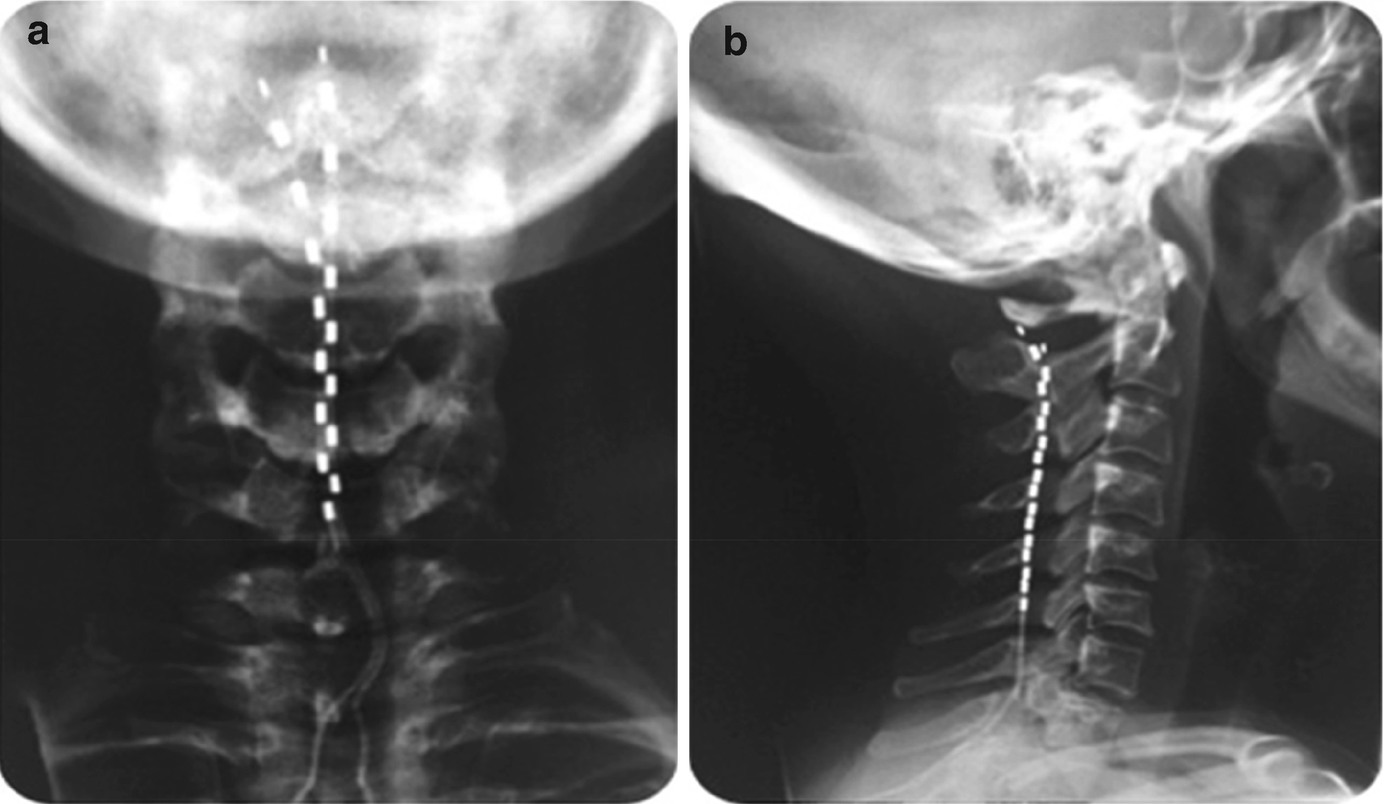
Anteroposterior (a) and lateral (b) radiographic view of the cervical spine to demonstrate the final position of the implanted lead within the posterior epidural space in a chronic migraine patient
Baseline data were available for 19 subjects (43 ± 10 years; 84% female), who had failed an average of 11.7 ± 3.2 preventive treatments at the time of recruitment. The average number of headache days at baseline was 23.3 ± 5.2 days of which 21.6 ± 6.6 days were migraine days. The average migraine-specific quality of life (MSQ) score at baseline was 32.0 ± 15.7. Compared to baseline, the average reduction in headache days at 12 weeks was 3.9 days, which increased to 4.9 days at week 24. The average reduction in migraine days at 12 weeks was 6.2 days/month, which increased to 7.2 days at weeks 24. Thirty-eight percent of the subjects at week 12 and 43% at week 24 obtained a 30% reduction in headache days; 44% of subjects at week 12 and 50% of subjects at week 24 reported a reduction of more than 30% in migraine days compared to baseline. In 50% of the subjects, the CM pattern reverted to an episodic pattern (<15 headache days/month) at week 24. We observed an improvement in the MSQ score of an average of 17.2 points at 24 weeks (50.8 ± 23.4). At week 24, five subjects reported pain at the site of implant, four reported musculoskeletal pain in the cervical and shoulder area and one experienced slight lead movement. No subjects required any further surgical procedure.
This preliminary evidence suggests that high cervical SCS, contrary to the first study in CCH, is a safe and well-tolerated treatment at least in experienced hands. In the only large-scale, prospective, controlled study evaluating ONS for CM with 1-year follow-up to date, the safety profile of the therapy was questioned by the authors themselves, as 183 device- or procedure-related AEs occurred, 8.6% of which required hospitalization and almost 41% required additional surgery [30]. In the first HF10 SCS study, four subjects (24%) required an additional surgical procedure, whereas none of the 20 patients implanted in the more recent trial required further surgery at 6 months f/u.
In terms of efficacy, these initial evidence may suggest that HF10 SCS is beneficial in rCM. One of the strengths of these studies is the fact that the migraine population included in these two trials was very refractory to medical treatments. Not many trials in ONS included a population who failed that many treatments and Botox. The ONS RCT in CM included patients who failed at least two preventive treatments; however, it was unclear the mean numbers of treatments failed at enrolment. Furthermore, none of the patients tried Botox according to the PREEMPT trial in those trials. Botox is currently considered the standard of care for CM treatment [31, 32]; hence, its failure has been included in the most recent international guidelines for the definition of rCM [33]. A recent prospective open-label study, which studied the efficacy of a group of 35 rCM patients who failed an average of 9.36 (±2.61, range 4–19) preventative treatments, is somehow comparable to the HF10 SCS study populations, although there was no mention of the proportion of patients who failed Botox before implant [34]. At baseline, the patient group had a mean of 26.83 (±6.74) moderate to severe headache days. At a median f/u of 42 months, there was an average reduction of 5.8 headache days/month and 34.3% of rCM patients obtained >30% in monthly headache days. Although it is not appropriate to compare these trials, it is possible that HF10 SCS is as effective or even more effective than ONS in rCM. Similarly to chronic pain, paraesthesia may not be needed to obtain relief in headache conditions.
Anteroposterior (a) and lateral (b) radiographic view of the cervical spine to demonstrate the final position of the implanted leads within the posterior epidural space (SUNA patient, 42 months follow-up)
7.5 Safety and Tolerability
SCS is considered a moderately invasive neuromodulation treatment, more invasive than ONS as far as headache disorders are concerned. Some of the complications may be severe, but they are extremely rare. These include spinal epidural haematoma, cerebrospinal leak and neurological deficit [36]. Common adverse events include hardware-related (e.g., lead migration, lead malfunction, connection malfunction and battery failure) and biological complications (e.g., infection, haematoma, seroma, dural puncture, nerve injury, IPG pocket pain). Most frequent AEs are infections and lead migrations with an average rate of 5% and 15% in the chronic pain literature [37]. In recent years, lead migration rate reported in clinical trials is decreasing arguably due to the better selection of patients, the improved device technology and more sophisticated technique of anchoring [38–40].
A panel of experts from the International Neuromodulation Society (INS) [41] has considered SCS of the cervical spine and of the thoracic spine similar in terms of adverse events [42]. The HF10 device (the Nevro Senza System) has received CE mark in 2010, TGA approval in 2011 and FDA approval in 2015 for treatment of failed back surgery syndrome, intractable low back pain and leg pain.
7.6 Spinal Cord Stimulation: Postulated Mechanisms of Action
SCS mechanisms of action are still not completely understood. Current hypotheses propose that a complex set of interactions at several levels of the nervous system mediate the effects of SCS. It has been postulated that SCS activates large A-beta fibres at the level of the dorsal horn and induces paraesthesia and simultaneously modulates the C-fibres transmission of pain signals [43, 44]. Animal studies have suggested a possible SCS target of stimulation at the wide dynamic range (WDR) neurons of the dorsal horn [45].
Later, several studies demonstrated a role of structures outside the dorsal horn and located in central and peripheral levels, such as supra-spinal circuits (demonstrated in fMRI studies) [46], and implication of descending inhibitory signals [47].
HF10 SCS has been shown to inhibit evoked afferent nociceptive inputs by modulating WDR neurons activity in the spinal cord of different animal models [48]. WDR neurons are spinal interneurons able to integrate C-fibres nociceptive inputs as well as multisynaptic inputs from myelinated A-type fibres signals before projecting to the brain. Significant modulation of WDR neuronal activity has been recorded in animal models of acute nociceptive and chronic neuropathic pain during SCS treatment [49].
Currently, no animal studies have tried to elucidate the mechanism of action of the high-frequency stimulation in headache disorders. Similarly to ONS, a modulation of the trigemino-cervical complex as well as a potential slow neuromodulatory effect at cortical levels may be postulated.
More research is needed to shed light upon the effect of paraesthesia-inducing and paraesthesia-free SCS and ONS neuromodulation modalities in headache models. Besides producing more scientifically robust basis to justify these therapies, such research may advance the understanding of the physiology of the trigemino-cervical pathway, which is pivotal in headache medicine.

Full access? Get Clinical Tree


