Selected Stroke Syndromes
CASE
A 67-year-old hypertensive male smoker comes in with sudden onset of complete paralysis of the right side of the body. His right face is weak, and his speech is slurred. Despite this, he is completely aware of his surroundings and has normal memory and affect. His sensory exam is normal. His right toe is upgoing.
LACUNAR INFARCTION
Lacunes are vascular lesions in the brain commonly seen in patients with hypertension or diabetes. They are small areas of thrombotic infarction that become pea-sized holes pathologically. It is important to recognize lacunar strokes, because they represent small-vessel disease and generally require limited investigation. Control of hypertension, hyperglycemia, hyperlipidemia, cessation of smoking, and use of antiplatelet agents are likely to improve outcome and prevent future strokes.
Look for these characteristic syndromes:
Pure motor hemiplegia, in which there is a lesion in the pons or internal capsule. Paralysis of face, arm, and leg without sensory loss. A right hemiplegia of lacunar origin that has no accompanying aphasia. With a left hemiplegia, there are no parietal lobe findings.
Pure sensory stroke, in which there is a lesion most often in the thalamus. Contralateral sensory loss in the face, arm, and leg, with no hemiplegia or other signs. Thalamic sensory loss may cause a loss of pin sensation affecting one side that splits the midline.
Clumsy-hand dysarthria, showing a lesion in the pons or internal capsule. Slurred speech with clumsiness and mild weakness of one arm.
Crural (leg) paresis and ataxia (ataxic hemiparesis) with a lesion in the pons, or internal capsule. Ataxia and weakness of one leg.
INTRACEREBRAL HEMORRHAGE
Computed tomography (CT) scan is diagnostic in acute intracerebral hemorrhage.
Note: CT may miss hemorrhage in the brainstem and cerebellum because of bony artifacts. If the CT is “normal” and a clinical suspicion of posterior circulation hemorrhage remains, a magnetic resonance imaging scan should be obtained.
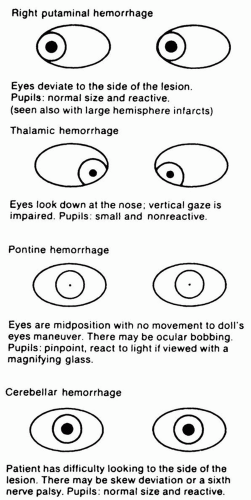
Cerebellar Hemorrhage
Cerebellar hemorrhage is important to diagnose because it can lead to rapid death via brainstem compression; treatment is surgical evacuation of the clot. Headache, vomiting, and inability to walk with normal lower-extremity strength are cardinal features. Strength and sensation are usually normal (unless brainstem compression occurs). The patient may have trouble looking to the side of the lesion (gaze paresis). Nystagmus and limb ataxia may not be present. Ipsilateral facial weakness may be present. Cerebellar infarction with subsequent swelling may mimic cerebellar hemorrhage, and require surgical treatment.
Putaminal
Most intracerebral hemorrhages occur in the putamen. Look for the following:
Striking eye deviation to side of hemorrhage and away from the hemiplegia (Fig. 16.1).
Headache.
Homonymous visual field deficit contralateral to the lesion.
Cortical deficits, which develop as the hemorrhage progresses.
Thalamic
May or may not have hemiplegia. Has eyes that look down at the nose, with small and nonreactive pupils (Fig. 16.1). Has marked contralateral sensory loss.
PONTINE HEMORRHAGE
The patient is comatose with small pinpoint pupils (Fig. 16.1). Pupils react to bright light when viewed with a magnifying glass. There is quadriparesis, with upgoing toes. Patient has no horizontal
extraocular movements with passive head turning or use of icewater calorics. Ocular bobbing may occur (rapid downward eye deflection with slow upward drift). The patient may be locked-in (conscious, but unable to move to show consciousness). He or she may retain the ability to look up and down.
extraocular movements with passive head turning or use of icewater calorics. Ocular bobbing may occur (rapid downward eye deflection with slow upward drift). The patient may be locked-in (conscious, but unable to move to show consciousness). He or she may retain the ability to look up and down.
Note: The most common causes of intracerebral hemorrhage are hypertension and trauma. Other causes include blood dyscrasias, side effects of anticoagulant therapy, drug abuse (cocaine), amyloid angiopathy, brain tumors, and cryptic arteriovenous malformations (AVMs).
SUBARACHNOID HEMORRHAGE
Subarachnoid hemorrhage (SAH) classically presents with the sudden onset of severe headache during activity, altered level of consciousness; at times, coma, nuchal rigidity, and bloody cerebrospinal fluid. There may be autonomic disturbances such as vomiting, fever, and electrocardiogram changes. Hemorrhage into the brain substance appears as an increased density on CT scan; arterial spasm generally produces no changes on CT scan. Delayed deterioration in patients with SAH may be caused by hydrocephalus, seizures, cerebral edema, vasospasm, or rebleeding.
The most common locations for aneurysms are at various arterial junction points around the circle of Willis at the base of the brain:
Posterior communicating artery: may have associated third nerve palsy.
Anterior communicating artery: mutism and leg weakness may occur.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree