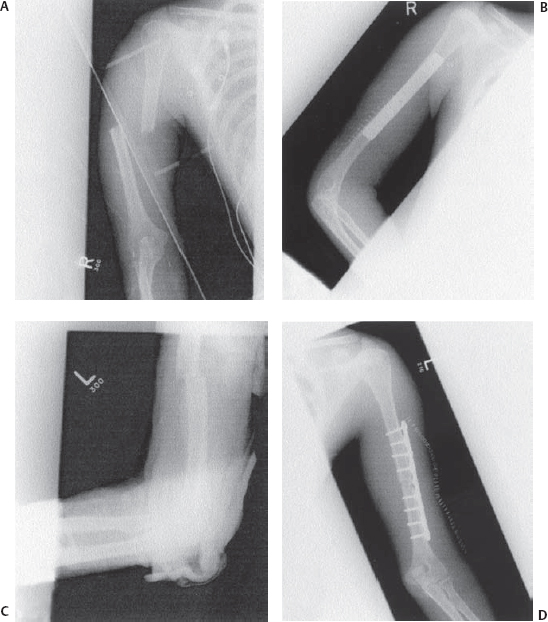
31 Radial Nerve Injury: Midhumeral Level A 29-year-old female, previously healthy, patient suffered severe multiple trauma as a result of a motor vehicle accident. Her injuries included bilateral open midshaft fractures of the humerus, bilateral femoral fractures, and multiple broken ribs. At the time of the initial presentation she had complete motor weakness of all the radially innervated muscles in both arms, except the triceps, which was intact, but little or no sensory deficit. No other neurological or vascular deficits were noted. Radiographic studies of the arm showed bilateral humeral fracture (Fig. 31–1). She underwent internal fixation of all of her long bones fractures. Examination of the left radial nerve at the time of humeral fixation revealed it to be continuous but contused and incarcerated in the fracture site. The nerve was released of the fracture site and left as such. Delayed physical and electrodiagnostic examination at 2 months showed continuing complete paralysis with no signs of reinnervation. Repeat exam at 4 months, however, showed remarkable improvement of the motor power grading Medical Research Council (MRC) 4 in the brachioradialis and wrist extensor muscles. At 9 months, the patient’s left wrist and finger extensor movements were almost back to normal. Figure 31–1 (A) Anteroposterior views of the fractured midhumerus on the right and (B) left, (C) before and (D) after fixation. On the right side, the orthopedic consultant found the patient’s radial nerve to be lacerated at a widely displaced fracture (Fig. 31–1A). The nerve ends were tagged. Six weeks later, once all her soft tissues were healed, the patient’s radial nerve was reexposed using the same lateral arm incision as the fixation surgery. However, the proximal stump was extensively scarred back to the spiral groove, and a medial arm incision was also needed to obtain proximal normal radial nerve. Four interpositional sural nerve graft cables (6 cm long) were used to repair the nerve injury, with grafts tunneled subcutaneously from the medial to the lateral arm incisions. Traumatic radial nerve injury The radial nerve, which is the continuation of the posterior cord, exits the axilla through the triangular space to reach the extensor compartment of the arm. Branches to triceps and the posterior cutaneous nerve of the arm are given before it exits the axilla. The nerve passes obliquely across the back of the humerus from medial to lateral in the spiral groove, where it gives the lower lateral cutaneous nerve of the arm and further supplies to the triceps. The nerve then runs in the posterior arm between the triceps heads. By piercing the lateral intermuscular septum it enters the anterior compartment and supplies the brachioradialis, extensor carpi radialis longus, and brachialis to divide to its terminal branches at the level of the lateral epicondyle. The superficial branch (superficial sensory radial) is purely cutaneous, whereas the deep branch (posterior interosseous nerve) supplies the muscles, which arise from the common extensor origin and the deep muscles of the extensor compartment of the forearm. In the lower half of the arm the radial nerve is relatively superficial and subject to compression (Saturday night palsy; low-placed tight blood pressure cuff), injection, penetrating injuries, and even blunt trauma. The hallmark of radial nerve injury in the axilla (e.g., compression by crutches) is triceps weakness, whereas injuries at the distal humerus (most commonly caused by humeral fracture) spare the triceps but lead to weakness of the rest of the muscles, including the brachioradialis. The sensory deficit is variable and may be absent. The radial nerve is injured in 10 to 20% of humeral fractures, which makes it the nerve most commonly injured by fractures. The injury usually happens at the time of the fracture rather than as a consequence of manipulation or the internal fixation. Nerve injuries associated with fractures and dislocations are usually classified according to Seddon’s classification (neurapraxia, axonotmesis, and neurotmesis). Nerve damage adjacent to fractures is most commonly neurapraxic, with neurotmesis least common. The latter occurs more often in open fractures than in closed ones. Radial nerve injuries usually lead to complete rather than partial deficit. Other causes of radial nerve injury