Chapter 47 Stereotactic Radiosurgery of Vascular Malformations
• Regardless of modality, radiosurgical devices achieve the desired characteristics of small fields, fast-dose falloff, and highly accurate targeting through the use of two basic principles: superposition of beams and stereotactic targeting.
• The goal of radiosurgery for arteriovenous malformations is to deliver a high absorbed radiation dose to the nidus, while largely sparing the surrounding normal brain tissue. Endothelial damage followed by subendothelial and intimal-medial proliferation of smooth muscle cells and subsequent cellular degeneration and hyaline transformation eventually obliterate the nidus.
• The reported obliteration rate following radiosurgery ranges between 60% and 90%. The outcomes of radiosurgery for arteriovenous malformations are dose and volume dependent. The role of preradiosurgical embolization remains to be fully defined.
• Complications associated with radiosurgery for arteriovenous malformations include symptomatic radiation-induced brain damage in 8.7% (permanent in 1.8%), late cyst formation in 1.6%, and radiation-induced tumor within 10 years following radiosurgery in 0.7%.
• Radiosurgery has a smaller role for the treatment of dural arteriovenous fistulas owing to its delayed effects. For patients with cavernous malformations, radiosurgery should be used primarily in compelling cases of repeated hemorrhages from a lesion located in an inoperable site.
Arteriovenous Malformations
Management
Three management modalities are employed alone or in combination for the management of cerebral AVMs: microsurgery, embolization, and radiosurgery. Several factors should be weighed when choosing the most appropriate choice of treatment. Microsurgery should be used in superficially located nidi because it eliminates the risk of hemorrhage immediately upon a complete total extirpation. Embolization is most commonly used to reduce the size of large AVMs, making them amenable to subsequent microsurgery or radiosurgery. However, new liquid embolization materials (e.g., Onyx) have increased the chance of obliteration solely by embolization.1,2 Radiosurgery is usually reserved for small to moderate-sized AVMs located in deep or critical areas of the brain.
Role of Radiosurgery
History
The first case of AVM treated with radiotherapy was reported by Magnus.3 In a patient he operated on with an AVM at the motor cortex, he did not attempt surgical removal because of the high possibility of neurological deficits. After decompressive craniectomy, he treated the patient with radium therapy and reported that the patient was seizure-free 2 years after radiotherapy. No imaging or histological studies were available. Cushing and Bailey reported the first successful surgery on an AVM.4 Cushing explored a vascular tumor and felt that the lesion could not be attacked without fatal hemorrhage. The patient was treated with radiotherapy. He reexplored the lesion 3 years later and described that the tangle of pulsating vessels previously encountered was largely thrombosed and transformed into a multitude of small bloodless shreds which could be easily separated from the adjacent normal cortex.
There was intense interest in the use of radiation for AVMs following Cushing’s discovery, but the initial results were not encouraging. Although some studies5,6 with small numbers of cases provided evidence of the possible utility of radiation in the treatment of AVMs, most did not provide imaging or histological proof of the efficacy of radiotherapy. This led to an almost unanimous consensus in the assessment of radiation as being worthless in the management of AVMs.
With the introduction of Gamma Knife, the potential value of irradiation in vascular malformations was reassessed. Contributing factors included an increasing body of evidence that the cells constituting the vessel wall were responsive to ionizing radiation. Long-term angiographic follow-up of a small series of AVMs treated with fractionated conventional radiation by Johnson in the 1950s revealed that the AVMs were obliterated in 45% of cases.7 In 1970, the first radiosurgical treatment for an AVM was performed by Ladislau Steiner and associates at Karolinska Institute in Stockholm. The patient refused surgery, and given the patient’s renal insufficiency, the risk of surgery was considered too high. Although the intention was to deliver focused radiation to the nidus, because only small collimators were available, the feeding arteries were targeted and 25 Gy was given as the prescription dose to the 50% isodose line. On angiography 19 months after the treatment, the feeding vessels were obliterated, and the malformation no longer filled. Subsequently, larger collimators were available and could cover the AVM nidi, and more patients were treated successfully. Today more than 50,000 AVM patients have been treated with Gamma Knife radiosurgery, which has been proved to be a safe and effective treatment alternative for AVMs.
Modality
The goal of radiosurgery for AVMs is to deliver a high absorbed radiation dose to the AVM nidus, typically in a single session, while largely sparing the surrounding brain significant dose and thereby minimizing undesirable effects from the treatment. As the number of modalities for delivering radiosurgery have increased over time, so have the numbers that have been applied to the treatment of AVMs. Reports in the literature exist for AVM treatment with various radiosurgical modalities including the Gamma Knife, isocentrically mounted linear accelerators,8–11 and robotic linear accelerators (CyberKnife).12 Regardless of modality, radiosurgical devices achieve the desired characteristics of small fields, fast-dose falloff, and highly accurate targeting through the use of two basic principles: superposition of beams and stereotactic targeting.
The details of beam superposition vary by modality. In the case of the Gamma Knife, 192 (or 201, depending on the model of the unit) individual beams are precisely aimed at a focal point, or isocenter, to achieve this effect. The beams are collimated through individual beam channels. In older units, this was achieved with a combination of internal primary and secondary collimation and external “helmet”-based final collimation. In the case of the newer Perfexion model Gamma Knife, the collimator assembly is housed entirely within the main body of the unit.13
For early linear accelerators adapted for radiosurgery, finely collimated beams were achieved through the use of circular collimator “cones” that could be attached to the accessory tray of the accelerator.14 Many currently available accelerators are equipped with micro-multileaf collimators that can achieve irregularly shaped beams that can more precisely conform to the target morphology.15 Both approaches are often used with a non-coplanar arc technique, which directs the fields at the target while spreading out the overall delivered energy.16
The ability to create a focal, high-dose distribution does little good in itself if there is no way to precisely and accurately aim at the target. This problem is elegantly solved using the principles of stereotaxy. Traditionally in intracranial radiosurgery a rigid frame is fixed to the skull. This frame defines a coordinate system by which any point within the brain can be localized. Fiducial markers, which are visible in stereotactic imaging studies as part of the procedure, are directly related to this coordinate system; thus, the target can be visualized and localized in “stereotactic space.” Accuracy and precision of treatment are thus guaranteed by the precision and accuracy with which the target can be localized and the assurance that this target will not move during a treatment owing to the rigid head frame. More recent innovations in radiosurgery have included frameless stereotaxy.17 In these systems image-guidance plays a greater role both before and during the procedure. Less invasive restraint systems such as thermoplastic masks are used in place of the rigid head frame, and periodic imaging is used to track and correct for patient motion.
Histopathology
Several histological studies have described the changes of irradiated vessels with progressive narrowing and obliteration of the lumen.18 The earliest changes are endothelial damage and endothelial-intimal separation. These are followed by subendothelial and intimal-medial proliferation of smooth muscle cells with elaboration of extracellular matrix components. Cellular degeneration and hyaline transformation of vessel walls follow, and finally the vessels obliterate completely. The above-mentioned histopathological changes are correlated with time after radiosurgery and tend to occur in smaller vessels.
Gamma Knife Radiosurgery
Treament Planning
Treatment planning is the process of creating a dose distribution that conformally covers the intended target by defining one or more isocenters, or “shots,” which each contribute to the total dose distribution. It is an iterative technique requiring detailed knowledge of neuroanatomy, neuroradiology, the biological effect of single-fraction radiosurgery, and the compromises required to create a treatment that will be effective to obliterate the nidus and at the same time tolerable for the surrounding brain structures. Optimal prescription dose has been described by Steiner and associates within the range of 23 to 25 Gy.19 However, in cases with large nidi or nidi close to critical structures, the dose needed to be adjusted.
Outcomes
Following radiosurgery, angiography reveals that hemodynamic changes occur before changes in the size and shape of an AVM.20 First, the flow rate decreases progressively. This may be related to the changes in the sizes of the feeding arteries and outflow veins. The outcome of an AVM following radiosurgery may be a total, subtotal, or partial obliteration of the nidus.
Total obliteration of the AVM after radiosurgery was defined as “complete absence of former nidus, normalization of afferent and efferent vessels, and a normal circulation time on high-quality rapid serial subtracted angiography.”20 Any remaining nidus, regardless of its size, is considered partial obliteration. Subtotal obliteration of an AVM means the angiographic persistence of an early filling draining veins without demonstrable nidus.21 The early filling venous drainage suggests that some shunting persists. Our studies have shown that these subtotally obliterated AVMs have very low risk of hemorrhage in spite of the fact that per definition the AVM nidus is still patent as indicated by the shunting. It should be noted that more than 70% of them went on to obliterate completely without further treatment.21
The reported obliteration rate following radiosurgery ranged between 30% and 92%.10,22–24 One should be cautious in terms of the interpretation of the results owing to the biases injected from different cutoff time and imaging modality used to conclude total obliteration. Studies excluding patients with short follow-up, reporting only patients undergoing angiography, or including MRI as an imaging study to conclude obliteration tend to overestimate the success rate of radiosurgery.23,25,26
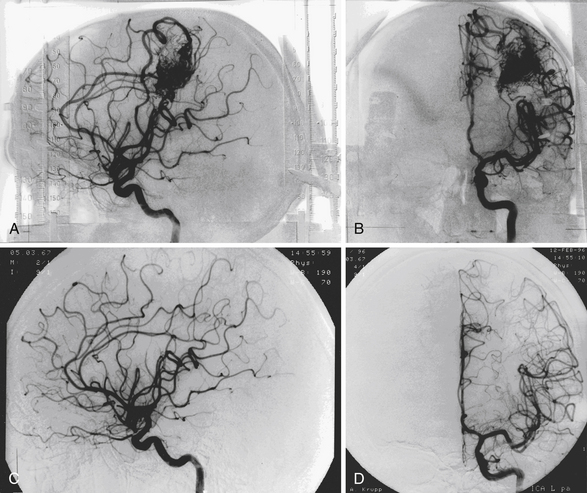
The mean follow-up after GKS was 80 months. GKS yielded a total angiographic obliteration in 552 (54%) and subtotal obliteration in 42 (4.1%) patients (Fig. 47.1). In 290 (28.3%) patients, the AVMs remained patent and in 139 patients (13.6%) no flow voids were observed on the MRI. The angiographic total obliteration was achieved in 65.2% of patients with nidus less than 3 cm3; 43.8% between 3 and 8 cm3, and 27.6% with nidus volume larger than 8 cm3. Small nidus volume, high prescription dose, and low number of isocenters are predictive of obliteration. Preradiosurgical embolization has a negative effect on obliteration.
Complications
Radiation-Induced Changes
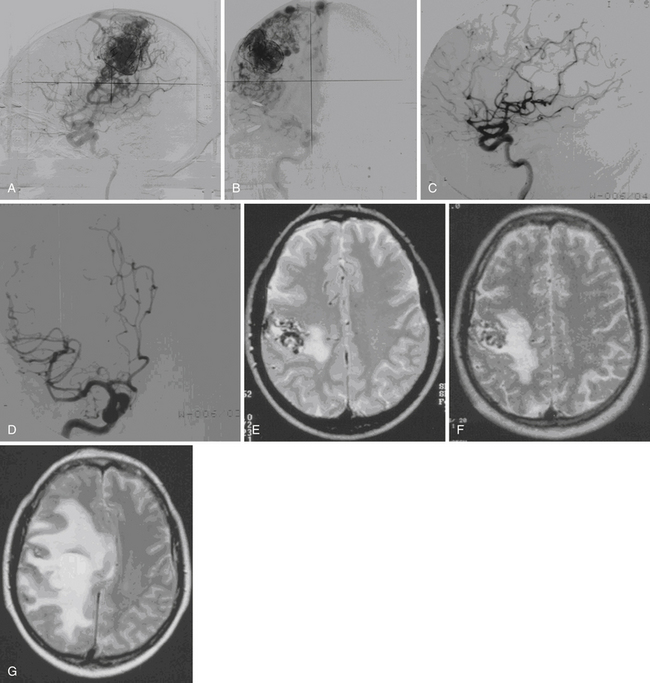
Radiation-induced change is an increased T2 signal around the AVM seen on MRI (Fig. 47.2). Radiation damage of glial cells, endothelial cell damage followed by breakdown of blood-brain barrier, excessive generation of free radicals, or release of vascular endothelial growth factors have been proposed to explain this imaging finding. The severity of radiation-induced changes on images and associated neurological deficits varies, ranging from asymptomatic, being only a few millimeters of increased T2 signal surrounding the treated nidus to massive brain edema with symptoms and signs of increased intracranial pressure. From our 1500 Gamma Knife procedures performed for AVM patients with follow-up MRI available for analysis, 34.4% of patients developed radiation-induced changes. Among them, 60% had mild (a few millimeters of increased T2 signal surrounding the nidus), 33% had moderate (compression of ventricle and effacement of sulci), and 7% had severe (midline shift) radiation-induced changes. The mean time to the development of radiation-induced changes was 13 months after GKS, and the mean duration of the changes was 22 months. Larger nidus volumes, higher prescription doses, history with preradiosurgical embolization, and nidus without previous hemorrhage were associated with higher risk of radiation-induced changes.
Cyst Formation
Cyst formation is a rare complication following GKS. Cysts that develop after resolution of previous hemorrhages or fluid cavities from encephalomalacia after surgeries should not be considered as complications related to GKS. Direct radiation injury to the perilesional brain tissue, increased permeability of the blood-brain barrier with accumulation of the exudative fluid, hemodynamic perturbations during gradual obliteration of the nidus with subsequent ischemic tissue damage, and tissue destruction due to subclinical perilesional hemorrhages have been proposed as the possible mechanisms of cyst formation. From our 1272 patients with follow-up MRI available, we found a total of 20 patients (1.6%) developing a cyst after a mean of 8.1 years after GKS. Four cysts were found in 710 patients with follow-up shorter than 5 years, eight cysts were found in 302 patients with follow-up between 5 and 10 years, and another eight cysts were found in 260 patients with follow-up between 10 and 20 years. Of the 20 patients, 18 had regular MRI follow-up and 14 (78%) of them had radiation-induced changes before the development of cysts. Six patients had large cysts and three of them were symptomatic, requiring surgery. Two patients underwent craniotomy and drainage of the cyst. The cyst wall showed no evidence of neoplasia.
Radiosurgery-Induced Neoplasia
We found two meningiomas from 1333 AVM patients treated with GKS; however, follow-up imaging was performed over a period of at least 10 years in 288 of these patients. If we conservatively estimate that radiosurgery-induced lesions would be evident within a 10-year time interval, then our incidence of radiosurgery-induced neoplasia is 2 in 2880 person-years or 69 in 100,000 person-years. Thus, there is a 0.7% chance that a radiation-induced tumor may develop within 10 years following GKS. This is less than the 1.9% risk detailed by Brada and colleagues,27 but our results encompass a follow-up period of only 10 years. The long latency and relative rarity of these lesions following radiosurgery may defy a conclusive determination of the true incidence.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree