Cervical spondylotic myelopathy (CSM) is a clinical condition that arises secondary to degenerative changes in the cervical spinal column. 1,2 It is characterized by several clinical symptoms and signs on clinical examination that are consistent with dysfunction of the spinal cord, typically including elements of hand clumsiness and gait impairment. When the spinal cord becomes compressed as degenerative changes occur in the spine, long tract signs arise. CSM is the most common cause of myelopathy in patients older than 55 years. 3,4 Thorough patient history and physical examination can allow for early diagnosis and prevention of further neurological deficits and improve clinical outcomes. There is varied clinical presentation of CSM based on severity and cooccurring conditions that can complicate the outcomes. 2 Cervical deformities (CDs) are an increasingly recognized combination of clinical and radiographic entities. While CD can occur in the absence of neurological dysfunction, its presence has been shown to be strongly associated with CSM, as malalignment of the cervical spine itself causes the spinal cord to be compressed or altered in contour in ways to accommodate the deformity, leading to similar neurologic symptoms.
20.2 Pathophysiology of Cervical Spondylotic Myelopathy
CSM is the most common cause of cervical myelopathy. It is a degenerative, age-related condition that involves direct compression and ischemic dysfunction of the spinal cord. CSM is more common in males than in females and presently mostly in patients older than 55 years. 5 The demographic of CSM patients varies by geographical region, with the average age of CSM patients being the highest in North America and lowest in Asia. 5 Spinal cord compression can arise from anterior degenerative changes, including osteophytes and disc osteophyte complexes, as well as posterior changes and can span multiple levels of the cervical spine. 6,7 Most commonly, degenerative changes occur at the C5–C6 and C6–C7 levels, though degeneration can occur anywhere in the spine. Congenital narrowing of the cervical spinal canal (congenital stenosis) can predispose individuals to myelopathic symptoms in combination with degenerative changes over time. 8 Intramedullary hyperintensity on T2-weighted MRI of the cervical spinal cord can detect spinal cord edema which can ultimately lead to myelomalacia and demyelination associated with spinal canal volume loss caused by long-term compression. 9,10
CSM is also associated with cervical kyphosis, in which curve progression can compress and/or flatten the spinal cord and cause symptoms. Cervical malalignment can cause the anterior and posterior margins of the spinal cord compress and the lateral margins expand. When the spinal cord becomes tethered and bends around the kyphotic regions of the spine, it causes increased intramedullary pressure and neuronal loss and potential demyelination of the spinal cord. 11 Individuals with kyphotic cervical spinal deformities display shifts in the spinal cord to the anterior region of the spinal canal and presses against the vertebral bodies posteriorly at the apex of the deformity. 12,13 As the kyphosis of the cervical spine progresses and becomes more severe, there is additional mechanical stress applied to the spinal cord and the cord is stretched out on the posterior side of the vertebra. 14 When the spinal cord experiences increased elongation as a result of dynamic motion, including flexion of the spine and increased stretching as a result of the deformity, the strain becomes heightened and can lead to myelopathy. 11
20.3 Natural History of Cervical Spondylotic Myelopathy
The natural history of CSM is based on studies with inconsistent findings and clinical evaluations. 3 CSM generally presents later in life and can have periods of asymptomatic presentation and also progresses slowly. 15,16 One study reported that 95% of CSM patients had a slow, stepwise decline in neurological function with only 5% of patients experiencing rapid, dramatic deterioration. 17 Other studies have reported mixed patterns as well, with some patients deteriorating quickly in neurological function and others experiencing a slow decline. 18,19
Given that CSM is a progressive disease, there are estimates that between 20 and 60% of symptomatic CSM patients will have their symptoms deteriorate without surgical intervention. 20,21 Consistent recommendations for treatment for CSM have been difficult to establish, given that the course of CSM progression is widely varied and differs between individuals. 21,22 In assessing neurological outcomes by means of Japanese Orthopedic Association (JOA) score, one prospective study showed that 15% of patients either worsened or remained unchanged at or below a score of 14 on the JOA at 1-year follow-up, and 27% by 3 years. 23,24,25,26 In the same prospective study, they reported a mean JOA score of 15 at 1-year and a median JOA score of 15 at 10-year follow-up. Retrospective studies reported that 31% of patients deteriorated in JOA score at 3-year and 37% at 4-year follow-up. 27,28
Worsening neurologic or functional symptoms lead to some patients undergoing surgical treatment. The rate of conversion from nonoperative to surgical treatment for CSM ranged from 4 to 40% in studies with 3- to 7-year follow-up. 19,27,28,29,30,31,32,33 One study reported that cervical hypermobility, segmental kyphosis, and instability were factors for conversion to surgical treatment. 30 Deterioration is also associated with a long duration of symptoms, and rigorous conservative treatment showed higher improvement rates than less intense methods of conservative treatment. 32 The circumferential spinal cord compression in the segment with the maximum compression on an axial MRI was a significant prognostic factor for surgical treatment in a subset of CSM patients. 33 Another study reported that surgery for CSM was associated with improvements in functional, disability-related, and quality-of-life outcomes, regardless of baseline severity of the disease. 34
20.4 Clinical Presentation of Cervical Spondylotic Myelopathy
Given that the spinal cord involves nerves that carry signals to diffuse regions of the body, patients with CSM can experience a wide range of symptoms. Commonly, patients present with upper extremity symptoms such as hand weakness and numbness, and motor dysfunction characterized by the inability to perform fine motor skills, difficultly buttoning a shirt, and tendency to drop objects. 15,35 Patients with CSM also commonly present with balance problems and unsteady gait. Less than 50% of CSM patients present with neck pain, though this rate becomes much higher for patients with CD. Lhermitte sign and sphincter dysfunction can also present in CSM patients, though at lower rates. More severe CSM progression may present at paraparesis and hand numbness. Most commonly, CSM involves cervical levels C5–C6, C6–C7, followed by C4–C5 and C3–C4. Early recognition of symptoms and treatment prior to spinal cord damage or deterioration of symptoms is critical for optimal clinical outcomes.
20.5 Other Cervical Spondylotic Myelopathy Etiologies Associated with Cervical Deformities
20.5.1 Ossification of the Posterior Longitudinal Ligament
Ossification of the posterior longitudinal ligament (OPLL) can elicit cervical spinal canal stenosis. 36,37 OPLL is one of the most common causes of cervical myelopathy particularly in the Asian population, with the highest prevalence found in Japan (1.9–4.3% incidence), with lower rates found in Korea, the United States, and Germany. 5,37,38,39 As OPLL progresses, it eventually causes compression of the spinal cord and myelopathy. 40,41,42 Postlaminectomy kyphosis after treatment for OPLL has been reported in the literature and cervical malalignment is a crucial consideration when treating OPLL. 43 Cervical lordosis (CL) is important in performing a laminoplasty for OPLL with an occupying ratio greater than 60%, as suggested by findings that patients who underwent a laminoplasty and achieved a good outcome had a greater degree of CL even though they also had a larger ossification-occupying ratio. 44 The K-line was developed to assess cervical alignment and OPLL size using only one parameter that aids surgeons in decisions regarding the surgical approach for patients with cervical OPLL while taking into account cervical malalignment. 45 The K-line is drawn from the midpoints of the spinal canal at C2 to the midpoint at C7 and then OPLL cases can be divided into two cases: K-line (+) where the OPLL does not exceed the K-line and K-line (-) where OPLL extends beyond the K-line. 45
20.6 Atlantoaxial Dislocations
Atlantoaxial dislocations are a loss of stability between the atlas and the axis that causes a loss of normal articulation between the joints, caused by traumatic, inflammatory, idiopathic, or congenital abnormalities. 46,47 Myelopathy is one clinical presentation of atlantoaxial dislocations that can lead to more severe clinical presentation and increased morbidity and mortality associated with the atlantoaxial dislocation. 46,48,49,50 Though rare, atlantoaxial dislocations are associated with complex CDs that often require surgical intervention. It has been shown that the subaxial cervical spinal alignment is in part determined by the direction of the dislocation, with anterior dislocations causing hyperlordosis of the subaxial cervical spine and posterior dislocations causing straightening or kyphosis, all in an effort to maintain overall balance. 47
Swan neck deformities of the cervical spine have been documented first in patients after multilevel cervical laminectomies, tumor resections, and osteomyelitis and then after upper cervical procedures. 51,52,53,54 More recently, studies have looked at the preoperative development of swan neck deformities in patients with chronic atlantoaxial dislocations with abnormal kyphosis at the occipitoaxial segment and subaxial hyperlordosis. 55 Another study investigated whether abnormalities in subaxial alignment could be reversed following surgical correction of occipitoaxial malalignment for patients with swan neck deformities secondary to chronic atlantoaxial dislocation, defining a swan neck deformity as lordosis of the subaxial spine greater than 30 degrees with upper cervical kyphosis (less than 0 degrees). The authors found that these swan neck deformities can be reversed following correction of the primary upper CD. 56
20.7 Chiari Malformations
Chiari malformations, most commonly type 1, present with the cerebellar tonsils below the foramen magnum, giving rise to brainstem and spinal cord compression and disruptions of cerebrospinal fluid. 57,58,59 A case report of a 51-year-old patient with previous intradural surgery for Chiari malformation presented with recurrent cervical myelopathy and progressive kyphotic CD and spinal cord tethering. 60 Spinal malalignment is frequently associated with Chiari 1 malformations, though the presentation varies significantly. 61,62
20.8 Cervical Spondylotic Myelopathy and Cervical Deformity
20.8.1 Cooccurrence of Cervical Deformity and Cervical Spondylotic Myelopathy
CSM with associated cervical kyphosis results from the progressive subluxation of the apophyseal joints from facet joints and discs degeneration. 12 The cooccurrence of CD and CSM has been previously reported for patients mostly older than 60 years, with the majority of patients being male. 12,63 The operative treatment for patients with concurrent CD and CSM can be higher than for a patient with isolated CD or CSM, given that progression of the kyphotic deformity can lead to worsening and possibly irreversible spinal cord compression and myelopathic symptoms. Surgical correction of both the malalignment and the spinal cord compression from the CSM can help mitigate further neurologic deficit and help improve patients’ overall quality of life. Given the known natural history of CSM and its often rapid progression once symptoms present, early surgical intervention for these CD patients with CSM can help optimize outcomes.
CD is a complex group of disorders with etiologies including spondylosis, inflammatory arthropathy, posttraumatic, postsurgical, and others. 64,65 CDs occur in both the coronal and sagittal planes; however, sagittal plane deformities are more frequent. 66 Deformities can either be primary (often congenital) or secondary (iatrogenic cause or ankylosing spondylitis). 67,68 Cervical kyphosis is the most common cervical spine deformity and is often the result of iatrogenic causes, including postlaminectomy kyphosis. When the deformity begins, it leads to postural shifts including the head and neck shifting forward and the change in load on the spine can influence further spinal deformities. Additionally, dropped head syndrome leading to a flexible chin-on-chest kyphotic deformity has been reported in conjunction with CSM and, while rare, leads to debilitating consequences for patients’ quality of life. 69 These clinical presentations highlight the similar and interconnected degenerative processes of CD and CSM, as the compressive effect of multilevel disc degeneration is exacerbated by the kyphosis of the vertebrae.
The relationship between alignment of the upper cervical and subaxial spine has been documented in previous reports. 70,71,72 Studies have shown that changes in subaxial alignment can result following upper cervical fusion procedures, primarily in atlantoaxial dislocation patients. One study showed that when the atlantoaxial joint was surgically fixed in a hyperlordotic position, the subaxial spine responded with kyphotic sagittal alignment. 73 Another study showed that for complex swan neck deformity patients involving alignment changes of the upper cervical and subaxial spine, the sagittal alignment of the subaxial spine can still be reversed when the alignment in the upper cervical spine is treated. 56 They also found that age was a significant and independent predictor that was related to the amount of change in alignment of the subaxial spine after surgical correction of the occipitoaxial malalignment, suggesting that younger and more flexible spines can better compensate in order to maintain proper horizontal gaze. One case report described a patient with acute kyphotic swan neck CD that caused spinal canal narrowing and spinal cord compression after cervical laminectomy. 74
20.8.2 Common Classification for CD Incorporating CSM and Radiographic Components
Recent advances in CD correction techniques and improved understanding of regional sagittal alignment of the cervical spine have led to the development of a new classification system for CD. 2 This classification system developed by Ames-ISSG et al primarily characterizes CD according to the apex of the deformity whether in the cervical, thoracic, or the cervicothoracic junction with added modifiers in the form of cervical sagittal vertical axis (cSVA), T1 slope minus cervical lordosis (TS–CL), chin–brow vertical angle (CBVA), SRS–Schwab modifier, and modified JOA (mJOA). The incorporation of a myelopathy modifier was found to be vital. Progressive cervical kyphosis has been associated with development of myelopathy, through draping and tensioning of the spinal cord over anterior pathology. This results in direct neural injury and ischemic changes. 3,4,5,6,7 Surgical correction for CD has led to improvement in radiographic alignment and patient-reported outcomes related to pain, disability, and neurologic and myelopathic improvement. 8
20.8.3 Relevant Radiographic Parameters
The most common radiographic parameters to assess cervical alignment include CL, cSVA, TS–CL, and CBVA. Normative values for CL range from 15 degrees ± 10 degrees in young adults and 25 degrees ± 16 degrees in patients older than 60 years. 75 While normative values for cSVA have been reported as 1.5 cm ± 1 cm, reports suggest that a cSVA greater than 4 cm is correlated to inferior health-related quality-of-life (HRQOL) scores. 76 TS–CL takes into account both the CL and T1 slope and studies have shown that the parameter should be less than 17 degrees and higher TS–CL values are associated with worse clinical outcomes. 77 CBVA values ranging from 1 to 10 degrees have been used in the CD classification system of Ames and this parameter is useful especially in the management of severe, rigid, kyphotic CDs, since the loss of horizontal gaze significantly impacts quality of life and daily activities. 78,79
20.8.4 Correlation of Cervical Deformity and Cervical Spondylotic Myelopathy Improvement with Outcomes
Multiple studies have examined the relationship between radiographic parameters and HRQOL scores, both in asymptomatic and spinal deformity patients, and correlations between the two measures have been well established. 80 Tang et al concluded that a C2–C7 SVA greater than 4 cm was associated with worse Neck Disability Index (NDI) scores at 6 months postoperative interval following correction of CDs. 80 One of the limitations of their study was the inability to comment on the preoperative cervical alignment and HRQOL outcomes due to lack of available data. Recently, Iyer et al studied the relationships between neck disability and preoperative cervical alignment in patients with degenerative cervical spine disease. They concluded that increased CL and T1 slope correlated with decreased NDI. Increasing cSVA was found to be an independent predictor of high preoperative NDI. 81 Both these studies prove the importance of restoring a cSVA less than 4 cm as an alignment goal while treating cervical sagittal malalignment. It is important to note, however, that restoration of cervical alignment is not the only factor contributing to improved patient outcomes following CD-corrective surgery. Postoperative myelopathy improvement may also contribute to improved patient-reported outcome measures, but the extent of this influence is ill characterized in the literature. 80,82
In addition, recent work focusing on prospectively collected severe CD patients has shown that improvements in myelopathy symptoms and mJOA functional scores were significantly associated with superior 1-year postoperative outcomes in comparison to patients who improved only in alignment parameters. 83 This work, along with other preliminary investigations, indicates a strong connection between CD alignment correction and improvement and patient-reported outcomes, with myelopathy improvement as a key driver of patient-reported outcomes for patients undergoing CD surgical correction.
