Introduction
Since sleep and epilepsy are common bedfellows, it stands to reason that sleep disorders may mimic, cause, or even be triggered by epileptic phenomena, and vice versa. It is known that, in some individuals, sleep promotes seizures, as does sleep deprivation.25,86 Conversely, seizure disorders can affect the wake–sleep cycle.114 As discussed in Chapter 188, in most cases, epilepsy is highly state-dependent: Non–rapid eye movement (NRM) sleep promotes seizures, while rapid eye movement (REM) sleep is a relatively antiepileptic state.132,134 This fact reflects the dramatic reorganization of the entire central nervous system (CNS) as it moves across the three states of being: Wakefulness, NREM sleep, and REM sleep.
There are certain predisposing factors in NREM sleep that facilitate epileptic discharges. There may be a relationship between sleep spindles and spike-and-wave bursts in human epilepsy.57 There may also be a relationship between the cyclic alternating pattern (CAP) of “fluctuating cortical excitability” with both sleep-related epilepsy and a number of other sleep disorders.136,145
In simpler times, it was felt that sleep was a unitary phenomenon—the passive absence of wakefulness. In the first half of this century, it was discovered that sleep was an active state. Then, in 1953, it was discovered that sleep was actually composed of two completely different states of being: NREM and REM sleep. We, as humans, as most mammals, spend our lives in three completely different states of being: Wakefulness, REM sleep, and NREM sleep. Each of these states has its unique neuroanatomic, neurophysiologic, neurochemical, and neuropharmacologic correlates and substrates.55,135 It took centuries to determine that sleep is actually a bimodal process because (a) superficially and from a distance, REM and NREM sleep look similar, and (b) these two states cycle back to back, giving the illusion of homogeneity.
There are five primary determinants of the quality of nighttime sleep and of daytime alertness117:
Homeostatic (duration of prior wakefulness)
Circadian (biologic clock influence)
Age
Drugs
CNS pathology
These factors determine the overall wake–sleep pattern, upon which the parasomnias are superimposed. These same factors also play an integral role in epileptic events.
With the advent of neurophysiologic monitoring techniques, it has become obvious that state determination is a very complex and dynamic phenomenon, involving multiple neural networks, neurotransmitters, neuropeptides, neurohormones, and myriad sleep-promoting substances. Given these complexities, it has become clear that the determination of state may be inexact, with components of two or all three states occurring simultaneously or oscillating rapidly. This concept of state dissociation in animals and humans has been extensively reviewed.73,74,76
Parasomnia is the term given to undesirable motor, verbal, or experiential phenomena that occur during the sleep period. It is these sleep disorders that are most commonly confused with epileptic phenomena. Parasomnias may be conveniently categorized as primary (disorders of sleep states per se) and secondary (disorders of other organ systems manifesting themselves during sleep). The primary sleep parasomnias can be classified according to the sleep state of origin: REM sleep, NREM sleep, or miscellaneous (those not respecting sleep state). The secondary sleep parasomnias can be further classified by the organ system involved.72 Many parasomnias are manifestations of state dissociation. These mixed states result in fascinating and perplexing clinical phenomena that may easily be confused with epileptic events, and conversely, these sleep disorders may be perfectly imitated by epileptic events. Furthermore, other primary sleep disorders may trigger seizures, and, conversely, seizures may trigger abnormal sleep phenomena. In addition to the parasomnias, there is impressive overlap among epileptic, sleep, and psychiatric phenomena (Table 1).
Clinical Description
The following is a listing of various areas of overlap and confusion between sleep disorders and seizures ranging from normal events to hypersomnia, insomnia, and parasomnias.
Normal Sleep Phenomena
Sleep Starts
Sleep starts (hypnic jerks) are experienced by many normal individuals during the transition from wake to sleep. The most common is the motor sleep start, a sudden jerk of all or part of the body, occasionally awakening the victim or bed partner.106 Variations on this theme include the visual (flashes of light, fragmentary visual hallucinations), auditory (loud bangs, snapping noises), or somesthetic (pain, floating, something flowing through the body) sleep start, occurring without the body jerk.20,42,70,101,122 Sleep starts represent a normal (although not understood) physiologic event, and should not be confused with seizures or other neurologic conditions. It is likely that the “exploding head syndrome,” characterized by a sensation of a loud sound like an explosion or a sensation of “bursting” of the head, and “explosive tinnitus” are variants of sensory sleep starts.22,108,121,144,152 Similar phenomena may represent the sole manifestation of a seizure.37
Table 1 Overlap among epileptic, sleep, and psychiatric phenomena | ||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||
Nightmares
Nightmares are frightening dreams that usually awaken the sleeper from REM sleep. Unlike disorders of arousal (see below), they are not usually associated with prominent motor or vocal behavior or autonomic excitation, and the arousal
results in immediate full wakefulness, with memory for the dream sequence of events that caused the awakening.72 Seizures manifest as recurrent dreams, nightmares, or disorders of arousal such as sleepwalking, and sleep terrors have been well described in both adults and children. The diagnosis of seizure-related dreams and nightmares may be overlooked, as the symptom is misinterpreted as a primary sleep phenomenon.12,28,29,39,138 Autosomal dominant frontal epilepsy may also present as recurrent “nightmares.”124,125
results in immediate full wakefulness, with memory for the dream sequence of events that caused the awakening.72 Seizures manifest as recurrent dreams, nightmares, or disorders of arousal such as sleepwalking, and sleep terrors have been well described in both adults and children. The diagnosis of seizure-related dreams and nightmares may be overlooked, as the symptom is misinterpreted as a primary sleep phenomenon.12,28,29,39,138 Autosomal dominant frontal epilepsy may also present as recurrent “nightmares.”124,125
Hypersomnia
Epilepsy
Nocturnal seizures may cause severe sleep fragmentation, if the sole manifestation is arousal (which may not be appreciated by the patient). The end result is excessive daytime sleepiness.130 Some patients with seizures are hypersomnolent during the day—even after antiepileptic medication discontinuation. Seizure-free preadolescent children with epilepsy are sleepier than healthy controls. In one study, there was no difference in objective sleepiness in children with epilepsy on or off medication, suggesting that use of antiepileptic drugs does not necessarily result in daytime sleepiness.103 The complaint of daytime sleepiness in patients with epilepsy may be due to a number of different conditions (sleep deprivation, sleep-related seizure-induced arousals, coexisting sleep disorders such as sleep apnea or narcolepsy, or medication effect). Thoughtful evaluation of this complaint is encouraged; hypersomnia in patients with epilepsy should not summarily be attributed to the effect of antiepileptic medications.7,35
Narcolepsy
Narcolepsy is a genetically determined disorder characterized by excessive daytime sleepiness, cataplexy (the sudden loss of muscle tone triggered by emotionally laden events), sleep paralysis, hypnagogic hallucinations, and automatic behavior during which prolonged, complex activities may be performed without conscious awareness or recall.1 The “spell-like” nature of some sleep attacks, cataplexy, and sleep paralysis may be mistaken for seizures. Conversely, atonic or inhibitory seizures may mimic cataplexy,3,41,45,56,66,139 and the periods of
automatic behavior are often misdiagnosed as partial complex seizures, postictal confusion, or poriomania.32,60,80 The incomplete and waxing and waning nature of cataplexy can imitate tonic–clonic seizure activity.
automatic behavior are often misdiagnosed as partial complex seizures, postictal confusion, or poriomania.32,60,80 The incomplete and waxing and waning nature of cataplexy can imitate tonic–clonic seizure activity.
Periodic Hypersomnia (Kleine-Levin Syndrome)
The Kleine-Levin syndrome is a poorly understood condition characterized by recurrent periods of hypersomnia. The often-cited association with adolescent males and unusual behaviors such as hypersexuality and megaphagia has been overrated.6,137 Menstruation-related periodic hypersomnia may represent a variant of the Kleine-Levin syndrome.11 Similar recurrent episodes of hypersomnia may be caused by “ictal sleep” lasting 1 to 3 days at 10- to 60-day intervals.94,156
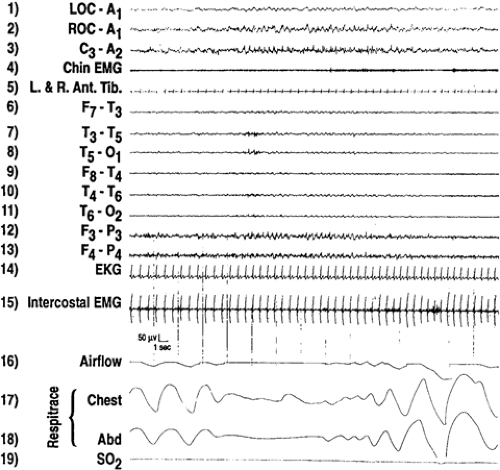
Sleep-disordered Breathing
There is an interesting and important relationship between sleep-disordered breathing and seizures. Nocturnal seizures, probably triggered by periods of hypoxemia, may be the presenting symptom in some individuals with obstructive sleep apnea or sleep-related hypoventilation.62 Furthermore, sleep apnea may exacerbate seizures in patients with epilepsy due to sleep disruption, sleep deprivation, hypoxemia, or decreased cerebral blood flow. As would be expected, patients who have both epilepsy and sleep-disordered breathing may have better control of their seizures following effective treatment for the sleep-disordered breathing.79,148 Not all “spells” associated with sleep apnea are epileptic manifestations. They may be due to episodes of cerebral anoxia.16
Insomnia
Paroxysmal, otherwise unexplained awakenings may be the sole manifestation of nocturnal seizures, and will result in the complaint of insomnia.8,30,31,97,110 Some patients with occasional paroxysmal periodic motor attacks during sleep have very frequent (every 20 to 60 seconds) subclinical arousals resulting in severe sleep fragmentation.130 These paroxysmal arousals may be due to deep epileptic foci.92 The arousal preceding nocturnal seizures may be the initial manifestation of the seizure.78 Animal studies support the concept of frequent arousals as the manifestation of seizures.133 This may explain the fact that some patients with epilepsy report frequent, otherwise unexplained, nocturnal awakenings and excessive daytime sleepiness.50
Parasomnias
Disorders of Arousal
Disorders of arousal are the most common and impressive of the NREM sleep parasomnias, and may readily be confused with epileptic phenomena. These occur on a continuum ranging from confusional arousals to sleepwalking to sleep terrors. The disorders of arousal share common features: A positive family history, suggesting a genetic component; they tend to arise from slow-wave sleep (stages 3 and 4 of NREM sleep), therefore usually occurring in the first third of the sleep cycle (and rarely during naps); and they are common in childhood, usually decreasing in frequency with increasing age.77 Although they most frequently occur during slow-wave sleep, they may occur during any stage of NREM sleep, and may occur late in the sleep period. Contrary to popular opinion, the
appearance or persistence of these events into adulthood is usually not associated with significant psychiatric disease. Specialized forms of arousal disorders may manifest as sleep-related eating or sleep-related sexual activity.126,131
appearance or persistence of these events into adulthood is usually not associated with significant psychiatric disease. Specialized forms of arousal disorders may manifest as sleep-related eating or sleep-related sexual activity.126,131
The disorders of arousal may be difficult to differentiate from nocturnal seizures, and vice versa.68,109 Preservation of consciousness during seizures may lead to confusion with disorders of arousal or psychogenic conditions.26 Crying (dacrystic) or laughing (gelastic) seizures may be misinterpreted as confusional arousals or sleep terrors.5,69 Both disorders of arousal and seizures may be menstrual related.52,96,127
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree