♦ Preoperative
Patient Evaluation
- Complete history and physical with close attention to lower extremity spasticity and strength for each nerve root. Assessment of tone, range of motion for each joint, and postural stability is essential. Physical and occupational therapists are essential to the evaluation.
- Neurologic evaluation: screening clinical criteria for appropriateness of therapy; can assist with determining extent and anatomy of spasticity
- Physiotherapy evaluation: assist with screening assessment for spasticity; establish goals for post-rhizotomy therapy
Review Imaging
- Complete neuraxis imaging (computed tomography [CT], magnetic resonance imaging [MRI]) evaluation for structural causes of spasticity and any abnormal anatomy
- Baseline pelvis and spine x-rays to assess the presence of hip dislocation and scoliosis
Special Equipment
- Microscope with bridge attachment
- Electrophysiologic monitoring (electromyogram [EMG]/nerve conduction studies) with intraoperative stimulating devices (i.e., rhizotomy probes)
- Fluoroscopy of intraoperative x-ray for localization
- Intraoperative ultrasound device
- Silastic sheet (1 × 3 cm)
Operating Room Set-up
- Patient prone on the operating table with anesthesia positioned at the head end
- General anesthesia
♦ Intraoperative
Positioning
- After induction of general anesthesia, the patient is placed prone with chest and hip rolls; close attention is given to the adequate protection of pressure points through padding.
Electrophysiologic Monitoring
- Bilateral lower extremity monitoring is performed with percutaneous electrodes placed into representative muscles for each nerve root from L1 to S2. Anal sphincter electrodes are also placed to permit the assessment of sacral rootlet contribution toward sphincter function.
Laminectomy
- The L1 spinous process is identified with lateral radiograph or fluoroscopy.
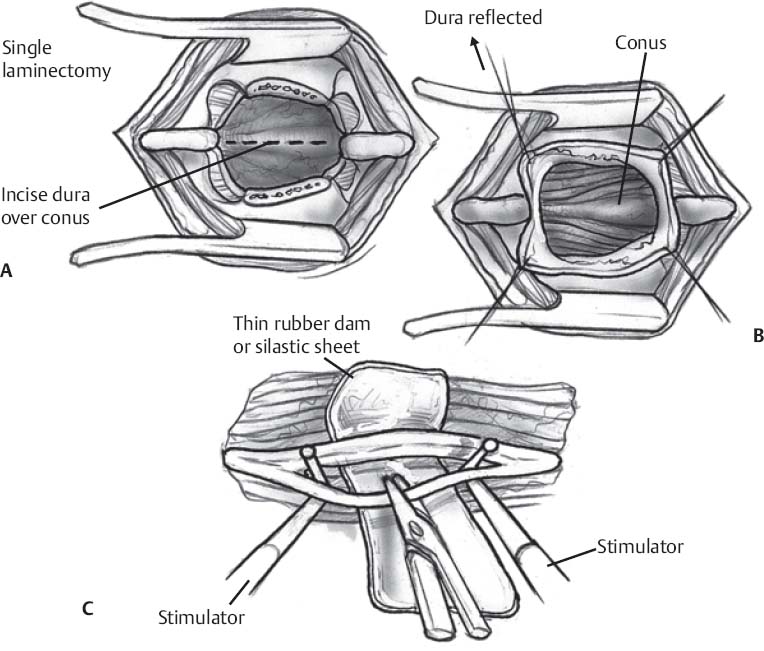
- Surgery involves a small (~2 to 3 cm) incision in the lower back, followed by a L1 laminectomy (Fig. 168.1A)
- Intraoperative ultrasound is then used to identify the conus medullaris before the dura is opened.
- Occasionally, the laminectomy needs to be extended by half of a level in either direction for adequate visualization of the conus and cauda.
- The dura is then opened and the operating microscope is used (Fig. 168.1B)
Identification of Anatomical Landmarks
- After opening the dura, the following structures are identified: the conus medullaris, the L1 nerve root, and the dorsal nerve roots from L2 to S1. The L1 nerve root is the most lateral and can be followed out of the L1 foramen. The L1 root can be separated into its dorsal and ventral components, which can help facilitate developing the plane between the dorsal and ventral roots of L2 to S1.
- Once the plane between the dorsal and ventral roots is established, the S1 dorsal nerve root can be identified as it is the most medial of the large dorsal roots and usually covers the conus. Lifting S1 will reveal the much smaller distal sacral nerve roots. L2–L5 dorsal roots can be identified moving from lateral to medial.
- The dorsal roots from L2–S1 are then wrapped in a silastic sheet to separate them from the conus, the distal roots, the ventral roots, and the contralateral nerve roots.
Electrical Stimulation of Dorsal Rootlets
- Each dorsal root bundle is separately stimulated with rhizotomy probes.
- Because L1 is the only nerve root where both the motor and ventral roots can be absolutely identified as they exit the L1 foramen, motor and sensory thresholds for electrophysiological monitoring are established at this level.
< div class='tao-gold-member'>Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree