Fig. 1
Cerebral blood vessels. Dual echo susceptibility weighted imaging (SWI) of a 75-year-old healthy male (voxel sizes 0.4 × 0.5 × 0.6 mm3) showing both the cerebral arteries and veins. Depicted are a transverse and coronal first echo 3D time-of-flight (TOF) arteriogram (a, b) and a transverse and coronal second echo T2* venogram (c, d)
Most vascular imaging applications are based on visualizing the lumen of blood vessels. However, many pathological processes arise in the vessel wall. With high field strength MRI, it has become possible to depict the intracranial vessel wall and its pathology with increasing detail. This has recently been demonstrated by our study group using magnetization preparation inversion recovery TSE (MPIR-TSE) at 7 T [12]. This allows the study of plaques in intracranial vessels and their role in stroke (Fig. 2).
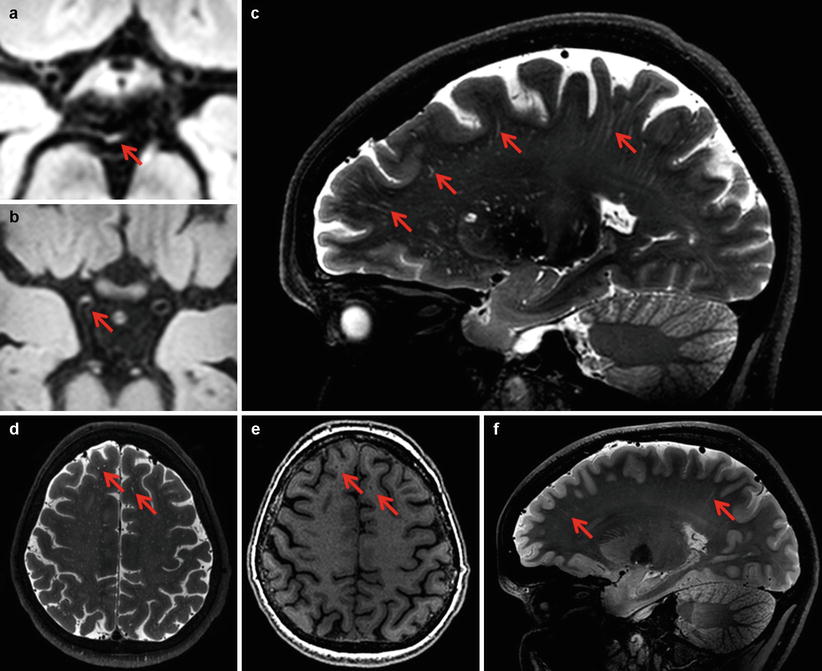
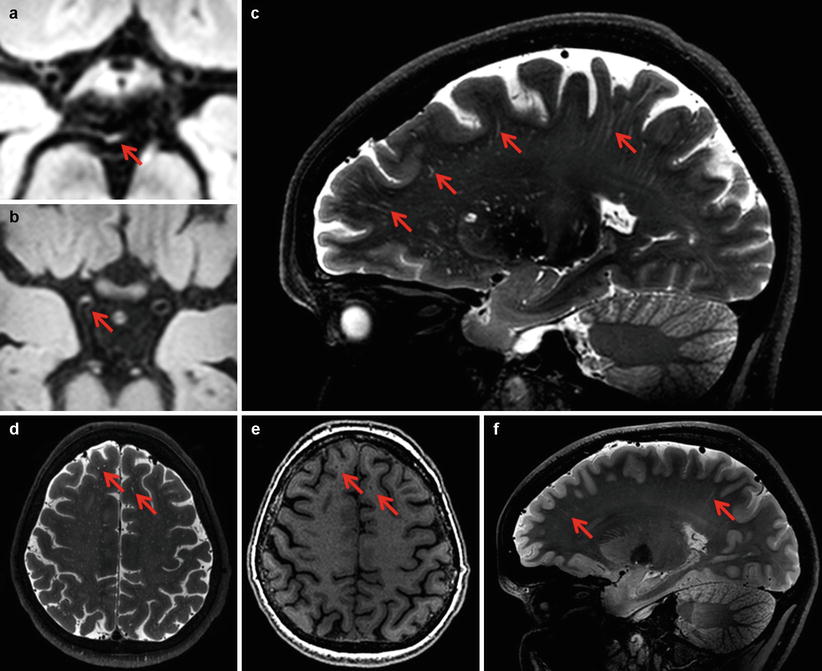
Fig. 2
Vessel walls and perivascular spaces. Transverse 3D MPIR-TSEimages (voxel sizes 0.8 × 0.8 × 0.8 mm3) of a 58-year-old male with amaurosis fugax based on thrombo-embolism, with a focal hyperintense lesion in the basilar artery (a, arrow) and of a 49-year-old male with multiple transient ischemic attacks based on intracranial atherosclerosis, with a focal hyperintense lesion in the distal ICA (b, arrow). Sagittal T2 weighted (voxel sizes 0.8 × 0.8 × 0.8 mm3) image of a 66-year-old female shows numerous perivascular spaces throughout the brain (c, arrows). Enlarged perivascular spaces (arrows) in the same subject on a transverse T2 (D) and T1 weighted (voxel sizes 1.0 × 1.0 × 1.0 mm3) image (e, arrows). On a sagittal T2 weighted image of a 19-year-old male several perivascular spaces are visible (f, arrows)
Perivascular spaces (PVS) are extracerebral fluid filled spaces that surround brain arteries, arterioles, veins, and venules. PVS are physiological structures that are present in all individuals and course from the cortical or basal brain surface into the brain parenchyma. With conventional MRI, only the abnormal, enlarged PVS can be visualized. These enlarged PVS on conventional MRI are thought to be a correlate of SVD and are associated with dementia [5, 6]. 7 T MR imaging now allows visualization of normal, non-enlarged PVS, for example, in young adults (Fig. 2). Furthermore, by combining images of PVS and blood vessels, the relationship between these structures can now, for the first time, be assessed non-invasively. High field strength MRI is thus likely to further our understanding of (enlarged) PVS as a marker of SVD.
Parenchyma
Conventional MRI markers of SVD, including WMHs and lacunar infarctions, do not fully capture the burden of vascular brain damage in aging and dementia. In this context, microvascular lesions, in particular CMBs and cerebral microinfarcts (CMIs), are attracting increasing attention. Autopsy studies have demonstrated that these lesions are common and are clearly correlated with impaired cognition, also in patients diagnosed with Alzheimer’s disease (AD) [9, 11]. Because CMIs are small (reported sizes vary between 50 μm and a few mm), they go undetected on conventional MRI [2]. The paramagnetic effects of hemosiderin allow the detection of CMBs with conventional MRI, despite limited size, but CMB detection is facilitated at higher field strength [7]. In a study done in our group by Conijn et al., it was shown that on 7 T dual echo T2* weighted images, up to three times as many CMBs could be detected, as compared to 1.5 T 3D T2* weighted images [4].
In one case report, 7 T T2* weighted images with short echo time, used for noncontrast enhanced MR angiography, revealed a direct relationship between several CMBs and a small penetrating artery in a single scan acquisition of a 42-year-old male patient who presented with acute headache, dysphasia, and severe hypertension [1]. This is another example of the high sensitivity of 7 T MRI, allowing visualization of the hemorrhages together with the related “leaking” small arteries (Fig. 3).
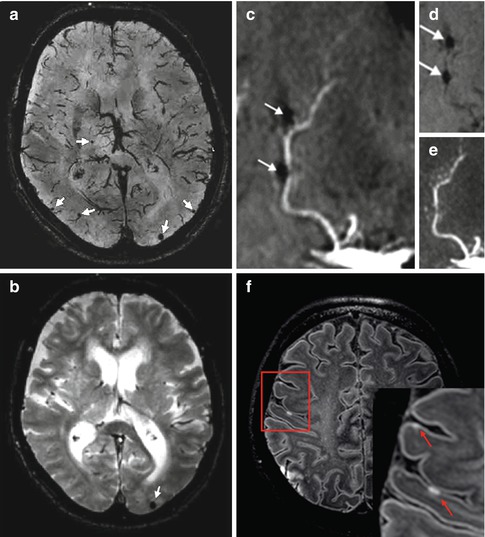
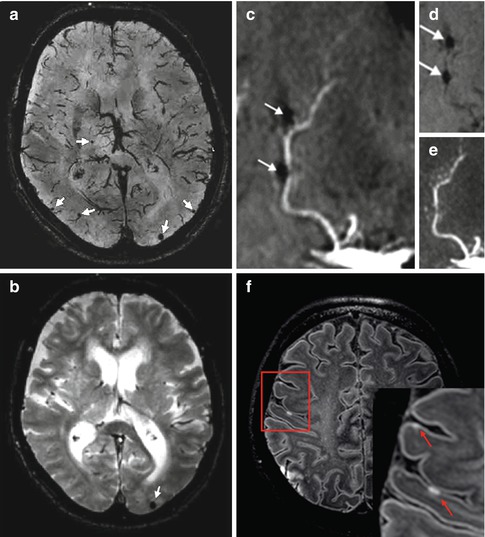
Fig. 3




Microvascular brain lesions. A minimum intensity projection of a T2* weighted image (second echo) of an 89-year old female with mild cognitive impairment shows several microbleeds in one slice (a). For comparison the 3T T2* weighted image of the same subject is shown, where only one microbleed is visible (b). A combination of a coronal minimum (d) and maximum (e) intensity projection generated from time-of-flight (TOF) angiography images reveals a direct correlation between microbleeds (which are, at 7T, even visible at the short TE used in TOF) and a penetrating artery in a 42-year old male (c). A fluid-attenuated inversion recovery (FLAIR) image from a 57-year old female with a history of atrial fibrillation who presented with aphasia and left-sided hemiparesis based on cortical ischemia in the right middle cerebral artery territory show small cortical hyperintensities (arrows), which represent minute acute ischemic lesions (f, box indicates enlarged inset)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








