Specific Injury Types
61.1.1 Craniovertebral Junction Injuries
Atlanto-occipital Dislocation
Injury Description
Atlanto-occipital dislocation (AOD) involves traumatic separation of the occiput from C1 and is an injury primarily of the pediatric population, occurring more than twice as frequently in children as in adults (▶ Fig. 61.1 a–d). It is one of the most common fatal cervical spine injuries, resulting from high-energy acceleration–deceleration impacts, most often during motor vehicle accidents involving pedestrians. AOD is primarily a ligamentous injury; it is caused by either hyperextension or, less commonly, hyperflexion in combination with extreme rotation, lateral flexion, and distraction, which results in rupture of the O–C1 joint capsules and disruption of either or both of the tectorial membrane and alar ligaments.1–7 There are usually no fractures, although in older children and adolescents, stronger ligaments may result in avulsion fractures at the ligamentous attachments to the occipital condyles or the base of the clivus, as opposed to frank ligamentous rupture.3,4,6 There is often additional injury to the suboccipital and posterior cervical musculature and prevertebral intrafascial hemorrhage.
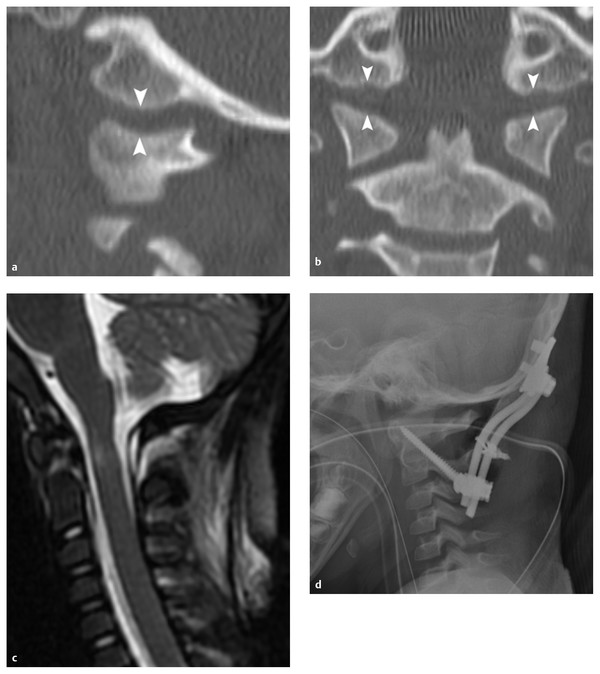
Fig. 61.1 Atlanto-occipital dislocation. (a) Sagittal and (b) coronal reconstructed computed tomographic scans of the occipital condyle–C1 joint from a 4-year-old girl demonstrating an abnormally large occipital condyle–C1 joint interval (white arrowheads). (c) Sagittal fat-suppressed T2-weighted magnetic resonance image demonstrating associated spinal cord edema at the cervicomedullary junction and significant ligamentous injury. (d) Postoperative lateral radiograph from this patient demonstrating occipital condyle–C2 posterior fusion incorporating bilateral C1-2 transarticular screws.
Clinical Presentation
Historically, AOD has been associated with a high incidence of at-the-scene mortality; however, increased resuscitation skills in the lay public, improved emergency medical service response times, better initial cervical spine immobilization, and more prompt diagnosis have led to an increasing number of survivors.8–13 Children with AOD generally present with cardiopulmonary failure and severe neurologic deficits resulting from supratentorial, brainstem, cranial nerve, and spinal cord injuries.14–18 Coma or severely altered mental status is common. Motor deficits in AOD vary depending on the level and degree of injury and range from subtle hemiparesis to flaccid quadriplegia. It is important to note that most survivors of AOD, including those with a severe initial presentation, such as flaccid quadriplegia, have incomplete injuries and ultimately may have a good outcome.
Radiographic Diagnosis
Radiographic findings on plain films may be subtle, and AOD should be suspected in any child involved in high-speed trauma, especially one presenting with cardiopulmonary instability and associated facial injuries. Because early diagnosis is paramount to mitigate additional neurologic injury, all patients with suspected AOD should undergo prompt initial radiographic screening with a lateral cervical spine plain film.
Historically, AOD has been classified according to the system developed by Traynelis et al in 1986, which defined three types based on the direction of displacement of the occiput with respect to the atlas: type I, with anterior dislocation; type II, with longitudinal dislocation; and type III, with posterior dislocation.19 The majority of children with traumatic AOD have a type I injury. Recently, use of the Traynelis classification system has largely been supplanted by use of the occipital condyle–C1 (O–C1) joint interval (CCI) of Pang et al for the diagnosis and classification of AOD (▶ Fig. 61.1a,b).20,21 A CCI of more than 4 mm in either the sagittal or coronal plane for one or both O–C1 joints is considered a positive finding. Alternatively, a Powers ratio of greater than 1 is always abnormal and is indicative of Traynelis type I AOD. A basion–axial interval of more than +12 mm is indicative of type I AOD, and a value of less than –4 mm represents type III AOD. The dens–basion (DB) distance of Wholey et al may also be used to assess for AOD, and values greater than 14 mm should be considered diagnostic.22
Any patient with suspected AOD based on clinical presentation, compatible mechanism, or plain radiographic findings should undergo thin-cut computed tomography (CT) from the occiput to at least C2 with sagittal and coronal reconstructions. CT reconstructions through the O–C1 joint can more clearly demonstrate abnormal separation or translation of the articulation than plain films. However, it should be noted that if AOD is reduced at presentation, bony abnormalities may not be apparent on either plain films or CT scans.
AOD is commonly associated with other radiographic abnormalities on both CT and magnetic resonance (MR) imaging, including cervicomedullary subarachnoid hemorrhage, spinal cord injury (SCI) or compression, and traumatic brain injury (i.e., cerebral edema, contusions, traumatic subarachnoid hemorrhage, intraventricular hemorrhage, or diffuse axonal injury). MR imaging is useful when plain radiographs or CT is not diagnostic and may demonstrate disruption of the tectorial membrane or alar ligaments and hemorrhage or edema in the retropharyngeal and posterior soft tissues, as well as brainstem and spinal cord damage or compression (▶ Fig. 61.1c).
Treatment
The initial treatment for AOD begins in the field with aggressive cardiopulmonary resuscitation as needed. During resuscitation efforts, the spine and head are temporarily immobilized in a neutral position, as discussed in Chapter ▶ 60 in the section on initial evaluation and treatment. In young children with a disproportionately large head-to-torso ratio, elevation of the thorax with padding or blankets or the use of a specialized back board with a recess for the occiput prevents undue flexion of the neck and anterior dislocation. Immobilization with a rigid cervical collar should be maintained pending more definitive treatment. If a properly fitting cervical collar is not available, the head of a young child may be temporarily immobilized by taping to the back board.
Following radiographic confirmation of AOD, if there is a reasonable chance of survival and meaningful neurologic recovery from associated supratentorial brain injuries, the child should undergo prompt external immobilization. AOD is exceedingly unstable, and the use of distracting cervical traction is contraindicated because it may result in additional cervicomedullary injury.23,24 Evolving brainstem findings following immobilization are suggestive of vertebral artery dissection.
Some authors have reported successful treatment and fibrous fusion in children with AOD by using only external immobilization in a halo vest.23,25–27 Others, however, have reported worsening neurologic deficits when internal stabilization was not pursued.9 Given that AOD is extremely unstable and there is a very real risk for delayed neurologic injury with inadequate immobilization, occipitocervical instrumentation and fusion should be strongly considered once the patient is medically stable and any associated brainstem swelling has begun to resolve, typically 5 to 7 days after injury. Because C1–2 instability cannot be independently elicited in the presence of AOD, longitudinal C1–2 instability should be assumed, and therefore internal fixation and fusion from the occiput to C2 is typically performed (▶ Fig. 61.1d).
Long-term stability is predicated on achieving bony arthrodesis across a wide area of the occipital bone and the posterior arches of both C1 and C2. Autologous structural bone graft, such as rib, iliac crest, or split calvarial bone, is the gold standard and is most commonly used. Given the high incidence of AOD in infants and very young children, the posterior elements may not be robust enough to accept internal fixation, although rigid internal fixation from the occiput to C2 has been reported in children as young as 18 months. If rigid internal fixation is not possible, then sublaminar fixation techniques with postoperative halo immobilization may be required to achieve adequate fusion rates.
Jefferson (C1) Fracture
Injury Description
First described by Sir Geoffrey Jefferson in 1920, fractures of the atlas (C1) result when axial compression is transmitted from the occipital condyles to the lateral masses of C1 (▶ Fig. 61.2).28 Jefferson fractures are rare in children because the atlas is not completely ossified in this age group and the C1 ring contains a large amount of cartilage, allowing the dissipation of excessive axial loads.29 The most common mechanisms of injury are falls and motor vehicle accidents. The posterior and neurocentral synchondroses of the atlas fuse at around 3 and 7 years of age, respectively.30 In children, it is important to distinguish a Jefferson fracture from an unfused synchondrosis, which is generally not of any clinical significance.31 Alternatively, C1 fractures may occur through the synchondrosis and can be missed on plain radiographs.30 Atlas fractures may be accompanied by disruption of the transverse ligament, resulting in atlantoaxial instability. There is a high incidence of associated C2 fracture.
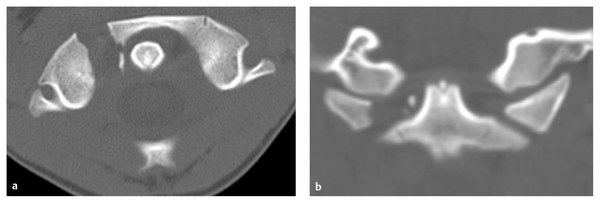
Fig. 61.2 Jefferson fracture. (a) Axial and (b) coronal computed tomographic (CT) scans demonstrating fracture through the right anterior arch and lateral mass of C1. If the sum of the total lateral overhang of the C1 lateral masses on C2 is ≥ 7 mm on odontoid view radiographs or coronal CT, then disruption of the transverse ligament should be suspected (the “rule of Spence”).119
Clinical Presentation
The classic presentation of a child with an atlas fracture includes neck pain, muscle spasm, decreased range of motion, and head tilt; the majority of patients have at least three of these four symptoms.29 Neurologic deficit is rare because of the capacious size of the spinal canal at this level and the fact that pathologic axial loads result in widening of the C1 ring as it fractures.
Radiographic Diagnosis
The majority of atlas fractures can be diagnosed with plain radiographs or CT scans. CT has led to an increased recognition of these fractures children (▶ Fig. 61.2a,b).32 On odontoid view radiographs, transverse ligament disruption is suggested if the sum of the total overhang of the C1 lateral masses on C2 is 7 mm or more (the “rule of Spence”). MR imaging can be used to further assess the integrity of the transverse ligament, if needed.
Treatment
The treatment of isolated Jefferson fractures with an intact transverse ligament is generally external immobilization in a rigid cervical collar, Minerva brace, or halo. If there is transverse ligament rupture and atlantoaxial instability, treatment should involve either halo immobilization or, rarely, C1–2 internal stabilization and fusion.
Translational Atlantoaxial Subluxation
Injury Description
Traumatic translational atlantoaxial (C1–2) subluxation is an extremely rare injury in children, often occurring as a result of a violent mechanism. There are few survivors (▶ Fig. 61.3, ▶ Fig. 61.4).33–36 The majority of affected children are 0 to 9 years old and often have purely ligamentous injury without fractures. In this age group, the dentocentral synchondrosis has less strength than the transverse ligament; therefore, epiphysiolysis of the odontoid process occurs more readily than transverse ligament rupture and translational C1–2 subluxation, partially accounting for the low incidence of this injury in children.36 As such, traumatic translational atlantoaxial subluxation generally occurs under very specific circumstances and in the presence of predisposing factors. It is thought to result from disruption of the transverse ligament, allowing compression of the spinal cord between the odontoid process and posterior C1 arch. However, some autopsy studies have disputed this, reporting that injury to the C1–2 facet joints and capsules is more common than transverse ligament rupture in these patients.34 A flexion mechanism is implicated in most cases of traumatic translational C1–2 subluxation37 however, rare instances of posterior subluxation secondary to hyperextension or atlantoaxial distraction have been noted, even in the presence of a normal odontoid process and C1 ring.38 Nontraumatic translational atlantoaxial subluxation is associated with developmental disorders that result in either laxity of the transverse ligament or odontoid hypoplasia (i.e., Down syndrome, Klippel-Feil syndrome, juvenile rheumatoid arthritis, Morquio syndrome, skeletal dysplasias).
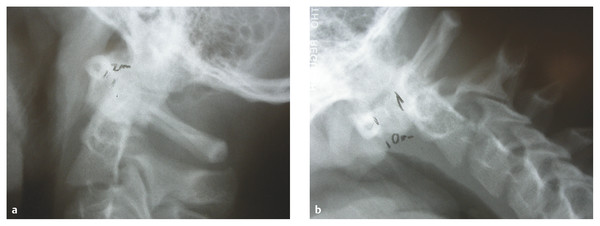
Fig. 61.3 Translational C1–2 subluxation. (a) Extension and (b) flexion radiographs demonstrating an atlantodental interval of 2 mm on extension and 10 mm on flexion, indicative of atlantoaxial instability in a 13-year-old boy following an assault to the head.
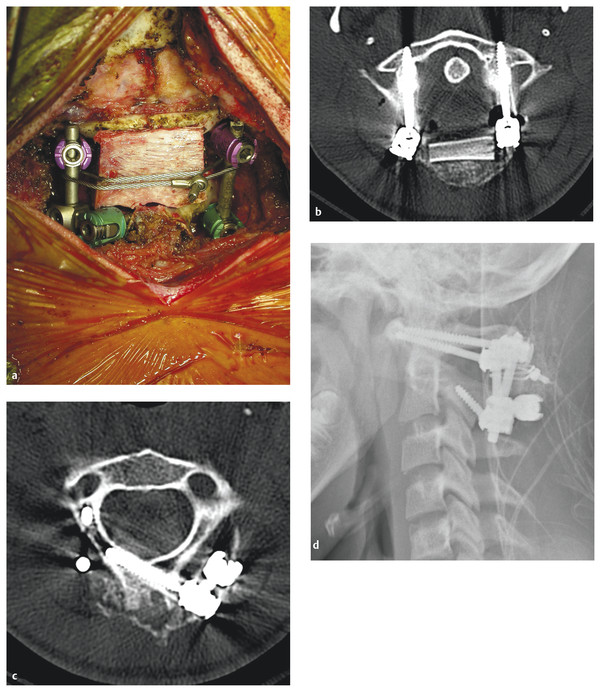
Fig. 61.4 Translational C1–2 subluxation. (a) Intraoperative photograph and (b,c) axial computed tomographic scans of a modified Goel-Harms type of fusion construct performed in the patient from ▶ Fig. 61.3 with traumatic C1–2 subluxation.63,64 Bilateral C1 lateral mass screws were placed and connected via metallic rods to the right C2 pars and left C2 laminar screws. An iliac crest bone graft was cabled in place between the posterior arch of C1 and the spinous process of C2. (d) Postoperative lateral radiograph of the fusion construct.
Clinical Presentation
Like those with AOD, most children with traumatic translational C1–2 subluxation are victims of high-speed pedestrian–motor vehicle accidents.31,39,40 Patients frequently present at one of two extremes: with minor neck pain, C2 hypesthesia, and subtle myelopathy or with severe head injury and anoxic encephalopathy.41 Long-term survivors of traumatic translational C1–2 subluxation often have good neurologic outcomes, likely because of selected survival at the injury scene.
