45 Spinal Cord Myelopathies
Acute Myelopathies
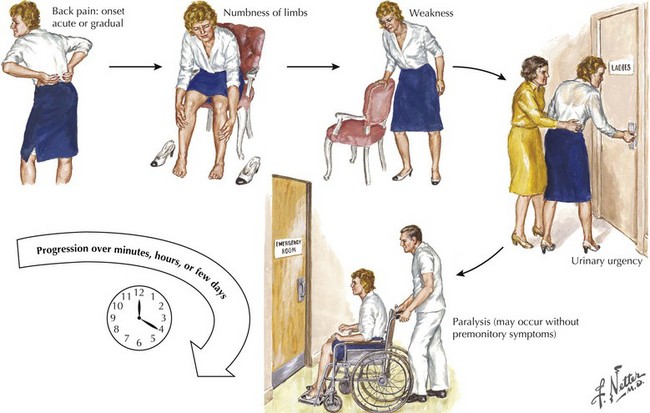
The patient presenting with an acute myelopathy provides one of the most challenging emergencies that a neurologic physician will confront. These clinical settings require expeditious and thorough evaluation including careful history, detailed neurologic examination, and immediate definitive neuroradiologic studies. In most instances, a magnetic resonance image (MRI) is the perfect study. The primary exception is the patient with a pacemaker or other medical apparatus that is not compatible with a magnet. Expeditious therapeutic intervention can sometimes reverse/stabilize a potentially disastrous clinical outcome (Fig. 45-1). Three common causes of an acute myelopathy are spinal fracture/dislocations (Chapter 60), acute transverse myelitis in young adults, and metastatic tumors in late middle- and senior-aged individuals (Chapter 53).
Acute Extradural Spinal Lesions
Trauma
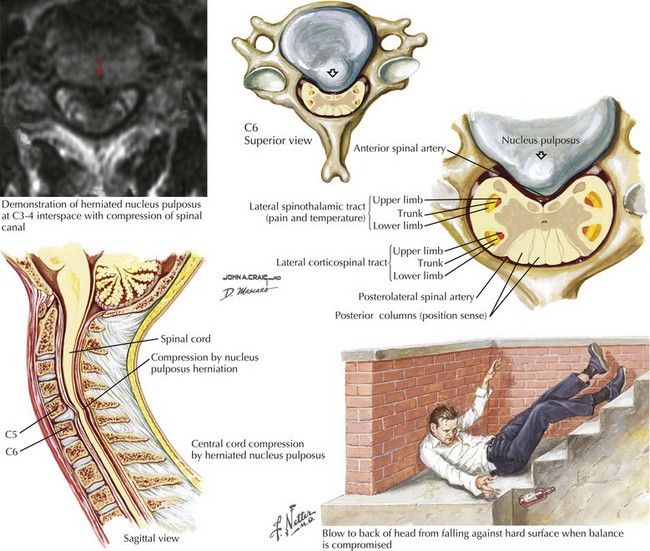
Central Herniated Disc
Clinical Vignette
Comment: Initially, this patient was thought to have a basically untreatable brainstem stroke, that is, a lesion in an entirely different part of the neuraxis. A more careful subsequent clinical examination, lying the patient on his side and examining for a specific sensory level, was the key to diagnosis, as patients with brainstem stroke rarely have total loss of sensory function in a spinal cord–level distribution (see Figs. 44-11 and 44-12).
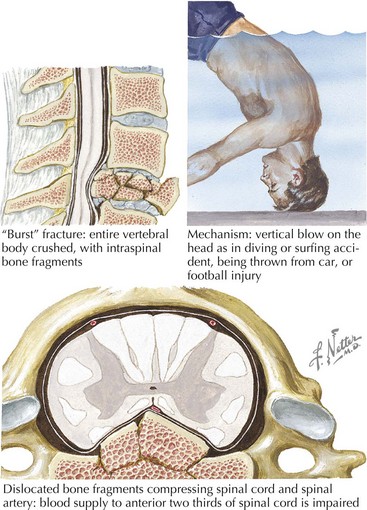
Acute spinal cord injuries, with subsequent paraplegia or quadriplegia, are among the most dreaded sequelae to a serious bodily injury (Box 45-1). There is a tragic propensity for traumatic myelopathies to occur among vigorous and healthy young persons. Automobile and motorcycle accidents as well as sports injuries are the most common etiologies. Gunshot wounds, whether resulting from war, accident, or assault, are another source of traumatic spinal cord injury.
Box 45-1 Acute Extradural Extramedullary Myelopathies
Cervical spinal fracture dislocation with resultant ligamentous tear, allowing bony fragments to directly tear or transect the spinal cord, is the common denominator in this setting (Fig. 45-2). Sometimes, there is concomitant compromise of the spinal arteries causing an associated spinal cord infarction, hematomyelia, or both. Typically, in the acute setting, spinal shock results with complete paralysis, loss of sensation, areflexia distal to the trauma site, and loss of bladder and bowel function.
Occasionally, these traumatic spinal lesions are amenable to immediate surgical correction or external traction (Chapter 60). Prognosis is always guarded. Once emergent management is completed, these patients are cared for at specialized spinal rehabilitation centers. Treatment of autonomic and sphincter dysfunction has greatly improved the long-term survival for many patients. Spinal cord repair, leading to functional recovery, is one of the greatest challenges for 21st-century neuroscientists.
As these lesions are eminently treatable with neurosurgical intervention, consideration of these less common lesions is vital in patients who have sudden unexplained falls leading to immediate paralysis. Anatomically, the extruded disc compressed the anterior spinal cord between two vertebral bodies. Occasionally, these lesions present subacutely or chronically. Because associated bony pain or tenderness may be present, these lesions often mimic metastatic or primary tumors. However, if the patient does not have a history of malignancy, a benign mechanism, such as a central disc, must be sought (Figs. 45-3 and 45-4). Rarely, a dural arteriovenous malformation (AVM) or spinal epidural hematoma (SEH) mimics this clinical picture.
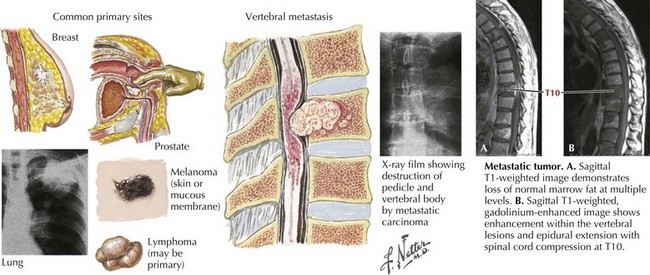
Metastatic Malignancies
One of the most common etiologies for a nontraumatic acute or subacute extradural myelopathy occurs with various forms of metastatic carcinoma or lymphoma (Fig. 45-5). These patients initially develop spinal pain secondary to bony metastases. Within a matter of days, they begin to note symptoms of spinal cord compromise, usually with a spastic gait or bladder. Once these symptoms appear, the progression to paraplegia may be very rapid. On occasion, the spinal metastasis may be the presenting sign of a previously undiagnosed lung cancer. Emergency MRI is indicated. Treatment of metastatic extradural tumors includes radiation and sometimes surgery, chemotherapy, or both. In contrast to metastatic disease, primary intrinsic spinal cord tumors are usually either intradural extramedullary or of intramedullary origin.
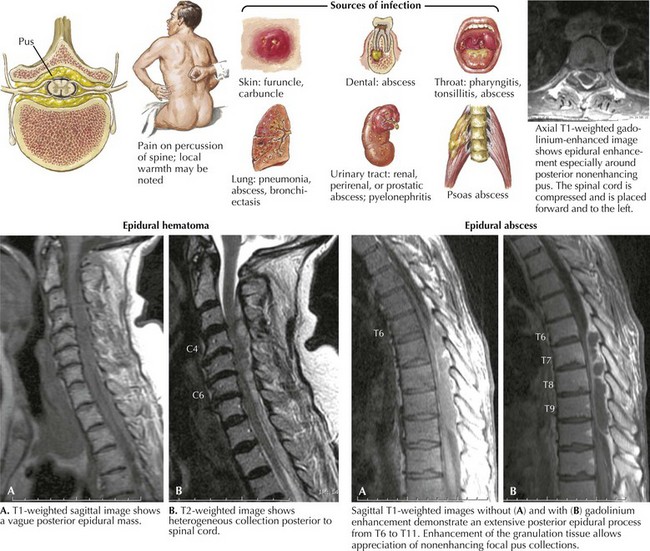
Epidural Abscess
Clinical Vignette
Epidural spinal abscess is a rare clinical process occurring in 2–20 cases per 100,000 hospital admissions. Its incidence appears to be increasing; these are usually seen in middle-aged adults, more often men. Despite its rarity, the potential for an epidural abscess to cause permanent paraplegia makes it one of the most urgent spinal cord emergencies (Fig. 45-6). Even though back pain is such a ubiquitous and usually benign process, it is very important for any physician to consider the potential diagnosis of an epidural abscess in every patient presenting with acute and increasing back pain, especially when febrile. The epidural space in the posterior thoracic cord is the primary site for an epidural spinal abscess to develop. These may extend to the cervical cord and rarely into the lumbar spine. Experimental studies suggest that the mass effect of the abscess, leading to cord compression, is the important clinicopathologic mechanism.
Staphylococcus aureus is the predominant etiologic microorganism leading to epidural spinal abscesses. Usually a distant septic focus provides bacterial seeding via the bloodstream, for example, skin furuncles, dental abscesses, simple pharyngitis, or a recently infected traumatic site (see Fig. 45-6). Often there is a concomitant history of diabetes mellitus, alcoholism, drug abuse, or recent spinal or extraspinal trauma. Less commonly, epidural spinal abscesses develop subsequent to vertebral osteomyelitis, pulmonary or urinary infection, sepsis, or extremely rarely bacterial endocarditis. Invasive procedures, including epidural anesthesia, spinal surgery, vascular access lines, and paravertebral injections, also provide potential mechanisms for bacterial seeding. Corticosteroid therapy may contribute to immune suppression and the possibility of secondary nosocomial infections.
Acute Intradural Intramedullary Spinal Lesions
Myelitis Secondary to Multiple Sclerosis
Clinical Vignette
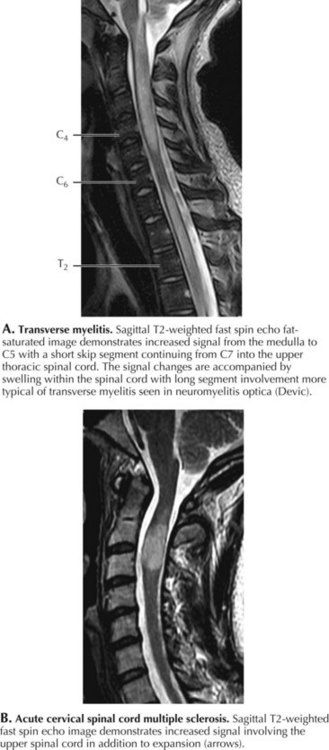
Cervical spine MRI demonstrated an area of increased signal with ill-defined enhancement located posteriorly and on the left side of the cord (Fig. 45-7A). Brain MRI with and without gadolinium demonstrated a few periventricular lesions and other abnormalities oriented perpendicularly along vessels (Dawson fingers) within the corpus callosum. Visual evoked responses (VERs) were prolonged for her right eye. Her cerebrospinal fluid (CSF) was significant for 10 white blood cells (99% lymphocytes, 1% monocytes), and the presence of oligoclonal bands that was not identified in her serum.
Comment: This vignette presents a classic clinical picture of early multiple sclerosis (MS). The patient has an incomplete demyelinating myelitis consistent with classic hemicord syndrome, affecting ipsilateral motor and proprioceptive function and crossed sensory fibers. This is known as the Brown–Sequard syndrome. However, she also had involvement of her right arm, implying extension into the right anterior horn. The presence of the subclinical brain MRI abnormalities, as well as the prolonged VERs, point to multiplicity of demyelinating lesions in time and space consistent with the diagnosis of MS (Table 45-1).
Table 45-1 Acute Intradural Intramedullary Myelopathies
| Inflammatory Transverse myelitis | |
| Vascular Anterior cord syndrome | |
| Infectious | |
| Trauma Central cord syndrome |
Transverse Myelitis
Clinical Vignette
Very often, there is no underlying pathology identified with many transverse myelitis (TM) cases. Acute transverse myelitis most likely represents another type of autoimmune CNS disorder. A nonspecific “viral infection” may be the inciting mechanism or sometimes a bacterial infection, and rarely this may occur subsequent to immunization. Sometimes, a transverse myelitis is preceded by or associated with optic neuritis. This is known as neuromyelitis optica (NMO), an unusual autoimmune demyelinating disorder associated with a very specific serum autoantibody referred to as NMO-IgG (Fig. 45-7). This antibody binds to the CNS-dominant water channel, aquaporin 4; this is a structure that is normally present on astrocytes. The diagnostic criteria for neuromyelitis optica include optic neuritis, acute myelitis, and two of the following three: brain MRI not characteristic for multiple sclerosis, contiguous spinal cord MRI lesion extending over three or more vertebral segments, and NMO-IgG positive status.
MRI with gadolinium is the procedure of choice to exclude compressive lesions, especially when history and exam suggest a specific level of spinal cord dysfunction (see Fig. 45-7). Brain lesions consistent with MS are demonstrated with MRI in approximately half of all TM patients. Transverse myelitis appears with T2 signal hyperintensity on MRI. The area of signal abnormality may be focal or extensive in cross section and length. Gadolinium enhancement is frequent. Cord swelling is present to variable degrees. Large cross-sectional area, multisegment length, cord expansion, and peripheral enhancement are most consistent with a diagnosis of TM. In contrast, MS lesions tend to be smaller, usually involving only 1–2 segments, and are often multifocal. Total cross-sectional area and multisegment length are uncommon in MS, although cord expansion and enhancement are frequent with larger acute inflammatory MS lesions. Gadolinium-enhanced brain MRI, and optical coherence tomography (OCT), even more than visual evoked potentials (Chapter 46), help determine the presence of multifocal demyelinating disease. Associated cerebral white matter lesions and oligoclonal bands in CSF increase the later probability of developing unequivocal MS. Oligoclonal bands, however, are nonspecific for multiple sclerosis and not always present in individuals with multiple sclerosis.
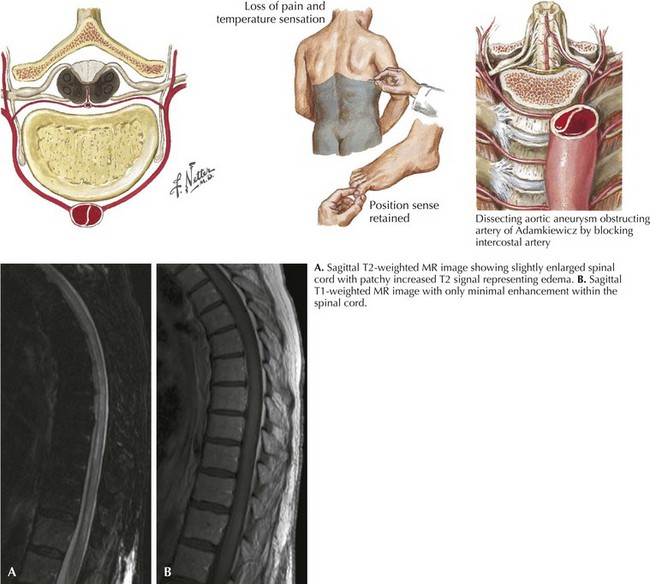
Spinal Cord Infarction/Ischemic Myelopathy
Anterior Spinal Artery Syndrome
Clinical Vignette
The clinical picture of paralysis secondary to loss of corticospinal tract function and sensory change from impaired spinothalamic function, as well as infarction of the anterior horn cells, but with very preserved posterior column function, is classic for an anterior spinal artery distribution spinal cord infarction (Fig. 45-8). Onset of anterior spinal artery syndrome, although usually sudden, may occasionally be gradual over hours or days.
Chronic Myelopathies
Extradural Myelopathies
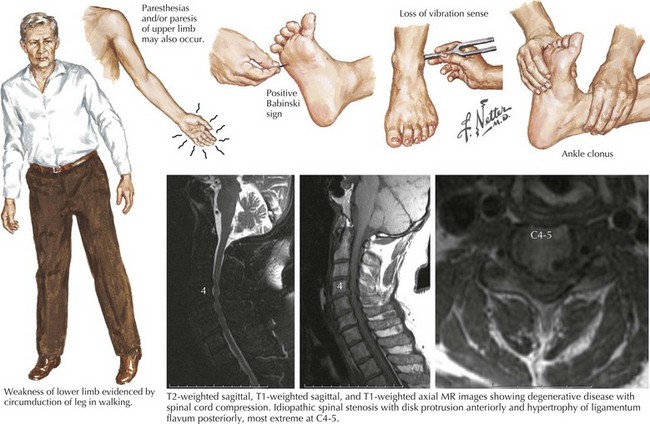
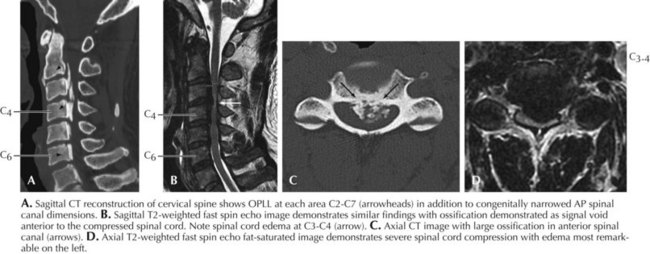
Cervical Spondylosis
Clinical Vignette
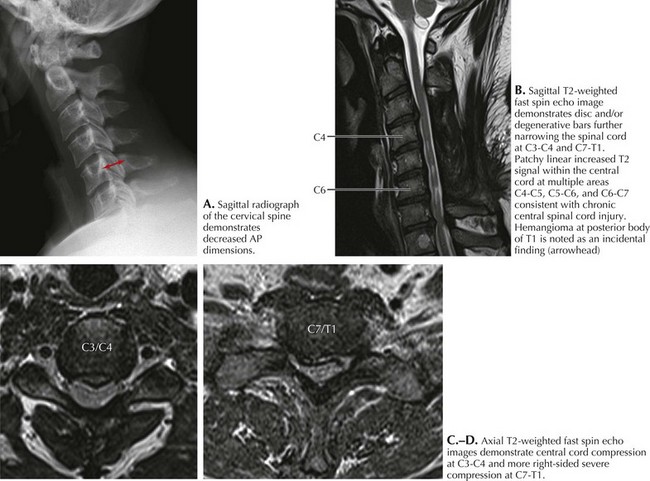
Spondylosis, a normal aging process, is the most common cause of a cervical myelopathy (Figs. 45-9 and 45-10; Box 45-2). This results from disc degeneration followed by reactive osteophyte formation, fibrocartilaginous bars, spondylotic transverse bars, articular facet hypertrophy, and thickening of the ligamentum flavum causing spinal canal narrowing. Subsequently, gradual spinal cord compression may occur; it is particularly likely in patients having congenitally narrowed spinal canals. In its simplest form, a chronically herniated central nucleus pulposus in patients with congenital stenosis can produce a cervical myelopathy. Although many senior individuals have radiographic signs of cervical spondylosis, most are asymptomatic. When a myelopathy develops, clinical findings can present acutely, subacutely, or over many years. Sometimes both a cervical myelopathy and adjacent radiculopathy may occur in the same spondylotic patient.