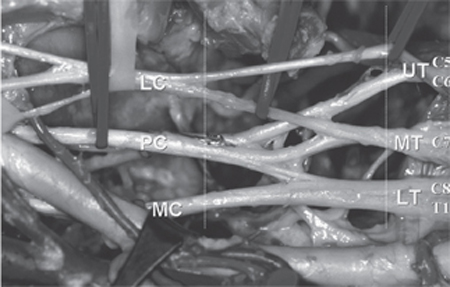
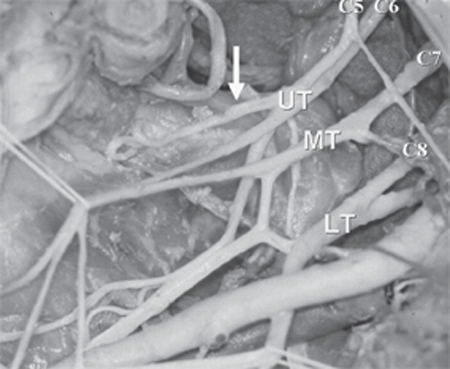
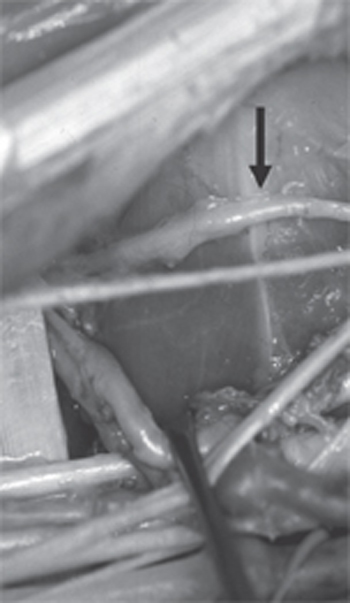
2 Upper Brachial Plexus Injury (Duchenne-Erb Palsy) A 29-year-old, right-handed male construction worker presented after sustaining blunt trauma to his right shoulder from a falling wooden column, ˜80 lb, from a second-floor level. No head trauma was sustained. The patient experienced intense pain in the right shoulder and was unable to shoulder abduct and elbow flex but was able to flex and extend the wrist and fingers. The patient was assessed at the nearest emergency room and evaluated with radiographic examinations. The x-ray of the shoulder confirmed the presence of a nondisplaced fracture of the right clavicle. The patient was managed in a shoulder sling and discharged on oral analgesia. Twelve days after the injury, the patient underwent further evaluation by an orthopedic surgeon who also found no evidence of shoulder separation/fracture and confirmed the diagnosis and management of the undisplaced right clavicular fracture. Although there was good tolerance of shoulder pain with the administration of oral analgesia, the patient continued to have difficulties with shoulder movements and had also developed severe muscle wasting of the right shoulder. The primary physician sought a neurosurgical opinion on the possibility of an upper brachial plexus injury. At 6 weeks the cranial nerve examination was normal with no evidence of a Horner syndrome. Upon inspection there was atrophy of the deltoid muscle and marked prominence of the lateral end of the clavicle. The spine of the scapula was prominent and there was pseudosubluxation of the humeral head from the glenohumeral joint. Motor strength was absent in the following muscles: deltoid, supraspinatus, infraspinatus, and biceps/brachialis. Motor strength testing was normal in the following muscles: sternocleidomastoid, trapezius, rhomboids major/minor, serratus anterior, latissimus dorsi, extensor carpi ulnaris, extensor carpi radialis, flexor pollicis longus, and flexor digitorum profundus digits 2 through 5, flexor digitorum superficialis, abductor pollicis brevis, opponens pollicis, extensor digitorum communis, extensor digiti quinti, extensor indicis, extensor pollicis, interossei, and lumbricales. Motor strength testing was reduced to 4/5 in the triceps, brachioradialis, forearm supination and pronation, flexor carpi ulnaris, and flexor carpi radialis. There was a marked decrease in light touch and pinprick in the C5 and C6 dermatomal distribution. Elsewhere sensation was normal. Reflex examination revealed an isolated absence of the right biceps reflex. The remainder of the neurological examination was normal. Upper brachial plexus injury (Duchenne-Erb palsy) The brachial plexus receives contributions from C5 to T1 spinal nerves (Fig. 2–1). The C5 and C6 spinal nerves form the upper trunk of the plexus. The middle trunk is formed by the C7 spinal nerve, and the lower trunk by the C8 and T1 spinal nerves. The upper and middle trunks are the most readily identifiable portions of the supraclavicular plexus. The upper trunk is seen adherent to and partially covered by the anterior scalenus muscle. The suprascapular nerve arises from the dorsolateral surface of the distal upper trunk at the junction where anterior and posterior divisions occur (Fig. 2–2). The nerve to the subclavius sometimes arises from the anterior aspect of the middle of the upper trunk, running medially and obliquely into the subclavius muscle. Large arterial and venous branches originating from and draining to the subclavian vessels cross beneath the upper trunk divisions and may be adherent to the nerve bundles. The middle trunk, usually smaller in caliber than the upper and lower trunks, is found beneath the anterior scalenus muscle between it and the middle scalenus muscle. The distal middle trunk may occasionally blend into or be adherent to the upper or lower trunk or both. The posterior division of the middle trunk is relatively short and combines with the posterior divisions of the upper and lower trunks to form the posterior cord. The anterior division of the middle trunk combines with that from the upper trunk to form the lateral cord. The lower trunk is relatively short and lies behind the subclavian artery that crosses over with the accompanying vein. Medially, the vertebral artery ascends anterior to the level of the trunk and anterior to the T1 spinal nerve. The lower trunk’s posterior division combines with those of the upper and middle trunks to form the posterior cord, whereas the remaining anterior division continues as the medial cord. Figure 2–1 Anterior view of the brachial plexus. The spinal nerves of the brachial plexus lie between the intertransversalis muscles in the bony troughs of their respective transverse processes, before emerging between the scalenus anterior and scalenus medius muscles. The spinal nerves in turn form the trunks, which are directed laterally and inferiorly into the apex of the axilla. UT, upper trunk; MT, middle trunk; LT, lower trunk; LC, lateral cord; PC, posterior cord; MC, medial cord. In the infraclavicular region the posterior cord lies deep or posterior to the axillary artery. The relatively small thoracodorsal nerve runs from its posterior aspect in a posterior direction to supply the latissimus dorsi muscle. The posterior cord then divides into its two major branches, the radial nerve and the axillary nerve. Several subscapular branches arise from the posterior cord and run inferiorly and obliquely. The axillary nerve passes inferiorly and laterally into the quadrilateral space to supply the deltoid muscle (Fig. 2–3). The radial nerve passes posteriorly and inferiorly accompanied by the profunda branch of the axillary artery toward the spiral groove to wind around the humeral shaft. Figure 2–2 Suprascapular nerve passing posteriorly from the upper trunk (UT). The suprascapular nerve (arrow) passes posteriorly through the suprascapular notch under the superior transverse scapular ligament along with the accompanying suprascapular vessels to supply the supraspinatus and infraspinatus muscles and provide sensation to the shoulder joint. The middle trunk (MT) and lower trunk (LT) are also shown. The lateral cord is superficial to the axillary artery at the level of the pectoralis minor in the infraclavicular region. It terminates in contributions to the median nerve and the musculocutaneous nerve; the latter runs laterally and obliquely into the coracobrachialis and biceps/brachialis muscles. The medial cord, seen lateral and inferior to the axillary vein, sends a major contribution to the median nerve joining its lateral contribution from the lateral cord, clasping around the axillary artery. The medial cord also provides important innervation to the pectoralis muscles via the medial pectoral nerve and terminates in the ulnar nerve after giving off medial cutaneous branches to the arm and forearm.
 Case Presentation
Case Presentation
 Diagnosis
Diagnosis
 Anatomy
Anatomy
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



