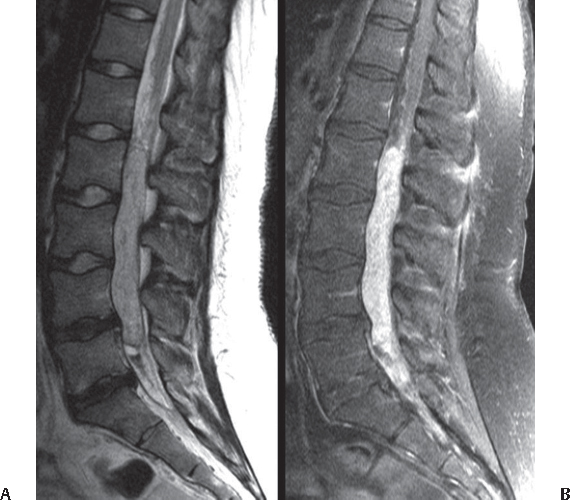
36 Are older or younger patients more likely to present with extradural malignancy? Patients >30 years of age Are primary tumors or skeletal metastases more common? Skeletal metastases (by a ratio of 25–40:1)1 With respect to primary lesions, what are some positive prognostic signs at presentation? Tumors that are likely benign: • Occur in younger patients • Involve posterior elements (versus the vertebral body) What are some examples of benign primary bony lesions? • Osteochondroma • Osteoid osteoma • Osteoblastoma • Giant cell tumor (but has malignant potential) • Aneurysmal bone cyst • Hemangioma • Eosinophilic granuloma In general, how are these lesions identified? By MRI and/or CT And how are they treated? Resection ± Preoperative embolization ± Postoperative radiation List examples of malignant primary tumors of the spinal column. • Chordoma • Chondrosarcoma • Osteosarcoma • Ewing’s sarcoma • Plasma cell myeloma What are the imaging modalities of choice? MRI for extent of tumor, and CT to assess for bone invasion/destruction What is the preferred treatment for these lesions? Resection ± Chemotherapy ± Radiation ± Embolization True or false: Spinal metastases occur from virtually all kinds of systemic carcinomas. True; as many as 90% of patients with systemic carcinoma also have spinal disease1 True or false: A patient with acute neck or back pain and a known carcinoma has metastasis to the spine until proven otherwise. True. Which carcinomas are most likely to metastasize to the spine? Breast > prostate, lung > renal > thyroid and multiple myeloma What is their most likely site of metastasis in the spine? Vertebral body (85%) > posterior elements (10–15%) > epidural space (<5%) Discuss some hypotheses as to the spread of metastatic carcinoma to the spine. • Hematogenous spread • Direct flow from segmental arteries from the lungs or through Batson’s paravertebral venous plexus • Direct extension into the spinal column from the primary site Is surgery the mainstay of treatment for metastatic extradural tumors? No, the goal is palliative care (pain control and preservation of neurologic function). • Uncertain diagnosis • Neurological compromise • Spinal instability • Pathological fracture • Intractable pain • Radiation failure What is the most common presenting complaint with an intradural extramedullary tumor? Back or neck pain in a radicular pattern, particularly at night What is the imaging modality of choice? MRI, with and without gadolinium (T1 images for solid tumor, T2 for CSF and tumor-associated cysts) What is the role of CT myelography in the management of spinal cord lesions today? Limited mostly to use in situations where patients cannot tolerate MRI, or when spinal instrumentation creates artifact-degrading image quality True or false: Intradural extramedullary tumors are the most common kind of intradural tumor. True, at least in adult populations. These tumors comprise about two thirds to three fourths of intradural lesions in adults, but slightly less than half in children.1 What are the two most common forms of intradural extramedullary tumor, and how does their etiology affect outcome? • Nerve sheath tumors: arise from the dorsal roots, so nerve preservation is difficult during resection • Meningiomas: arise from arachnoid, so they offer better chance of nerve preservation Which of these may demonstrate a “dumbbell” presentation? Nerve sheath tumors, when presenting with both an intra- and extradural component Can an ependymoma present in the extramedullary space? Yes, though only rarely Is complete resection of the dural attachment meningiomas necessary to decrease recurrence? No, recurrence rates seem to be the same whether dural attachment is resected or not, so this step may be avoided to minimized damage to the cord.2 What tool is particularly useful for resecting meningiomas, given the tumor’s firm texture? Microsurgical laser, which can be used as a scalpel to vaporize or resect the tumor What other tool (that has largely replaced suction and bipolar cautery) is of special utility in spinal cord tumor resection? Ultrasonic aspirator, which uses high-frequency sound waves to break up tumor tissue and then aspirates them using a suction device What approach is typically used in the resection of extramedullary tumors? Posterior, and occasionally dorsolateral True or false: Extramedullary tumors are often completely resected. True; unlike intramedullary lesions, they can typically be completely removed (if their location is favorable and they are not too large). Piecemeal resection is acceptable for larger lesions. What is the most important strategy to ensure complete resection of a spinal schwannoma? Sacrifice of the nerve root from which the tumor arises (which should not cause additional deficit)1 After resection, is radiotherapy indicated for extramedullary spinal lesions? No, with the exception of recurrent clear-cell meningioma (or other recurrent nonresectable meningioma) What is the prognosis after resection of an extramedullary spinal lesion? Very good; recurrence is 6% after complete resection and 17% after partial resection.2 Is there any exception to this general rule? Yes; outcome is less favorable if the patient has neurofibromatosis What is the typical presentation of a patient with an intradural intramedullary lesion? Back or neck pain in a diffuse pattern, worse at night. Children may even present with abdominal pain. Would you expect to see hydrocephalus? • In up to 15% of patients with low-grade tumors and 35% of those with high-grade lesions • Higher incidence with cervical tumors, perhaps due to fourth ventricular outflow obstruction • High concentration of protein in CSF • Arachnoidal fibrosis • Subarachnoid dissemination of tumor leading to clogging of absorptive sites What is the most common kind of intramedullary tumor? Ependymoma in adults; astrocytoma in pediatrics (usually low-grade fibrillary or pilocytic) At what age do astrocytomas tend to present? Typically in the first three decades of life, though they may occur at any time What other kinds of tumors may be found within the spinal cord? • Hemangioblastomas • Gangliogliomas • Metastases What is a ganglioglioma? A WHO grade I tumor characterized by dysplastic neuronal and glial cell elements. Eosinophilic granular bodies, calcifications, lymphoid infiltrates, and a prominent capillary network are frequently seen. They typically present in children and young adults and follow an indolent course. What is a hemangioblastoma? A slowly growing WHO grade I tumor composed of large stromal cells with abundant vacuolated cytoplasm and abundant small blood vessels that may present sporadically or in association with von Hippel–Lindau syndrome (approximately 35% of cases) What extra study is sometimes helpful (but is not mandatory) before resection of hemangioblastoma? Angiography What kind of neoplasm occurs in the spinal cord with a “pencil-shaped” appearance? Ependymoma In what region of the spinal cord would you expect to find an intramedullary subependymoma? Cervical or cervicothoracic What about an intramedullary ependymoma? Also cervical and cervicothoracic What genetic changes are common in spinal-cord ependymoma? • Loss of chromosome 12 or 14q/14 • High expression of HOX gene family members Which variety of ependymoma is found almost exclusively in the cauda equina and filum terminale? Myxopapillary ependymoma True or false: Like spinal-cord ependymoma, myxopapillary ependymoma is also WHO grade II. False; myxopapillary ependymoma is grade I. What is the average age of presentation of myxopapillary ependymoma? 36 years Range: 6 to 82 years Is it common for this lesion to erode sacral bone or affect nerve roots? No, this happens only rarely. How does this lesion typically present? As longstanding back pain How does it appear on MRI? As a sharply circumscribed, brightly enhancing lesion Fig. 36.1 Myxopapillary ependymoma: sagittal T2-weighted MRI (A) and T1 fat suppression (B) sequences. There is a visible component of hemosiderin deposits in the caudal aspect of the tumor
Spinal Tumors
36.1 Extradural
36.2 Intradural Extramedullary
36.3 Intradural Intramedullary
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