20.9 Spinal Cord Symptoms Resulting from Cervical Deformity
Progressive cervical kyphosis is associated with myelopathy. Deformity of the spine causes the spinal cord to bend and elongate against the vertebral bodies, which increases spinal cord tension. 13,84,85 With curve progression, the spinal cord becomes compressed and flattens, 86 as described previously. Spinal cord tethering leads to increased intramedullary pressure and neuronal loss and demyelination of the cord. Additionally, when the blood vessels on the spinal cord flatten, blood supply is reduced, which causes an abnormal blood supply network. One study found a significant correlation between the degree of kyphosis and the amount that the spinal cord was flattened in a population of small game fowls. 86 Further study using angiography showed that the anterior portion of the cord displays decreased vascular supply. Sagittal alignment of the cervical spine and cervical myelopathy are closely linked. When degenerative changes in the spine occur and osteophytes form, in addition to ligamentous and facet hypertrophy, cervical spinal stenosis develops and can compress the spinal cord. Stenosis and compression on a long-term scale can lead to demyelination and necrosis of gray and white matter due to hypovascularization of the cord. 87 Changes in the spinal cord can first be detected by high signal intensity of the cord at the level of the compression and then by the “snake-eyes” appearance of myelomalacia or necrotic changes. 88
20.10 Surgical Management of Cervical Deformity and Cervical Spondylotic Myelopathy
20.10.1 Technical Goals for Patients with Cervical Deformity and Cervical Spondylotic Myelopathy
Cervical deformity without compression of the neurologic elements may be treated without central decompression. The addition of myelopathy requires that central decompression be performed in addition to reduction of deformity and stabilization if adequate decompression of the spinal cord is not achieved with realignment alone. The intrinsic damage to the spinal cord causing myelopathy may be as a result of direct compression or it may be a result of traction placed on the cord by malalignment. The surgeon has two interrelated considerations prior to deciding the most appropriate surgical approach. The first is deciding the method for correcting the deformity, and the second consideration is the approach to neural element decompression. In selected patients, cervical realignment alone may be sufficient to decompress the neural elements. Presented but yet unpublished data show that for patients with CD and myelopathy symptoms, realignment alone improves symptoms in a subset of patients. 83 Other variables requiring consideration include age and medical comorbidities, global sagittal alignment, cervical sagittal alignment, rigid or flexible CD, smoking status, body mass index, prior cervical spine surgical approaches, the combined presence of a thoracolumbar deformity, ventral versus dorsal compression, focal or diffuse compression, and etiology of the compressive component. Approaches to the cervical spine can be ventral, dorsal, or a combination of both.
The general options for posterior central neural decompression include standalone laminectomy, laminoplasty, and fusion. Cervical alignment and lordosis is an important factor when deciding on an operative approach. Isolated laminectomy is the least invasive procedure but is associated with increased incidence of postoperative kyphosis, even in patients with straight (30%) and lordotic (14%) preoperative alignments. 43 Standalone laminectomy is even less palatable in the setting of cervical spinal deformity.
A literature review published in 2013 noted the overall evidence for effectiveness of laminoplasty compared to laminectomy and fusion for treatment of CSM is insufficient to recommend one procedure over the other. 89 Moreover, only two articles examined the development of kyphotic deformity between the two procedures. One article looking at patients with multilevel CSM found laminectomy and fusion to have a higher rate of kyphotic deformity development than laminoplasty (0 vs. 15%). 90 This study also found significantly increased loss of lordosis in laminectomy and fusion group versus the laminoplasty group. In CSM patients with preoperative CL, laminoplasty has shown to increase lordosis slightly (1.8 degrees) relative to preoperative lordosis as well as maintain 87.9% of preoperative flexion/extension range of motion. 91 Perhaps more intuitively, a recent large case series comparing laminoplasty versus laminectomy and fusion found no difference in postoperative sagittal cervical Cobb angle, despite the fusion group having significantly less preoperative lordosis (5.8 vs. 10.9 degrees). 92 Fusion was also associated with improved neurologic outcome as measured by the Nurick score; however, it had significantly longer operative time and blood loss. Neck pain was similar between groups. This study underscores the bias preventing matched comparison between these two procedures in the setting of CD. Specifically, in patients with worse preoperative sagittal balance, surgeons are unlikely to randomize between the two posterior options and will choose laminectomy and fusion over laminoplasty.
The general options for anterior neural decompression include anterior cervical discectomy and fusion, anterior disc replacement, corpectomy, combination of anterior cervical discectomy and fusion, and corpectomy. It has been recommended that patients with CSM without dorsal compression will have superior neurological recovery, less neck pain, and superior correction of sagittal alignment if multiple anterior discectomies are performed instead of corpectomy or combined discectomy–corpectomy approaches. 93
20.10.2 Surgical Goals for Patients with Cervical Deformity and Cervical Spondylotic Myelopathy
There is a paucity of literature comparing the effect of anterior versus posterior surgical approach on operative outcomes in patients with sagittal CD and CSM. Uchida et al compared anterior decompression and fusion with posterior open door laminoplasty in patients with CSM who also had cervical kyphosis of at least 10 degrees on lateral radiograph in the neutral position (average: 15.9 degrees ± 5.9 degrees). Their results showed a significantly smaller kyphotic angle in neutral and flexion positions in the anterior spondylectomy approach compared with the laminoplasty approach. 12 A more general review comparing anterior versus posterior approach for CSM (not restricted to those with deformity) found no clear advantage to either approach. Neurological outcome based on mJOA was similar, rates of C5 palsy were similar, canal diameter was larger with posterior surgery, infection rate was lower with anterior surgery, and dysphagia was lower with posterior approach. 94
Ideal degree of deformity correction is not established. An analysis of 56 operative CSM cases found no correlation between cervical sagittal balance (C2–C7) and myelopathy severity as measured by mJOA. 95 However, this was not a cohort specifically with deformity. In patients undergoing posterior cervical spine fusion, sagittal CD as measured by C2 SVA has been shown by Tang et al to correlate with worse postoperative HRQOL. They proposed C2–C7 SVA greater than 40 mm as the threshold beyond which HRQOL will be negatively affected. 76 This suggests reducing C2–C7 SVA to less than 40 mm as a minimal threshold for CD correction; however, further study is necessary to confirm this. Other radiographic parameters to assess when correcting CD include T1S–C2–C7 lordosis less than 15 degrees and CBVA between -10 and + 20 degrees. Patients with a CBVA less than -10 degrees have significantly lower scores on horizontal gaze testing. 78 An upper CBVA limit of 20 degrees has been proposed, but perhaps an upper limit of 10 degrees may be a superior goal. 96 The mismatch between T1 slope and CL (T1S–C2–C7 lordosis) attempts to account for the increasing lordotic requirements as the T1 slope increases. It has been proposed by expert opinion that less than 15 degrees is a reasonable goal. 79 It should again be noted that the earlier-mentioned alignment parameters are established in the literature as generally accepted values, but each patient must be evaluated and treated based on their particular needs and deformity. From a functional deformity perspective, operative goals should be to restore forward gaze, reduce muscle strain, and minimize axial neck pain. Lastly, it has been shown that dynamic spinal cord compression increases in extension more so than flexion in all kyphotic deformity subtypes. 97 This suggests that it would be prudent to perform decompression of the spinal cord prior to attempted reduction of deformity, particularly if the reduction of the deformity involves extension.
In summary, in the setting of CSM and cervical spinal deformity, the operative goals are twofold, neural decompression and reduction and stabilization of the CD. There is a paucity of evidence to recommend specific surgical approaches. The surgeon must individualize the approach to the patient based on the location of compression, the curvature of the deformity, and their comfort with various approaches.
20.10.3 Case Examples of Patients with Concurrent Cervical Deformity and Cervical Spondylotic Myelopathy
We present three case examples of patients with concurrent CD and CSM. In ▶ Fig. 20.1, the patient improves in cervical alignment only postoperatively. In ▶ Fig. 20.2, the patient improves only in myelopathy, with cSVA worsening postoperatively. ▶ Fig. 20.3 displays a CD patient with CSM who improves in both cervical alignment and myelopathy symptoms after surgical correction.
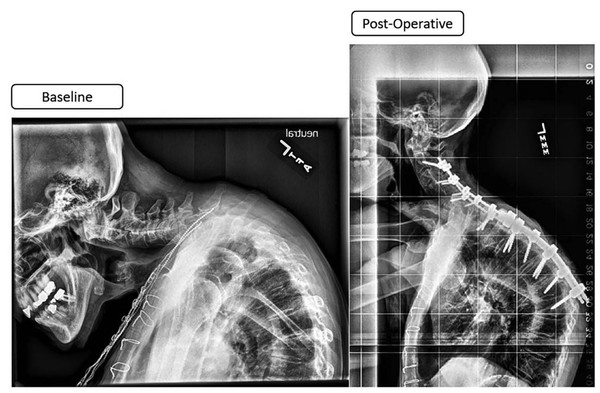
Fig. 20.1 Cervical deformity patients with myelopathy who improved only in alignment. Pre- and postoperative radiographs of a cervical deformity patient with baseline myelopathy symptoms. This is a 73-year-old female patient with a TS–CL of 77 degrees and cSVA of 90 degrees. The baseline NDI score was 42 and mJOA was 13. She underwent a C2–T7 posterior fusion, with a three-column osteotomy at T2. Postoperative improvement was seen in alignment, with TS–CL decreasing to 34 degrees and cSVA to 54 degrees, though myelopathy symptoms remained the same (post-op mJOA score of 14). cSVA, cervical sagittal vertical axis; mJOA, modified Japanese Orthopedic Association; NDI, Neck Disability Index; TS–CL, T1 slope minus cervical lordosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