include Monteggia fracture dislocation, retraction during coronary bypass surgery, low-placed intramuscular injections intended for the deltoid, and tight blood pressure cuff and as a complication of axillary block. Understanding the sequence of radial nerve supply to its innervated muscles not only helps in the initial assessment but also during assessment for nerve recovery. The brachioradialis is the first muscle and the extensor pollicis longus is the last one to recover. The extensor carpi radialis recovers before the extensor carpi ulnaris, which leads to radial deviation of the hand. Needle examination of the anconeus, which is very proximally supplied, may give the first hint for early recovery. As mentioned earlier, sensory examination is unreliable. The neurological assessment should be performed before and after both open and closed manipulation to discern worsening neurological deficit. The history and physical findings described earlier point to lesions of the radial nerve at the spiral grove. Rarely, isolated injury of the radial nerve in the axilla can occur. In these situations the triceps muscle and the sensation on the posterior aspect of the arm and forearm will be involved. With lesions of the posterior cord, involvement of the subscapularis, teres muscles, latissimus dorsi, and deltoid may be appreciated. Lesion of the radial nerve in the forearm affects mainly the extensors of the fingers (see Chapter 33 on the posterior interosseous nerve). These studies are usually done after 3 to 4 weeks from the time of the injury. Nerve conduction studies (NCSs) show conduction block across the injury site. Distal conduction velocity is present in neurapraxia, but is absent in the more severe injury grades. Electromyographic (EMG) studies show lack of denervation in neurapraxic injuries, with denervational changes in muscles after 3 weeks in the non-neurapraxic injuries. Reinnervation motor unit potentials appear after weeks to months in cases of axonotmesis. The first step in management of radial nerve or any other nerve fracture–associated injury is to immobilize and then stabilize the broken limb to minimize further nerve damage. The type and nature of the fracture, irrespective of the presence or absence of neural deficit, dictate the nature of the stabilization. It is essential to prevent further nerve insult by internal or external compression from a hematoma or cast. Most of the injuries should be managed nonoperatively because the chance of spontaneous recovery is high. The indications for immediate exploration are mostly related to the nature of the fracture, such as open or irreducible ones, or related to associated vascular injury. In such circumstances the nerve exploration should include nerve release from the entrapment, irrigation in cases of open fractures, and tagging of severed nerve but no attempts at primary nerve repair. The severed nerve should be explored a few weeks postinjury, where the extent of the longitudinal damage to the nerve is much better appreciated. Sharp, clean injuries are an exception to this approach and should be repaired immediately. Though controversial, secondary nerve injury following fracture fragment manipulation may best be treated with early exploration. The conservatively managed cases (where the lesion is in continuity) should be followed by serial clinical exams and electrical studies. Those that fail to show any signs of recovery after 4 to 6 months should be explored. The majority of the injuries are neurapraxic and carry a high chance of spontaneous recovery. This is estimated to be around 70% in all of the fractures and up to 90% when only the closed fractures are considered. Full recovery occurs in almost all of the injuries with initial partial deficit as well. Those injuries requiring nerve reconstruction also carry a very good prognosis for useful (but not complete) recovery of wrist and finger extensor function. If deficits are still present, tendon transfers are most beneficial in allowing substitutive function.
 Case Presentation
Case Presentation
 Diagnosis
Diagnosis
 Anatomy
Anatomy
 Characteristic Clinical Presentation
Characteristic Clinical Presentation
 Differential Diagnosis
Differential Diagnosis
 Diagnostic Tests
Diagnostic Tests
 Management Options
Management Options
 Outcome and Prognosis
Outcome and Prognosis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


