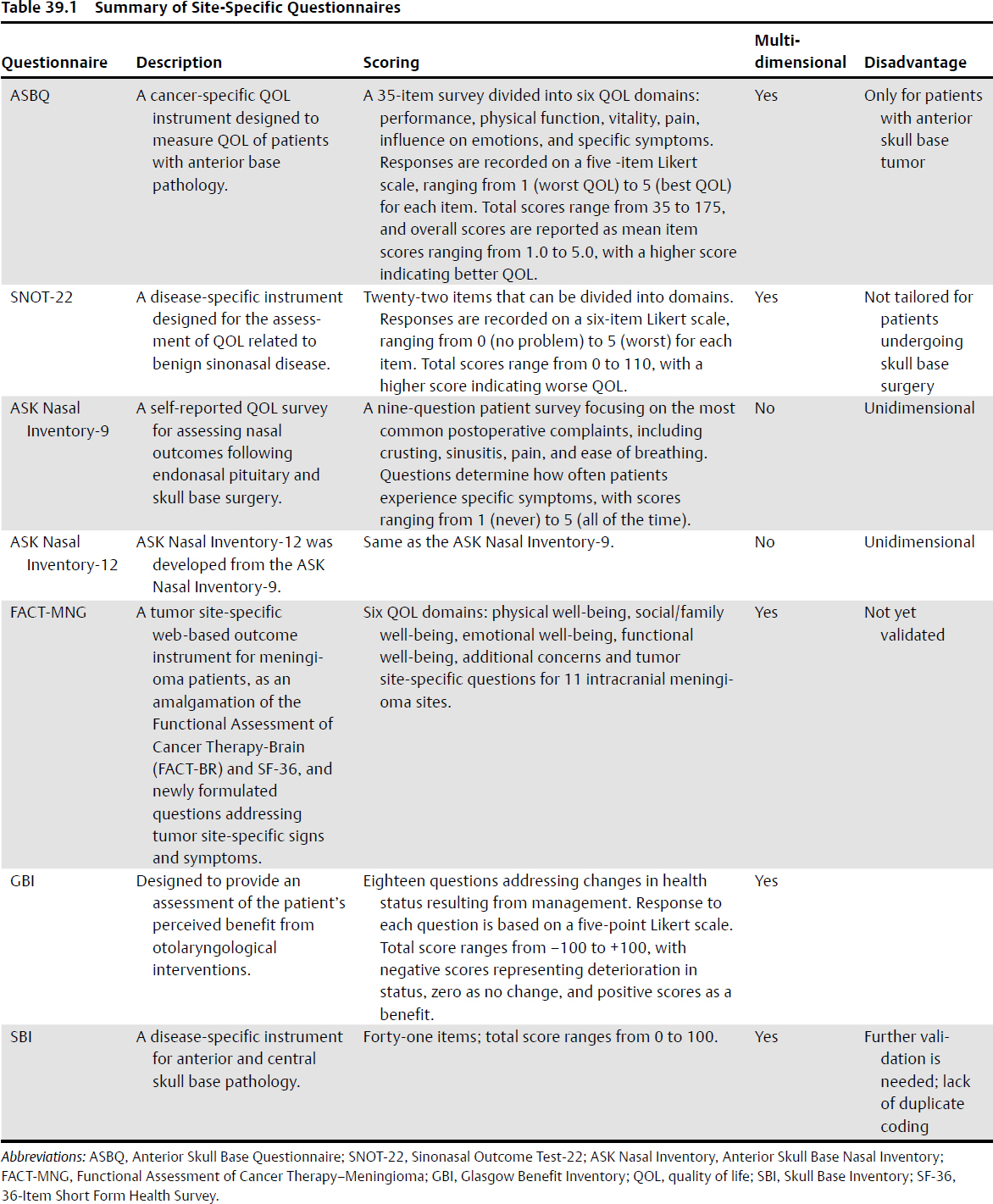
Site-Specific Questionnaires (Table 39.1)
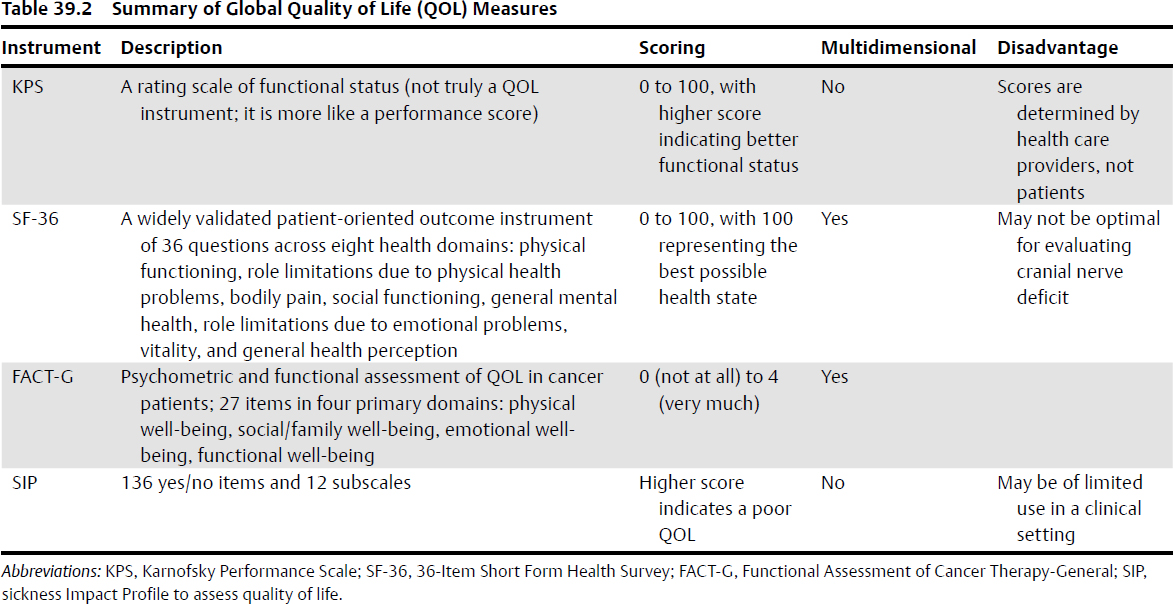
Global QOL Measures (Table 39.2)
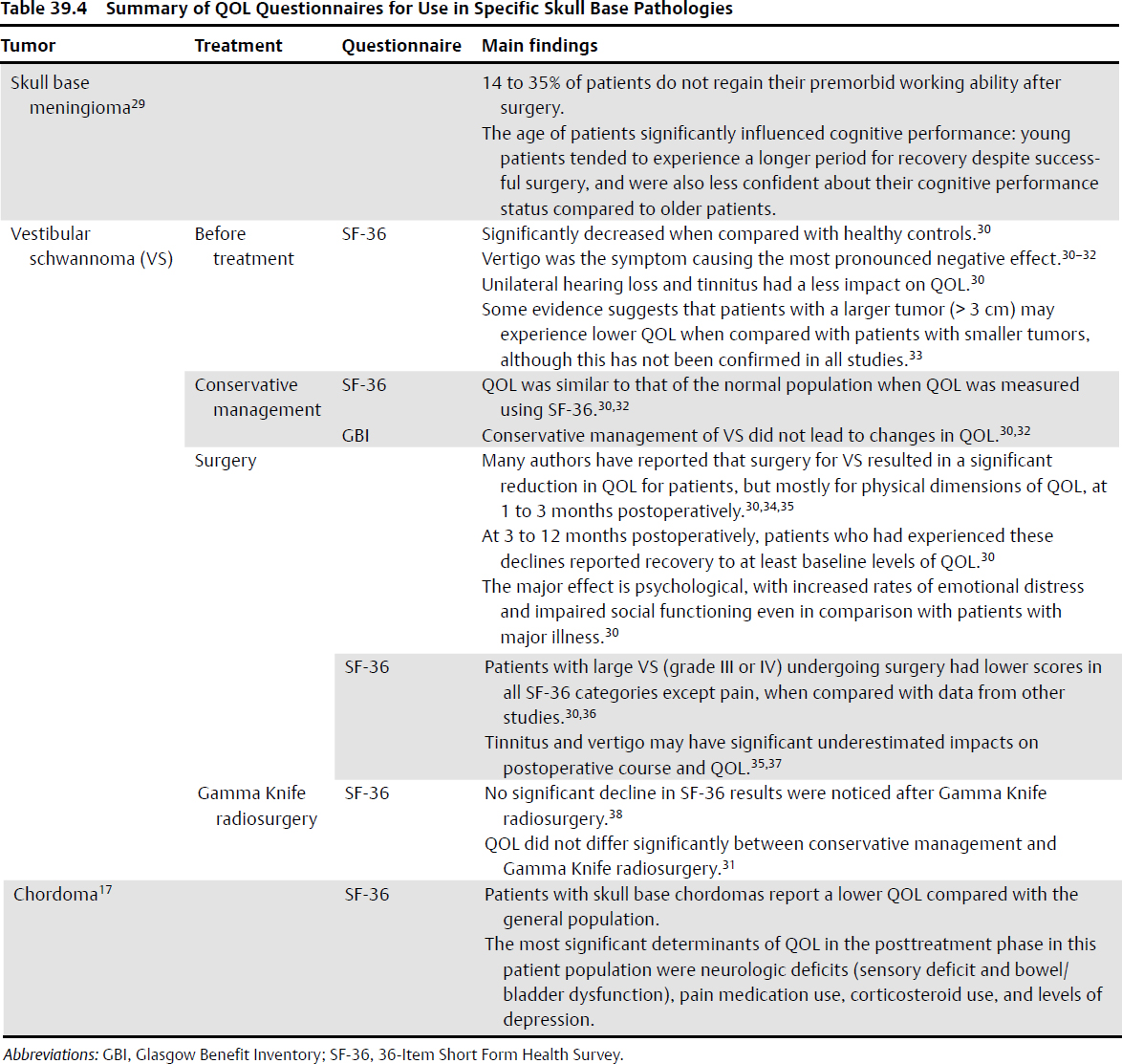
QOL Indexes Used for Various Skull Base Surgery Approaches (Tables 39.3 and 39.4)
Treatment | Questionnaire | Main findings |
Open skull base surgery | ASBQ | Overall QOL: 74% reported a significant improvement or no change within 6 months after open skull base surgery.7 Significantly improved at 12 months postoperatively.6,7,10,21,22 Worst impact: financial and emotional domains22 Negative prognostic factors: old age, malignancy, comorbidity, wide resection, and radiotherapy6,7 |
Transnasal endoscopic surgery | ASBQ | No significant association with reduced QOL Age, comorbidity, adjuvant radiation therapy, prior surgery, histological type (benign vs malignant),5,23 type of surgery (pituitary tumors vs nonpituitary tumors), anatomic region involved (cribriform, planum, sella, or clivus),23 functioning tumors were not associated with postoperative ASBQ score.24 |
| SNOT-22 | Scores worsened at 3 weeks postoperatively and returned to baseline thereafter; at 12 months postoperatively.8 Scores worsened at 3 weeks postoperatively and significant improved at the 12 months.8 Sinonasal morbidity is increased temporarily; the vast majority of patients have good QOL by 4 to 6 months after surgery.26 An expanded endonasal approach with vascularized septal flap induces more nasal symptoms (olfactory loss and posterior nasal discharge) compared with routine pituitary surgery.24 |