♦ Preoperative
Operative Planning
- The patient’s history, pain description, physical examination, imaging studies, and psychological evaluation support the diagnosis and reveal no contraindications
- A screening trial with a temporary electrode and external generator results in satisfactory pain relief, typically ≥ 50%, despite provocative activity on stable or reduced analgesics
Equipment
- Fluoroscope and padded fluoroscopy table
- For screening trial (in fluoroscopy suite)
- Percutaneous catheter electrode
- External pulse generator
- Percutaneous catheter electrode
- For spinal cord stimulation implantation or screening with plate/paddle electrode (in operating room)
- Electrode with extension cable
- Implantable pulse generator
- Electrode with extension cable
Operating Room Set-up
- Fluoroscopy equipment for anteroposterior and (as necessary) lateral imaging
Anesthetic Issues
- Local anesthetic infiltration alone is ideal during electrode insertion as the patient describes pain/paresthesia overlap
- Intravenous sedation with intermittent boluses or propofol drip facilitates implantation of a surgical plate/paddle electrode and subcutaneous tunneling
♦ Intraoperative (Fig. 145.1)
Positioning
- Patient prone or seated for percutaneous catheter electrode with target area neutral
- Patient prone or semilateral for surgical plate/paddle electrode
Planning of Sterile Prep
- Normal sterile prep
- Intravenous antibiotic prophylaxis
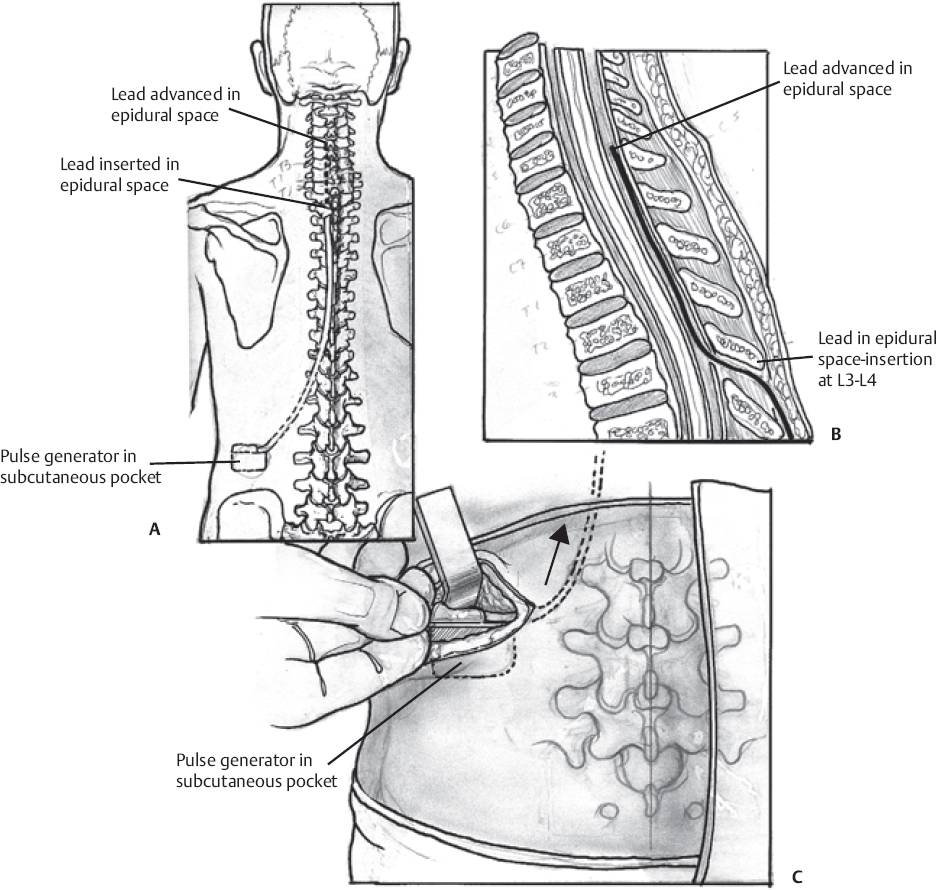
Fig. 145.1 Schematic illustrating (A) spinal cord stimulator placement, (B) catheter tip location in epidural space, and (C) pulse generator in subcutaneous pocket.
Percutaneous Catheter Electrode Insertion for Screening Trial
- Starting 1 to 2 segments (depending on the patient’s girth) below the target interlaminar space, advance a Tuohy needle at a shallow angle under fluoroscopy
- Increase the degree of spinal flexion if additional interlaminar space is needed
- Confirm epidural space entry with loss of resistance to a Seldinger guide wire (injected air or saline can interfere with steering and with test stimulation)
- Using bipolar test stimulation with adjacent contacts, identify the physiologic midline at each level as the electrode is advanced incrementally along the radiographic midline to the desired longitudinal location, repositioning as needed to achieve the requisite symmetry and concordance of paresthesia/pain
- Withdraw the Tuohy needle and suture the lead to skin
Percutaneous Catheter Electrode Implantation
- Insert the electrode as above; make a longitudinal incision around the Tuohy needle, down to dorsal fascia; place self retaining retractors
- Place two no. 0 nonabsorbable (e.g., Tevdek, Teleflex Inc., Limerick, PA) sutures through supraspinous ligament caudal to the needle, then remove the needle
- Pass the anchoring sleeve/strain relief through dorsal fascia, then tie one suture around it
- Inject a small amount (< 0.1 mL) of silicone elastomer adhesive between the inner surface of the sleeve and the outer surface of the lead
- Add ligatures around the anchor as appropriate and use the most caudal anchoring suture to secure the sleeve flat against the dorsal fascia
- Confirm the electrode position fluoroscopically
Surgical Plate/Paddle Electrode Implantation
- Use fluoroscopy to center the 1- to 2-in incision site on the planned minilaminectomy area, just below the intended position of the most caudal contact
- Heavily infiltrate the paravertebral muscles with local anesthetic and dissect them subperiosteally
- Perform a minilaminectomy of sufficient length and breadth to allow insertion of the electrode at a shallow angle, proceeding cephalad beneath intact lamina
- Insert electrode; test stimulate for symmetry and pain/paresthesia concordance
- Using a sleeve/strain relief, anchor the lead wire to supraspinous ligament
Pulse Generator Implantation
- Common implantation sites are the lateral abdomen and lower chest wall, the infraclavicular area (for cervical electrodes), and the upper buttock below the belt line (but this increases stress with flexion/extension)
- Plan the incision and the pocket to avoid wound closure directly over the implant
- Skin thickness should be sufficient to maintain integrity and patient comfort without compromising power transfer or telemetry; 1 cm is typical
- Tunnel subcutaneously and advance proximal lead and/or extension from the electrode(s) to the generator; avoid connectors (which introduce stress and can cause discomfort)
- Internalize loops of excess wire in the pocket beneath the generator (for strain relief)
- Close all incisions in layers
♦ Postoperative
- Program the system and educate the patient to maximize pain/paresthesia overlap, energy efficiency, and safety
- Monitor the patient for complications
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue








