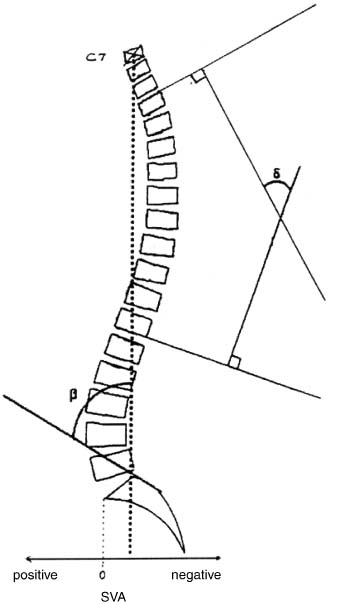
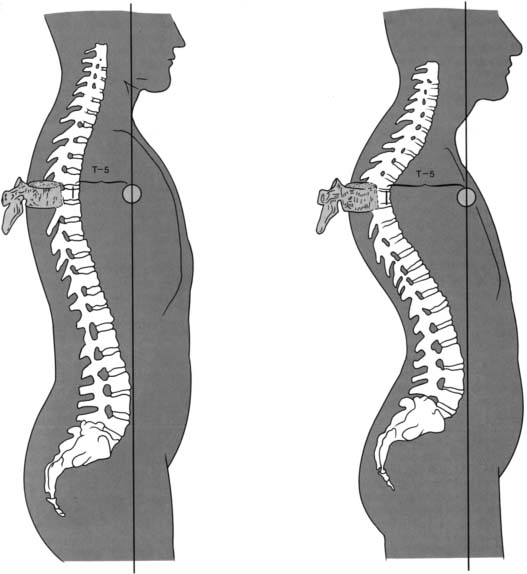
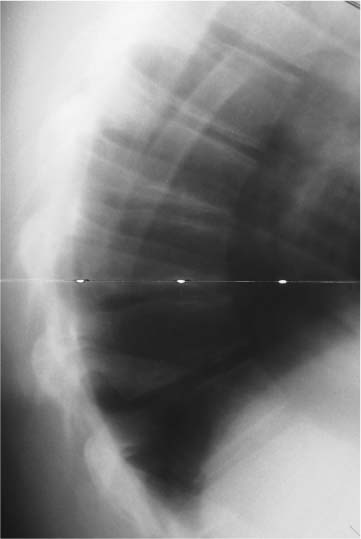
Chapter 19 Kyphotic deformities of the spine are defined as curves with abnormally increased posterior convex angulation. In distinction to scoliotic deformities, kyphotic deformities are more typically confined to one plane. Kyphotic deformities can occur in the cervical spine secondary to fracture (with subsequent loss of anterior vertebral body height), as part of postlaminectomy syndromes, or in a patient with ankylosing spondylitis. Causes of increased thoracic and thoracolumbar kyphosis are many and include changes associated with Scheuermann’s disease, osteoporosis, post-traumatic kyphosis, postinfection kyphosis, tumor, ankylosing spondylitis, paralytic kyphosis, and others. Winter and Hall have classified more than fifteen major groups of kyphosis.1 The most common causes of spinal kyphosis among the pediatric population are Scheuermann’s disease, postural round back, and congenital kyphosis. The fundamental principle in the analysis and treatment of kyphotic deformities is restoration or preservation of sagittal plane balance. Neutral sagittal balance is maintained when a line dropped perpendicular to the horizontal from C7 passes through the posterior aspect of the first sacral vertebra. Kyphotic deformities of the cervical, thoracic, or lumbar spine can result in anterior displacement (positive sagittal balance) of this plumb line with a consequent sensation of forward “tipping-over.” The correction of kyphotic deformities demands re-balancing to restore the C7 plumb line to within 2 to 3 cm of neutral. Although the lumbar spine does not often fall into absolute kyphosis, a loss of lumbar lordosis causes a relative lumbar kyphosis with a subsequent loss of sagittal balance (as the thoracic spine is unable to compensate for the adjacent hypolordosis). Clinically significant sagittal deformities may result in debilitating pain, cosmetic disfigurement, spinal cord dys-function, swallowing difficulties, gastrointestinal difficulties, pelvic organ prolapse, and cardiopulmonary compromise. This chapter will address the etiology, evaluation, and treatment of the most commonly encountered kyphotic deformity among children and young adults: Scheuermann’s kyphosis. Balance of sagittal contour depends on the sagittal vertical axis. This axis falls from the atlanto-occipital articulation through the cervical vertebral bodies and anterior to the thoracic spine. The axis crosses the thoracolumbar junction, travels posterior to the lumbar spine, passes through S1 and then posterior to the second sacral vertebra (Fig. 19–1). Thus, normal thoracic kyphosis combined with cervical and lumbar lordosis maintains the head in a centered, balanced position over the sacrum in the sagittal plane.2 Clinically, if a patient’s standing sagittal balance is neutral, a virtual line drawn vertically should pass from the ear, through the shoulder, greater trochanter, and knee. An increase in thoracic kyphosis in children is easily compensated by residual flexibility demonstrated by the cervical and lumbar spine. In an adult, loss of sagittal balance is often of greater significance secondary to the decreased compensatory flexibility in the mature cervical and lumbar spine, which can result in pain due to compensatory attempts at increasing lordosis. The normal adult spine has four balanced sagittal plane curves. Thoracic and sacral curves are kyphotic and rigid. These curves are considered primary, as the kyphosis is present at birth. The usual kyphotic curve of the thoracic spine extends approximately from T2 to T12. The cervical and lumbar spines are lordotic, and both are considered secondary or compensatory in nature. At birth, the spine is kyphotic throughout its entirety from occiput to coccyx (Fig. 19–2). As an infant gains head control and begins to crawl, the cervical kyphosis reverses into anatomic lordosis. As a child begins to ambulate, the lumbar spine develops a more lordotic contour. These compensatory changes balance the structural thoracic kyphosis to maintain normal sagittal balance. This adult configuration of a column with four alternating curvatures is more tolerant of axial load than a straight perpendicular column. Figure 19–1 Method of measuring various parameters of sagittal spinal alignment. The sagittal vertical axis (SVA) is positive in kyphotic deformities because the C7 plumb line lies anterior to the sacrum. the Cobb angle between two vertebrae. the angle of sacral inclination. From: Gelb DE, Lenke LG, Bridwell KH, et al. An analysis of sagittal spinal alignment in 100 asymptomatic middle and older aged volunteers. Spine 1995;20:1352. Reprinted by permission. Thoracic kyphosis is manifested by the combined effects of the wedge-shaped thoracic vertebral bodies and the wedge-shaped thoracic intervertebral disks. The Scoliosis Research Society (SRS) has accepted the normal range of thoracic kyphosis in the adolescent to be 20 to 40 degrees, and that any degree of kyphosis at the thoracolumbar or lumbar area should be considered abnormal.3 Fon et al. noted the upper limit of kyphosis to be 45 degrees in 316 healthy subjects aged 2 to 27 years, and that the average thoracic kyphosis increases with age, from 20 degrees in childhood, to 25 degrees in adolescents, to 40 degrees in adults.4 The relative rigidity of the thoracic spine permits less flexion, extension, and lateral bending; this is due, in part, to the additional constraint of the costovertebral articulations with the rib cage. Axial rotation is greater in the thoracic spine than lumbar spine, as facilitated by the coronal orientation of the thoracic facets. These facets transition from T10 to T12 to the more sagittal orientation characteristic of the lumbar spine. Figure 19–2 Lateral radiograph of a 2-month-old male infant illustrating the global kyphosis of the spine at birth from occiput to coccyx. The posterior elements of the spine primarily resist tension, and the anterior elements are best adapted to resist compression. Factors that may subsequently contribute to development of a kyphotic deformity include either disruption of the posterior tether (e.g., multilevel laminectomies and facetectomies) or loss of the anterior buttress (e.g., osteoporotic fracture, infection, trauma, or tumor). Kyphosis is the result of a relative lengthening of the posterior column and/or a shortening of the anterior column. Once a kyphotic deformity develops, the patient’s center of gravity is displaced anteri-orly (Fig. 19–3). This results in an increased bending moment acting across the apex of the kyphotic deformity (initiating a cycle of increasing progression until physiologic balance is restored).5 The more angulation at any given point, the greater the susceptibility to additional angulation at a given load.1,6 The development of kyphosis in the skeletally immature patient can result in asymmetric growth as compression tends to inhibit physeal growth anteriorly, and tension forces act to accentuate growth posteriorly. Kyphosis may be associated with malformation of the anterior vertebral body as in the case of Type I congenital kyphosis.7,8 If posterior column growth velocity exceeds that noted anteriorly, a kyphotic deformity will develop.9,10 Iatrogenic disruption of the stabilizing structures posteriorly in the pediatric spine, for instance, after selective dorsal rhizotomy or tumor resection, can lead to rapid progression of a kyphotic deformity.11,12 This may be similarly problematic in adult patients after multi-level cervical laminectomy. Figure 19–3 The line projected in this illustration is parallel to a plumb line drawn through the center of mass of the body. With increased kyphosis, the moment arm between the thoracic vertebral bodies and the center of gravity increases. As the moment arm increases, there is a greater tendency for progressive deformity. Notice the compensatory increase in lumbar lordosis and cervical lordosis, which causes the characteristic head thrust of kyphotic patients. From: An HS, Balderston RA. Juvenile kyphosis. In: Rothman RH, Simeone FA, eds. The Spine, 3rd Ed. Philadelphia: W.B. Saunders Company; 1992:493. Reprinted by permission. The differentiation of a rigid from flexible kyphosis is important. A flexible kyphosis usually spans multiple segments and corrects to within the normal range with active extension, whereas a rigid kyphosis is typically shorter, sharper, and is fixed with active range of motion. Over time, most flexible kyphotic curvatures will become more rigid. This occurs as a combined result of thickening of the anterior longitudinal ligament, loss of disk height, increasing rigidity of the spinal articulations, and loss of viscoelasticity with aging. Lonstein et al. have reported that patients with rigid kyphosis of the thoracic spine are at greater risk of developing neurologic impairment.13 Most cases of neurologic deterioration and kyphosis are the direct result of tethering of the spinal cord over a severe kyphotic deformity.13,14 Attempts to lengthen the kyphotic spinal column and the presence of anterior compression often aggravate the compressive effects on the cord, increase the neurologic risk, and should be avoided. In addition, small disk protrusions in the thoracic spine will act to further injure the already compromised cord leading to more severe spinal cord compression and neurologic injury. Computed tomography (CT) combined with myelography and magnetic resonance imaging (MRI) are useful diagnostic modalities in evaluating neurologic impairment in the setting of spinal kyphotic deformity. In 1921, Scheuermann described a rigid spinal kyphosis affecting the thoracic or thoracolumbar spine that he distinguished from the more correctable postural hunchback.15–17 Sorensen characterized this disease radiographically by the presence of anterior wedging (of five degrees or more) of at least three adjacent vertebrae, end plate irregularity, and the presence of Schmorl’s nodes (Fig. 19–4).18,19 Bradford et al. classified a variant of this process as vertebral body changes without wedging and increased kyphosis.3 Despite these descriptions, making these distinctions can be difficult, and the differentiation of abnormal kyphosis and “pathognomonic” signs of Scheuermann’s disease remain controversial.20 Figure 19–4 This lateral radiograph of an adolescent male demonstrates the typical features of Scheuermann’s kyphosis: anterior vertebral body wedging of three consecutive vertebrae, end plate irregularity, disk space narrowing, and Schmorl’s nodes. Scheuermann’s kyphosis has a reported incidence of 0.4 to 8.3% in the general population with a ratio favoring males to females, though many authors have stated that it occurs with an equal incidence in males and females.21–24 It is the most frequent cause of hyperkyphosis of the thoracic and thoracolumbar spine during adolescence. Scheuermann’s kyphosis is rarely very painful unless a severe deformity is present.25–27 If recognized early, patients with Scheuermann’s kyphosis can often be successfully treated with nonoperative intervention, such as bracing28,29 or exercises. The specific etiology of Scheuermann’s kyphosis remains unclear.30–32 Scheuermann’s initial description included that the condition results from avascular necrosis of the vertebral ring apophyses, which leads to a premature growth arrest with resultant wedging of the anterior portion of the vertebral bodies, and mentioned that it resembled Legg-Calvé-Perthes disease of the hip.15–17 Schmorl believed that there was inherent weakening of the cartilaginous end plate, which lead to herniation of disk material into the vertebral body.18 This was thought to occur during the endochondral ossification process leading to subsequent kyphotic deformity. This theory, however, was weakened by the identification of Schmorl’s nodes in verte-brae outside the kyphotic area and in patients without spinal deformity.22,23 Various mechanical theories have been put forth that implicate the anterior longitudinal ligament and anterior column pressure changes with the spinal deformity developing as dictated by Wolff’s law.33,34 Juvenile osteoporosis may also play a role in progressive kyphosis.35–37 Still others have demonstrated abnormal cartilage matrix and decreased expression of various glycoproteins in the affected end plates.38 What is still unclear in the mechanical theory is whether the end-plate changes seen histologically predispose the verte-brae to kyphosis or are secondary.7 Scheuermann’s disease has been associated with endocrine abnormalities, inflammatory diseases, and neuromuscular disorders.5,21,39,40 The etiology may lie in genetic factors. Genetic theories have varied from familial predilection to autosomal dominant inheritance patterns41 with high degrees of penetrance but variable expression.30 There have been three case reports of classic Scheuermann’s disease in monozygotic male twins, which supports the genetic theory.42,43 Other investigators, such as Ascani22 and Skogland,31 have noted a mean height in affected patients 2.5 standard deviations above normal subjects and increased levels of growth hormone. Scheuermann’s kyphosis is usually detected at puberty. It is commonly ignored or dismissed by parents or teachers as poor posture, which often leads to a delay in diagnosis. It is rare in patients younger than age 10 years, with the typical presentation in the late juvenile period, and the more severe form commonly appearing between the ages of 12 and 16 years.20 The primary distinguishing feature between postural kyphosis and Scheuermann’s kyphosis is the rigidity of the Scheuermann curvature. Trunk extension will produce deformity correction in those with postural kyphosis, whereas minimal to no such correction will be achieved in the patient with Scheuermann’s disease. In addition, patients with Scheuermann’s disease may be further affected by contracture of their pectoral muscles, hip flexors, and hamstrings. The patient with Scheuermann’s disease typically has a very well demarcated angular thoracic or thoracolumbar kyphosis, accentuated by forward bending, as well as a compensatory hyperlordosis of the cervical and lumbar spine. The compensatory changes produce the characteristic head and neck thrust typically associated with Scheuermann’s kyphosis. Loder reported that the flexible cervical and lumbar spine is linked by the intermediate rigid thoracic segment, and as the thoracic spine becomes more kyphotic, lordosis of the cervical spine increases as a patient struggles to maintain a forward visual gaze.44 Clinical manifestations of severe disease include pain, physical disability, decreased range of motion and back strength, restrictive lung disease, hamstring tightness, scoliosis, spondylolisthesis, disk degeneration, and decreased participation in athletic activities or labor-type occupations.3,22,24,32,45–51 Adolescents with Scheuermann’s kyphosis primarily have self-image or postural concerns but will often report neck pain, back pain, and fatigue; pain is more commonly the chief complaint of adults. The typical pain is above or below the apex of the deformity, in the paraspinal area, and may be activity related. Adult patients may also have lumbar pain, which is related to their compensatory hyper-lordosis, subsequent disk degeneration, and facet arthrosis. If an adult’s deformity is less than 60 degrees, a patient with Scheuermann’s kyphosis may be expected to have little chance of significant back discomfort beyond that noted in the general population.33 A long-term study by Murray et al. of adult Scheuermann patients with mean 32-year follow-up and age-matched controls showed that although they had more intense back pain, decreased trunk motion and strength, and tended to have less physically demanding occupations, there were no significant differences for days missed from work, self-esteem, social limitations, use of medications, or preoccupation with their physical appearance.24 However, in a subsequent article by Lowe and Kasten,52 adults with severe kyphotic deformities (>75 degrees) had severe thoracic pain secondary to degenerative spondylolysis and can have significant limitations, and the authors allude to magnitude of deformity as a cause of pain that alters lifestyle, although this relationship lacks Level I scientific evidence. Neurologic symptoms are rare in adolescents with Scheuermann’s disease. Paraparesis has been reported in rare cases with associated herniated thoracic disks, spinal stenosis, dural cysts, or extremely severe kyphotic deformity with tenting of the spinal cord over the apex of the deformity.14,27,53,54 One report studying patients with Scheuermann’s kyphosis noted that disk herniation resulted in neurologic symptoms in only 1% of the patients studied.45 One theory proposes that vascular compromise of the artery of Adamkiewicz may be responsible for the onset of acute paraparesis in affected patients.33 Selective spinal arteriography or magnetic resonance angiography is suggested as a useful diagnostic adjunct in these cases. Vertebral compression fracture may also precipitate acute paraparesis in these patients.55 In summary, patients with Scheuermann’s kyphosis may be neurologically intact, though with little reserve, leaving them vulnerable to acute neurologic deterioration from typically benign lesions or iatrogenic disruption of spinal cord blood flow.56 The normal range of thoracic kyphosis is generally considered to be between 20 and 40 degrees using the Cobb method on the erect lateral radiograph.3,57 Scheuermann’s disease is best identified from evaluation of a standing lateral long-cassette (36 in.) roentgenogram displaying narrowed intervertebral disk spaces, end-plate irregularities, and Schmorl’s nodes.47 The radiographic criteria for diagnosis, set forth by Sorensen, includes the presence of greater than 5 degrees of anterior wedging of at least three adjacent vertebrae at the apex of the kyphotic deformity (Fig. 19–4).19
Scheuermann’s Kyphosis
♦ Kyphotic Deformities
Normal Sagittal Alignment
Anatomy
Pathomechanics of Kyphotic Spinal Deformities
♦ Scheuermann’s Kyphosis
Etiology and Pathogenesis
Clinical Findings and Natural History
Radiographic Findings
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree