The practice of individualized medicine is on the rise in all fields of medicine. When discussing risks and benefits of a particular procedure with patients, surgeons often rely on average values and use gestalt to estimate whether a given patient has higher or lower than average risk. Risk stratification research focuses on factors that are associated with severe complications and/or poor outcomes in order to improve preoperative predictions of risk. As risk stratification tools grow progressively more reliable and comprehensive, it becomes possible to give patients a more accurate assessment of their personal risk undergoing a given procedure.
Spine surgery, including complex cervical surgery, has a very high rate of complications. In a prospective database of 78 cervical deformity patients, 44% had at least one complication and 24% had at least one major complication. 1 Among those patients who underwent three-column osteotomy procedures in the cervical spine, the complication rate was 60% and the reoperation rate was 33%. 2 Advances in surgery and anesthesia have made surgery available to older patients with more comorbidities by reducing the physiologic impact. 3 Given this degree of risk associated with cervical spine operations, improved preoperative risk stratification is essential to identify those patients at highest risk of severe complication. It is important that those patients who are at highest risk may also be those who have the greatest potential benefit. In adult spinal deformity, despite the higher rate of complications in older patients (62% in those older than 75 years 4), these patients also tend to experience greater improvement in pain and disability with surgical treatment. 5 Given the large discrepancy between potential benefit and potential harm, adequate preoperative risk stratification strategies are essential, particularly for elderly patients undergoing high-risk procedures, to minimize morbidity and mortality.
Risk stratification is also an important tool in cost-effectiveness strategies, 6,7,8 development of quality metric ranges in health policy, and accurate comparisons of intersurgeon complication rates. Minimization of complication incidence, identification of patients most likely to benefit from postoperative intensive care, and preoperative discharge planning are all potential cost-effectiveness methods that rely on adequate risk stratification. Additionally, when analyzing interventions and changes in surgical technique for efficacy, accurate risk stratification of patients is essential to control for patient factors. Health policy interventions are already comparing hospital outcomes to impact payments. As comparing interfacility and intersurgeon complication rates becomes standard practice, accurate risk stratification analysis of patients is essential to weight complication rates by patient population risk. If the current system continues to move toward bundled payments, it is important to quantify risk of complications depending on specific procedure and patient factors since payments need to be adjusted accordingly. All of these upcoming challenges in health policy rely on accurate patient and procedure risk stratification.
Given the importance of accurate risk stratification, this chapter investigates the current status of risk stratification tools, how these tools can be applied specifically to complex cervical deformity, and where further efforts are needed. Fortunately, risk stratification has become increasingly present in recent research, with many new tools and strategies being developed. As these methods become more quantitative and prognostic, avoiding inappropriately restrictive health policy regulations is essential to prevent some patients from receiving necessary care.
17.2 Retrospective Regression Models
By using regression models, researchers have identified many factors associated with worse outcomes based on complication incidence, reoperation rate, quality of life, length of hospital stay, readmission rate, and discharge to facility. 9 These factors can be divided into patient factors (▶ Table 17.1) and surgical factors (▶ Table 17.2). 9,10,11,12 However, given the number of identified contributors to preoperative risk, it is impossible to accurately assess and weigh each of these measurements in a routine office visit. In order to remedy this issue, risk tools were developed.
Diagnosed medical comorbidities | Overall preoperative functional status | Psychological factors | Other |
Heart disease Bleeding/Clotting Disorder Peripheral vascular disease Prior CVA Lung disease Kidney disease Osteoporosis Diabetes Hypertension Neurological comorbidity Cancer BMI | Totally dependent Partially dependent Independent Difficulty with specific ADLs, iADLs, mobility | Preoperative pain catastrophizing Kinesophobia Confidence Optimism Motivation Self-efficacy Stress Depression Social support Dementia Poor cognition | Substance use/abuse (especially smoking) Chronological age Gender Race Coagulation profile (low platelets, high PTT, high INR) Prealbumin Preoperative education classes Peer support |
Abbreviations: BMI, body mass index; CVA, cerebrovascular accident; iADLs, instrumental activities of daily living; INR, international normalized ratio; PTT, partial thromboplastin time. | |||
Invasiveness of the procedure | Level of surgical skill | Systems factors |
Operative time Osteotomy Pelvic fixation Fusion length Blood loss | Years of practice Volume of complex procedures | Facility volume Designated spine team (anesthesia/nursing) Preoperative steroid use Hospital size |
17.3 Risk Stratification Tools
The American Society of Anesthesiologists (ASA) classification scheme, first introduced in 1941 to evaluate overall health status of patients prior to surgery (▶ Table 17.3), 13,14 has long been used as a risk stratification tool to identify those patients at the highest risk. Key advantages of the ASA classification are ease of use and prevalence, but the main disadvantage is that it focuses only on comorbidities and does not take into account other patient or surgical factors. The ASA has been shown to have a strong correlation with major complication incidence and increased length of stay. 15 The Charlson Comorbidity Index is a similar tool that estimates a patient’s 10-year mortality, is associated with complication incidence, and is occasionally used for risk stratification (▶ Table 17.4). 16
Class | Definition |
1 | No comorbidities (healthy, non-smoking, minimal substance use) |
2 | Mild systemic disease (well-controlled hypertension or diabetes, current smoker) |
3 | Severe systemic disease (poorly controlled hypertension/diabetes/COPD, mild congestive heart failure) |
4 | Severe systemic disease that is a constant threat to life (recent [<3 mo] myocardial infarction, cerebrovascular accident, transient ischemic event, sepsis) |
5 | Moribund patient not expected to survive without the surgery (ruptured aortic aneurysm, massive trauma) |
6 | Brain-dead patient undergoing organ removal for donation |
Abbreviation: COPD, chronic obstructive pulmonary disease. | |
Points given | Comorbidity |
1 | Myocardial infarct, congestive cardiac insufficiency, peripheral vascular disease, dementia, cerebrovascular disease, chronic pulmonary disease, connective tissue disease, diabetes without complications, ulcers, chronic disease of the liver or cirrhosis |
2 | Lymphoma, leukemia, benign tumors, diabetes with complications, moderate or severe renal disease, hemiplegia |
3 | Moderate or severe liver disease |
6 | Malignant tumor, metastatic cancer, AIDS |
17.4 Frailty
In the last 5 years, research has focused on frailty as a potential predictor of poor outcomes following surgery. As a measure of physiologic rather than chronologic age, 17 frailty has been shown to be a better predictor of increased complication rate, longer length of hospital stay, and worse postoperative health-related quality-of-life (HRQoL) scores than chronologic age alone in general surgery. 18,19,20,21 Frailty is a comprehensive overview of patient factors which could potentially contribute to increased surgical risk including comorbidities, mental health, physical health, social support, and functional status. Given the aging population in the United States and worldwide, 22 and the fact that surgeries are now being made available to older patients with more comorbidities, 3 accurate risk stratification including all patient factors is especially critical.
Three recent studies in spine surgery have published an association between frailty and complications; however, most of these studies have utilized the modified frailty index. Frailty indices are based on the concept that frailty can be measured as an accumulation of deficits in all areas of health. The modified frailty index was developed by analyzing the National Surgical Quality Improvement Program (NSQIP) database and identifying 11 recorded variables that corresponded to 16 of the 70 variables in the Canadian Study of Health and Aging Frailty Index. 23,24,25,26 However, when Searle et al tested precision and accuracy of frailty indices created following the recommended rubric, a frailty index was found to be precise and accurate as long as enough (30–40) variables were included in the model, but frailty measurements were unstable and imprecise at lower numbers, especially below 10 variables. 27 In other words, the precise variable composition of the frailty index was found to not impact the calculation of frailty as long as enough variables were included in the model. There is no study comparing accuracy of frailty measurements using the modified frailty index to full frailty indices (those including at least 30–40 variables) or to other frailty calculators such as the frailty phenotype. While the modified frailty index has been shown to be another useful risk stratification tool similar to the ASA, it is not yet established whether this is an accurate measure of frailty. Additionally, these studies were all performed using the NSQIP database. Large national databases rely on current procedural terminology 28 to identify patients by diagnosis which leads to inclusion discrepancies, they only record complications for 30 days postoperatively, and they have been shown to under-report complications compared to surgeon-maintained databases. This leads to significant discrepancies in reporting. 29
The Cervical Deformity Frailty Index (CD-FI), developed by the International Spine Study Group, includes 40 variables and was developed utilizing the validated methodology mentioned earlier. It has been shown to be associated with major complication (▶ Fig. 17.1). 30 The Adult Spinal Deformity Frailty Index (ASD-FI), on which the CD-FI was based, has been more extensively studied and validated in multiple databases with strong associations with both major complication incidence and hospital length of stay. Based on these data, it has been established that frailty is a good risk stratification tool for spine surgery. The main advantage of developing a frailty-based risk stratification tool is that it is a comprehensive evaluation of all preoperative patient factors that affect individual risk of complications, increased length of hospital stay, and other adverse events.
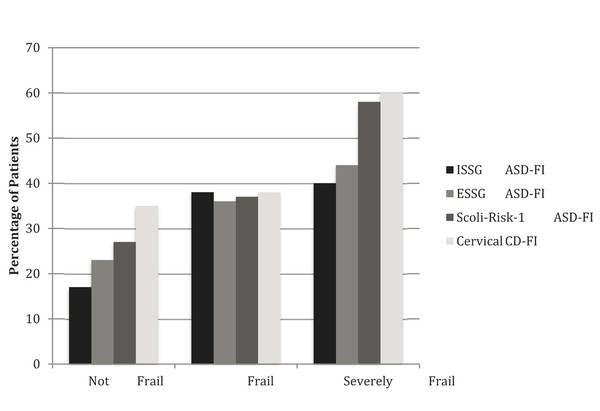
Fig. 17.1 Incidence of major complications.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