Radiographic Diagnosis
Translational atlantoaxial subluxation is most commonly diagnosed by an abnormally large atlantodental interval (ADI) on a lateral plain radiograph (▶ Fig. 61.3a,b). An ADI greater than 5 mm is considered abnormal in children younger than 8 years old, whereas 3 mm is the upper limit of normal in older children and adults.42–44 As the ADI exceeds 6 to 10 mm, the alar ligaments and tectorial membrane may become secondarily damaged and occipitoatlantal instability may ensue. The retropharyngeal soft tissues are usually widened on lateral plain films. If open-mouth odontoid views are obtained, it may be possible to visualize an avulsed C1 tubercle where the transverse ligament inserts onto the anterior C1 arch.45 MR imaging may demonstrate rupture of the transverse ligament, with blood products, swelling, or rarely discontinuity of the ligament.46,47 Surgical treatment should be considered in patients with Down syndrome and an ADI of 6 mm or greater because 20 to 30% of these children will experience neurologic deterioration over time if intervention is not pursued.48–51
Treatment
Because traumatic atlantoaxial subluxation is primarily an extensive ligamentous injury, the generally accepted treatment is C1–2 internal fixation and fusion (▶ Fig. 61.4a–d).39,41,52 Postoperative immobilization in a halo vest is recommended if nonrigid fixation is used,45 but it may be deferred if C1–2 transarticular screws or other rigid internal fixation is employed.53
Atlantoaxial Rotatory Subluxation/Atlantoaxial Rotatory Fixation
Injury Description
Atlantoaxial rotatory subluxation/atlantoaxial rotatory fixation (AARS/AARF) represents a spectrum of abnormalities ranging from mild rotatory subluxation to absolute fixation with no motion (▶ Fig. 61.5, ▶ Fig. 61.6). Postulated mechanisms resulting in AARS/AARF include physiologic hypermobility of the C1–2 articulation, which can lead to rotary subluxation during sudden and vigorous turning of the head, occasionally resulting in a true bony lock.36 Other cases may be due to redundant synovial folds in children that become trapped in the C1–2 joint spaces at the extremes of rotation, jamming the articulation during counter-rotation; subsequent muscle spasm exacerbates the fixation.
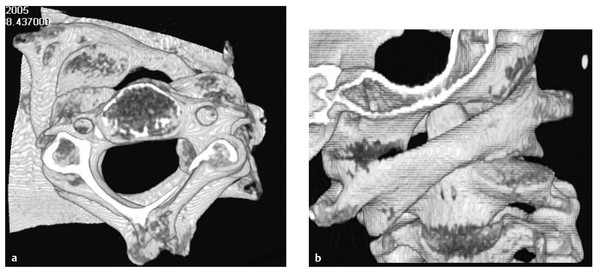
Fig. 61.5 Atlantoaxial rotatory subluxation (AARS). (a) Axial and (b) coronal three-dimensional reconstructed images of C1–2 in a 9-year-old girl with AARS that was refractory to conservative management. This patient ultimately required open reduction under general anesthesia with a posterior instrumented fusion.
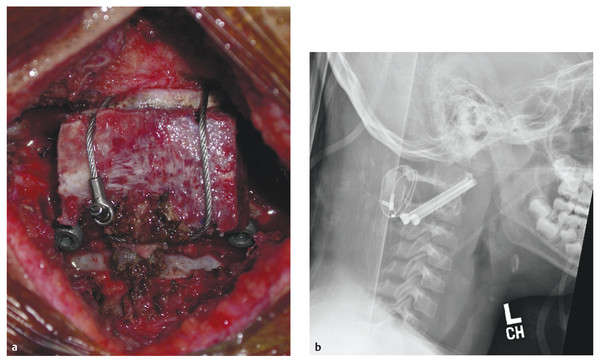
Fig. 61.6 Atlantoaxial rotatory subluxation (AARS). (a) Intraoperative photograph and (b) postoperative lateral radiograph of the fusion construct performed in the patient from ▶ Fig. 61.5 with refractory AARS. Following open reduction under general anesthesia, stabilization was achieved with bilateral C1–2 transarticular screws, and an iliac crest bone graft was cabled in Sonntag-Dickman fashion between the posterior arches of C1 and C2.65
Clinical Presentation
Only 30% of cases of AARS/AARF are traumatic in nature and usually result from only minor trauma.39,54 AARS/AARF has also been reported following inflammatory conditions of the head and neck, including pharyngitis, otitis media, retropharyngeal abscess (e.g., Grisel syndrome), and tumors.38 Children with AARS/AARF classically present with neck pain and the neck maintained in lateral flexion with the chin rotated to the opposite side (“cock robin” deformity). The neck pain typically worsens with attempted rotation to the corrective side. Children with this injury usually have no neurologic deficits; however, patients may rarely present with C2 radiculopathy or myelopathy.55 Although it has been reported, death directly attributable to AARS/AARF is exceedingly uncommon.36
Radiographic Diagnosis
Plain radiographs and static CT are generally unreliable for the diagnosis of AARS/AARF and have been supplanted by dynamic (“three-position”) CT studies (▶ Fig. 61.5a,b). Nonetheless, complete cervical radiographs with flexion–extension studies should still be obtained in children with suspected AARS/AARF to rule out fractures and gross instability. Before the advent of CT, the Sudeck sign (deviation of the C2 spinous process toward the side of the chin tilt caused by a conscious effort of the child to realign the frontal visual axis coupled with involuntary counter-rotation of the subaxial spine) seen on anteroposterior plain films was pathognomonic for AARS/AARF.36 Based on plain films, Field and Hawkins devised a classification scheme for AARS/AARF.55 Type I is rotatory fixation without anterior or posterior shift of the atlas; it is the most common type in children and is also the most stable because the transverse ligament remains intact. Type II is rotatory subluxation with anterior shift of the atlas more than 3 mm but less than 5 mm; this type involves compromise of the transverse ligament and is therefore considered more dangerous. Type III is similar to type II, however, there is greater anterior shift (> 5 mm). Type IV is rare and usually fatal, involving rotatory fixation with posterior shift of the atlas.
The relationship of C1 to C2 can be well visualized on dynamic CT, and CT is more accurate than plain films in diagnosing AARS/AARF.38,56 Lee and Pang developed a specific CT protocol wherein images are obtained with the patient’s head in certain positions to develop a C1–2 motion curve; deviation from the normal motion curve is then used to diagnose and determine the specific subtype of AARS/AARF.57 Based on their data, AARS/AARF can be classified into several types and subtypes. Type I is a true bony lock, with a fixed C1–2 angle as the head turns in the corrective direction. In type II, the C1–2 angle diminishes with corrective rotation; this type likely results from soft tissue interposition within the C1–2 joint, as opposed to a bony lock. Type II AARS/AARF is further subdivided into types IIA and IIB. In type IIA, the C1–2 angle never reaches 0 degrees because C1 never crosses to the other side of C2. This is the most common form of AARF. Conversely, in type IIB, C1 does cross to other side of C2, but only when C1 is at or less than 10 degrees. This suggests a pathologically sticky C1–2 articulation.
Treatment
The treatment of acute or subacute Field-Hawkins type I AARS/AARF generally consists of a combination of medical therapy (nonsteroidal anti-inflammatory drugs and muscle relaxants) and reduction via cervical traction.38,56,58 Following reduction, external immobilization for 4 to 6 weeks with a rigid collar is recommended. The duration of symptoms before treatment is a critical determinant of the response to conservative treatment. If treatment is not initiated within 1 month, the chances of restoring normal motion to the joint are much less than if treatment is begun acutely.38 Recurrence of AARS/AARF should be treated with repeated reduction and halo immobilization. Failure of reduction or a second recurrence, which may indicate transverse ligament incompetence, should prompt consideration of open reduction and C1–2 fusion (▶ Fig. 61.6a,b). Field-Hawkins types II and III should be considered inherently unstable because of injury to the transverse ligament and are most appropriately treated with open reduction and C1–2 fusion. Lee-Pang chronic type I (true bony lock) injuries are also unlikely to respond to conservative management. It is important to note that untreated atlantoaxial rotation can result in compensatory atlanto-occipital laxity and possible instability.38,59
Odontoid Fractures
Injury Description
True odontoid fractures are rare in children (▶ Fig. 61.7). In children, translational C1–2 subluxation is most frequently the result of epiphysiolysis at the dentocentral synchondrosis, which is located slightly lower than the base of the dens within the rostral aspect of the C2 vertebral body and is not fused until 8 to 11 years of age. Most dentocentral synchondrosis fractures occur in children younger than 3 years of age.60 These fractures tend to decompress the spinal cord and rarely lead to a neurologic deficit.
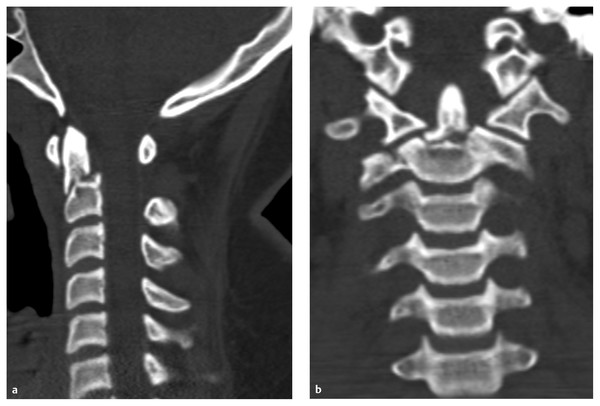
Fig. 61.7 Odontoid fracture. (a) Sagittal and (b) coronal computed tomographic scans demonstrating a type II odontoid fracture in an 18-year-old young man following a motor vehicle accident. Odontoid fractures in children are most commonly actually epiphysiolysis at the dentocentral synchondrosis (which is located slightly below the base of the dens in the rostral C2 body) rather than true odontoid fractures. The patient was successfully treated with halo ring immobilization.
Clinical Presentation
The majority of children with fractures of the odontoid process present after severe falls or motor vehicle accidents, although some fractures may occur after only minor trauma. Neck pain is the most common complaint. Some patients may also be obtunded from concomitant head injury, given the high percentage of cervical injuries that are associated with head trauma.61 The majority of children who present with odontoid fractures are neurologically intact because cord injury at this level is often acutely fatal.
Radiographic Diagnosis
True odontoid or dentocentral synchondrosis fractures can easily be seen on lateral plain films. There is often anterior angulation or displacement of the rostral odontoid process (▶ Fig. 61.7a). The ADI is normal in isolated fractures. An abnormal ADI suggests concomitant disruption of the transverse ligament. In epiphysiolysis, CT may demonstrate an abnormally widened growth plate.
Treatment
There are few recommendations for the treatment of odontoid injuries in children. In a series of 35 children, Sherk et al reported that only 1 child with an odontoid injury required surgical fusion.43 More recently, in a series of 13 children with odontoid fractures, 80% of those treated with halo immobilization for 10 to 18 weeks demonstrated a stable fusion. In general, children with odontoid fractures can be adequately treated with early external immobilization. C1–2 fusion is recommended in cases of failed fusion after immobilization or if the transverse ligament is disrupted.
Os Odontoideum
Injury Description
Os odontoideum was first described by Giacomini in 1886 and is a rare radiographic diagnosis defined as separation of an ossicle of bone from the odontoid process with no continuity to the body of the axis (▶ Fig. 61.8, ▶ Fig. 61.9, ▶ Fig. 61.10). Approximately 60% of patients present before 20 years of age, with a median age of 15 years. Although some authors have argued that os odontoideum is congenital, most now believe that it is an acquired lesion and represents a chronic nonunion from remote trauma. Functionally, os odontoideum is similar to a chronic type II odontoid process fracture, and most authors view it as unstable, with a risk for catastrophic injury to the upper cervical cord if left untreated.62
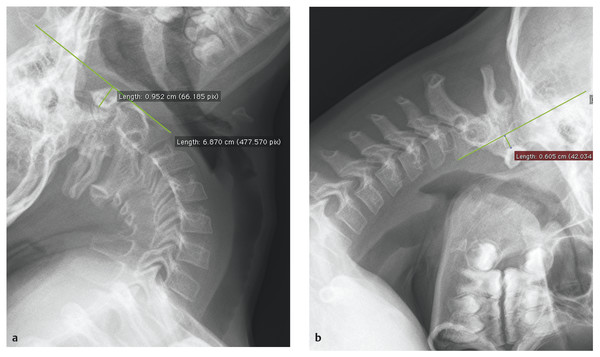
Fig. 61.8 Os odontoideum. Preoperative (a) extension and (b) flexion radiographs demonstrating gross instability with 15 mm of subluxation at C1–2 in a 9-year-old boy with os odontoideum who presented with vertebrobasilar insufficiency.
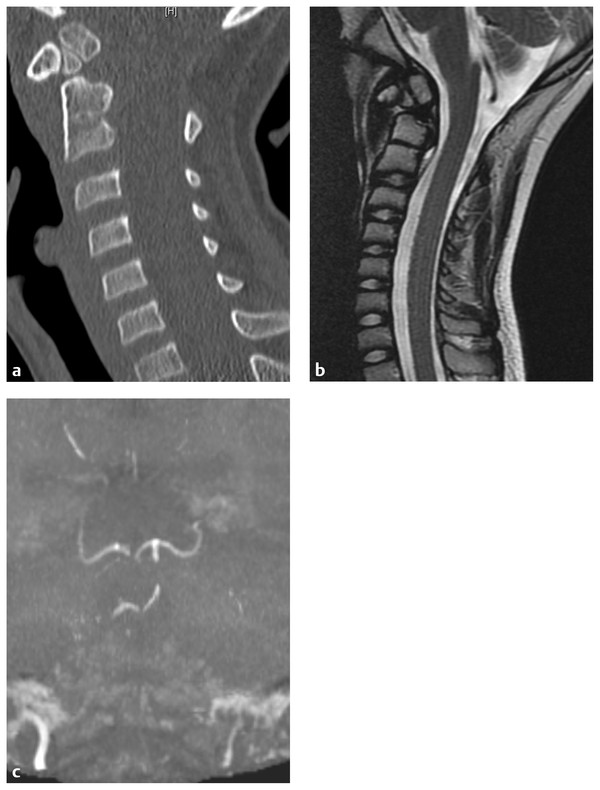
Fig. 61.9 Os odontoideum. Preoperative (a) sagittal computed tomographic and (b) sagittal magnetic resonance (MR) imaging of the same patient as in ▶ Fig. 61.8 clearly shows a well-corticated ossicle in the region of the dens in discontinuity with the remainder of the axis. (c) Preoperative MR angiogram from this patient demonstrating severe vertebrobasilar insufficiency from kinking of the vertebral arteries due to C1–2 instability.
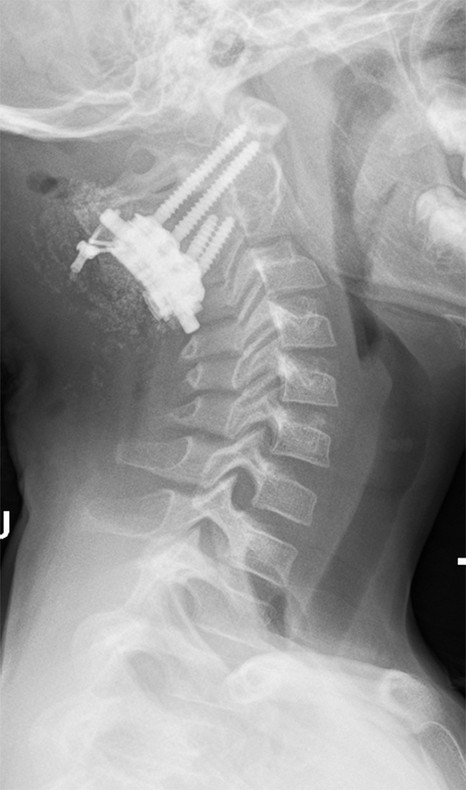
Fig. 61.10 Os odontoideum. Postoperative lateral radiograph of the fusion construct performed on the patient in ▶ Fig. 61.8 and ▶ Fig. 61.9. Following open reduction, stabilization was achieved with a Goel-Harms type of fusion construct,63,64 with bilateral C1 lateral mass and C2 pars screws and cabling of an iliac crest structural bone graft.
Clinical Presentation
The most common presenting symptom in patients with os odontoideum is neck pain, occurring in about two-thirds of patients. Approximately half of patients present following an instance of trauma, including falls, motor vehicle accidents, and sporting accidents. Neurologic symptoms on presentation may include myelopathy (23%) or transient paresthesias or quadriparesis (19%) following even relatively minor trauma.62 Headaches and symptoms suggestive of posterior circulation ischemia have also been reported (▶ Fig. 61.9c).
Radiographic Diagnosis
Os odontoideum can be diagnosed on lateral plain radiographs or CT scans demonstrating a well-corticated discontinuity between the odontoid peg and the body of the axis (▶ Fig. 61.8, ▶ Fig. 61.9, ▶ Fig. 61.10). The appearance is similar to that of a chronic type II odontoid fracture. The majority of patients demonstrate evidence of instability on flexion–extension radiographs (▶ Fig. 61.8a,b).62 MR imaging may demonstrate spinal cord edema in the C1–2 region.
Treatment
Most authors view os odontoideum as an unstable lesion with the potential for catastrophic cervical SCI from relatively minor trauma even in asymptomatic patients. Treatment should include decompression (if necessary), reduction, and internal stabilization and fusion (▶ Fig. 61.10).62 This may be achieved through the use of transarticular screws or other C1–2 instrumentation (i.e., a Goel-Harms construct63,64) in conjunction with a structural bone graft secured with cabling (e.g., the Dickman-Sonntag technique).65
Hangman’s (C2 Pars) Fracture
Injury Description
Hangman’s fractures are rare in the pediatric population (▶ Fig. 61.11a–c). When a hangman’s fracture does occur, it is most often due to a hyperextension mechanism, similar to that seen in adults. Classic causes include motor vehicle accidents, falls, diving accidents, and collisions during contact sports.
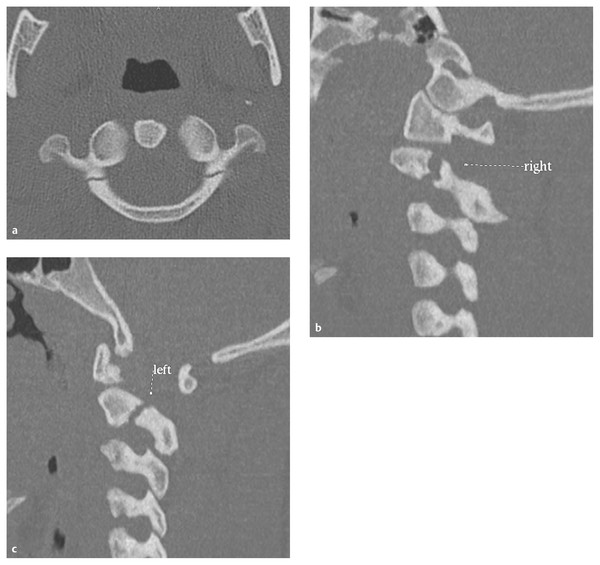
Fig. 61.11 Hangman‘s (C2 pars) fracture. (a) Axial and (b,c) parasagittal computed tomographic scans demonstrating a classic hangman‘s fracture with bilateral C2 pars involvement. Most fractures of this type can be treated with a rigid cervical collar if there is minimal displacement of the C2 vertebral body on C3. If there is more than 3 mm of displacement, external immobilization with a halo or Minerva brace should be strongly considered.
Clinical Presentation
Most children with C2 pars fractures present with neck pain. This fracture type typically results in widening of the spinal canal; therefore, neurologic deficits following a hangman’s fracture are rare. Only a few cases of neurologic injury following this injury have been reported in children.66,67
Radiographic Diagnosis
The diagnosis of a hangman’s fracture can be difficult in children because the neurocentral synchondrosis—the junction of the ventral and paired posterior ossification centers of the axis body—can mimic a fracture on oblique radiographs in patients younger than 7 years. Pseudo-subluxation at C2–3 may also be present in many children and can mimic true subluxation. When the diagnosis is in doubt on plain films, CT scans should be obtained through the region of interest.
Treatment
The treatment of C2 pars fractures is similar to that in adults.68 If the body of the atlas is not significantly displaced on C3, immobilization in a rigid collar should be adequate. If there is anterior displacement greater than 3 mm, external immobilization in a halo vest or Minerva cast is more appropriate. Surgical fusion is rarely required and is generally reserved for cases in which external immobilization fails to result in healing of the fracture or in which there is evidence of significant associated ligamentous injury.
61.1.2 Subaxial Cervical Spine Injuries
Purely Ligamentous Injury (Subluxation without Fracture)
Injury Description
These injuries include trauma to the supporting ligaments and soft-tissue structures of the cervical spine below C2. They range from very mild to severe injuries that completely disrupt supporting structures, leading to gross spinal instability.
Clinical Presentation
Nearly all patients with purely ligamentous injuries of the subaxial cervical spine present with neck pain. Neurologic deficits, including radiculopathy, myelopathy, or both, may also be seen. Neck pain that persists for several weeks following trauma is unusual and should be investigated with radiologic studies.
Radiographic Diagnosis
Plain radiographs in a child with purely ligamentous injury of the subaxial cervical spine may range from normal to grossly abnormal in appearance. Although static plain films may be normal, dynamic radiographs may unmask instability. The diagnostic criteria for determining instability in children with purely ligamentous injuries of the lower cervical spine are not well defined. White and Panjabi demonstrated that horizontal displacement of one vertebral body on another of more than 3.5 mm is consistent with significant ligamentous rupture in adults.42,69,70 The pediatric spine exhibits greater physiologic movement in the horizontal plane than does the adult spine. As such, displacement of up to 4.5 mm at a given segmental level may be considered normal and is termed pseudosubluxation, most commonly seen at C2–3 and C3–4.71,72 The following recommendations were developed by Pang and Sun to distinguish clinical instability from physiologic hypermobility in the subaxial cervical spine of children following trauma36:
In children older than 8 to 9 years, the spine is developmentally similar to that of adults. Therefore, horizontal displacement of more than 3.5 mm should be considered unstable.
In children younger than 8 to 9 years, the physiologic mobility of the subaxial cervical spine is increased, particularly at C2–3 and C3–4. Horizontal displacement of more than 4.5 mm should be considered unstable.
In children younger than 8 to 9 years, if displacement between 3.5 to 4.5 mm is accompanied by prolonged muscle spasm, pain, neurologic findings, or other abnormalities (i.e., an avulsed spinous process or widened interspinous space), then clinical instability should be assumed.
In addition to horizontal displacement, the degree of kyphotic angulation following trauma can be used to determine whether a given injury is stable. White and Panjabi determined that the angle between adjacent vertebrae in normal adults is always less than 11 degrees and that kyphotic deformities with a larger angle should be considered unstable.42,69,70 In children, however, the developing spine is more elastic and predisposed to recoil. Therefore, following trauma, the angle of displacement demonstrated on lateral X-rays or CT may be much less than the maximal excursion at the time of impact, and a high degree of ligamentous disruption may accompany a minor kyphotic deformity on imaging. Most authors agree that a kyphotic angulation of more than 7 degrees likely represents a significant ligamentous injury that may predispose the developing spine to further kyphosis and instability.73 Pang and Sun established the following algorithm to guide management in children with angular deformities of the subaxial cervical spine following trauma36:
If a neutral lateral radiograph demonstrates more than 11 degrees of angulation, with or without neurologic deficits, overt instability should be assumed. Dynamic imaging should be deferred and surgical fusion considered.
If a neutral lateral radiograph shows between 7 and 11 degrees of angulation and there is a neurologic deficit, the injury is considered unstable. The assumption is that the displacement during the moment of impact must have been larger than that currently observed on imaging to result in myelopathy. Dynamic imaging should be deferred and surgical fusion considered.
If a neutral lateral radiograph demonstrates between 7 and 11 degrees of angulation and there is no neurologic deficit, then dynamic imaging should be obtained. If the angulation increases to 11 degrees or more, the injury is considered unstable and surgical fusion is appropriate. If the angulation is unchanged, dynamic imaging may be repeated in several days to eliminate confounding from muscle spasm. If repeated imaging demonstrates less than 11 degrees of angulation and the study is satisfactory, then external immobilization should be pursued until dynamic radiographs confirm healing of ligamentous structures.
If initial angulation on a neutral lateral radiograph is less than 7 degrees but the patient has severe pain and muscle spasm, external immobilization (i.e., a hard cervical collar) should be considered until satisfactory dynamic studies can be obtained to rule out instability.
Evidence of instability in children with purely ligamentous injury of the subaxial cervical spine is often confined to a single level but may span two or more if the instability is particularly severe. CT scans are useful for confirming normal osseous anatomy and may also demonstrate indirect evidence of ligamentous injury, such as subluxation. MR imaging can be helpful to directly detect blood products in disrupted disk spaces or ligaments. On fat-suppressed T2-weighted MR imaging sequences obtained within 48 hours of trauma, high signal within the posterior interspinous and paraspinal soft tissues is suggestive of edema resulting from ligamentous and soft-tissue injury.
Treatment
Purely ligamentous injuries of the subaxial cervical spine that do not demonstrate gross instability on radiographic imaging can be managed conservatively with oral analgesics and, if necessary, a soft cervical orthosis for comfort. Most pain is associated with muscle spasm that usually resolves within 1 to 2 weeks after the injury. In children with more extensive ligamentous or soft-tissue injury that results in instability, operative reduction, internal fixation, and fusion should be considered. There are few series reporting on the management of purely ligamentous subaxial cervical spine injuries in children. Finch and Barnes used primary operative stabilization to treat most children with this injury; however, they suggested that in at least some cases, external immobilization might have been sufficient.74 Meanwhile, Pennecot et al treated minor ligamentous injuries with closed reduction and collar immobilization.75 Despite this, however, 8 of 11 children in their series had injuries that ultimately required fusion. When operative management is undertaken, the operation to be performed depends on the specific pathology, as well as on surgeon and patient preference. Options include anterior approaches with allograft or autograft and plate/screw fixation, or posterior instrumented fusion. In cases of severe instability, instrumented fusion from combined anterior and posterior approaches may be considered to ensure proper alignment and long-term stability.
Osseous Anterior Column Injuries
Injury Description
Osseous anterior column injuries of the subaxial cervical spine (based on a two-column model) encompass all vertebral body fractures from C3 to C7, including chip/teardrop, longitudinal, wedge compression, and burst fractures (▶ Fig. 61.12, ▶ Fig. 61.13). Fractures isolated to the anterior column are the most common fractures of the pediatric subaxial cervical spine.60 The intervertebral disks of children have a higher collagen concentration, making them less predisposed to rupture when subjected to traumatic stresses. Instead, axial loading and compressive forces are transmitted to the annulus fibrosis and subsequently to adjacent vertebral bodies, which may then fracture. Burst fractures of the vertebral body may be categorized into one of five subtypes according to Denis: (1) type A, with both end plates involved; (2) type B, with only the superior end plate involved; (3) type C, with involvement of the inferior end plate only; (4) type D, which exhibits burst–rotation; and (5) type E, with burst–lateral flexion.76

Fig. 61.12 C7 burst fracture. (a) Sagittal computed tomographic scan and (b) magnetic resonance image demonstrating an unstable C7 burst fracture with spinal cord compression in a 17-year-old boy presenting with upper extremity paresthesias and numbness following a snowboarding accident. Also seen is a stable C5 anterior compression fracture with minimal angulation and loss of body height.









