Subaxial Cervical Involvement in Rheumatoid Arthritis
Takenori Oda
Kazuo Yonenobu
PATHOGENESIS
Rheumatoid arthritis (RA) is a systemic disease characterized by inflammatory changes of the joints, ligaments, and bones in the upper and lower extremities. Destructive changes also occur in the subaxial cervical spine due to the rheumatoid disease process. In such lesions, the diarthrodial cartilaginous facet joints are directly destroyed by inflammatory rheumatoid pannus, which extends to the adjacent structures. The interspinous ligaments are affected with attenuation. The intervertebral disks are destroyed with erosion of the end plates. The vertebral body occasionally collapses due to osteoporosis and direct invasion of the rheumatoid pannus.
Several mechanisms have been suggested to contribute to the destructive processes affecting the subaxial cervical spine. Ball hypothesized that inflammation in the neurocentral joints extends to the adjacent structures, resulting in erosion of the disk and adjacent bone (1). However, “rheumatoid inflammation of the disk” remains a controversial subject. Martel (2) suggested that primary apophyseal arthritis and ligamentous laxity cause “chronic trauma” to the diskovertebral joints, leading to destruction of the disk cartilage and vertebral end plates. Bywaters demonstrated that involvement of the interspinous bursae resulted in destruction of the spinous processes and segment hypermobility associated with disk destruction (3).
The pathogenesis of myelopathy has been evaluated using autopsy and intraoperative findings. Autopsy evaluations have indicated that cervical myelopathy results from neural compression and/or vascular impairment, rather than inflammation (4, 5, 6 and 7). Delamarter and Bohlman described three histologic types of spinal cord compression: (a) severe chronic mechanical compression showing marked mechanical distortion, flattening, and destruction of the cord with secondary Wallerian degeneration of the ascending and descending tracts but without anoxic-ischemic neuron changes; (b) vascular compression showing ischemic damage to the cord with necrosis of the lateral columns in the ischemic watershed regions supplied by anterior and posterior spinal arteries; and (c) mild mechanical compression showing focal gliosis at the site of compression without ascending or descending tract injury (6). Histopathologic studies of the spinal cord at the level of subluxation in the subaxial spine have shown demyelination and gliosis in the posterior and lateral white columns (4–7).
Factors relating to compression of the spinal cord in the subaxial cervical spine include subluxation of the cervical spine itself (8), prolapse of the disk material (8), protuberance of the ventral bone mass (8), inward bulging of the ligamentum flavum (9), infolding of the dura (10), granulation tissue within the epidural space (8,11), and constrictive band formation of the dura mater (11,12).
INCIDENCE OF SUBAXIAL INVOLVEMENT
Radiographic features in the subaxial cervical spine due to RA include narrowing of the disk space without osteophyte formation, erosion of the vertebral end plate, erosion or fusion of the facet joint, erosion and/or atrophy of the spinous process, and subluxation (Fig. 62.1). Spontaneous fusion of the adjacent vertebral bodies sometimes occurs, while collapse of the vertebral body is occasionally observed in severe cases (Fig. 62.2). According to the classical radiographic studies, narrowing of the disk space without osteophyte formation and end plate erosions were evident in 18% to 25% and 14% to 20% of patients with RA, respectively (13, 14 and 15). Destructive changes in the facet joint were present in 15% to 32% (13, 14 and 15), while fusion of the facet joint was evident in 4% to 17% of patients with RA (15,16). Subaxial subluxation (SAS) is one of the characteristic instabilities of the rheumatoid cervical spine. The prevalence of SAS is lower than that of subluxation in the upper cervical spine (14, 15, 16, 17, 18, 19, 20 and 21). SAS is evident in 7% to 27% of patients with RA (13, 14, 15, 16, 17, 18, 19, 20 and 21). Several longitudinal studies have shown that the prevalence of SAS increases with the duration of RA (16, 17, 18, 19 and 20). Although subluxation may develop at any segment of the subaxial cervical spine, segments C3-C4 and C4-C5 are predominantly affected (15,18, 19 and 20). Subluxations sometimes appear at multiple segments in a “stepladder” fashion, particularly among patients with severe disease.
CLINICAL MANIFESTATIONS
Clinical manifestations due to cervical involvements in RA include pain, neurologic deficits, and death. Local neck pain is caused by involvement of the subaxial cervical spine, sometimes associated with local tenderness and crepitations. Symptoms due to insufficient circulation through the vertebral artery, such as vertigo and dark vision, are occasionally recognized.
Pain often refers into the paracervical, suprascapular, and interscapular areas. Although pain at the occipital area frequently occurs in patients with RA, such pain usually implies involvement of the upper cervical spine rather than the subaxial cervical spine. Severe pain along with difficulty maintaining a sitting position is occasionally induced, especially in patients with gross destruction of the vertebral bodies. In such patients, concomitant shortening of the neck and/or torticollis is often seen. Local pain was classified into four grades (Table 62.1) by Ranawat et al. (22).
Involvement of the subaxial cervical spine causes varying degrees of myelopathy, radiculopathy, and radiculo-myelopathy. Neurologic symptoms may be vague and can be multiple. Typical symptoms associated with myelopathy include numbness or diffuse paresthesia in the hands and feet, motor weakness in the upper and lower extremities, and bladder and bowel dysfunction. A radicular distribution of sensory and motor disturbances may predominate in SAS in the early stages. However, diagnosis in these early stages, and even in later stages, can be difficult because
symptoms due to articular involvement, tenosynovitis, tendon rupture, and peripheral neuropathy are already present in patients with RA. Neurologic examination is essential to diagnose myelopathy and radiculopathy but may sometimes be confounded by peripheral rheumatoid disease. Myelopathy should be suspected in patients with RA when levels of activities of daily living fall along with development or increasing numbness in the hands and feet without worsening of peripheral articular deformities or systemic inflammatory condition. Subjective feeling of weakness or loss of endurance should not be ignored when myelopathy is suspected. Lhermitte’s sign, representing an electric sensation radiating into the body usually with flexion of the neck, sometimes occurs with SAS. Loss of vibration and proprioceptive sensation is observed when the posterior column of the spinal cord is affected by compression. Meijers et al. (23) stressed a “marble sensation” in the limbs and trunk, with a disturbance of deep sensation as one of the “alarm signs” indicating spinal cord damage.
symptoms due to articular involvement, tenosynovitis, tendon rupture, and peripheral neuropathy are already present in patients with RA. Neurologic examination is essential to diagnose myelopathy and radiculopathy but may sometimes be confounded by peripheral rheumatoid disease. Myelopathy should be suspected in patients with RA when levels of activities of daily living fall along with development or increasing numbness in the hands and feet without worsening of peripheral articular deformities or systemic inflammatory condition. Subjective feeling of weakness or loss of endurance should not be ignored when myelopathy is suspected. Lhermitte’s sign, representing an electric sensation radiating into the body usually with flexion of the neck, sometimes occurs with SAS. Loss of vibration and proprioceptive sensation is observed when the posterior column of the spinal cord is affected by compression. Meijers et al. (23) stressed a “marble sensation” in the limbs and trunk, with a disturbance of deep sensation as one of the “alarm signs” indicating spinal cord damage.
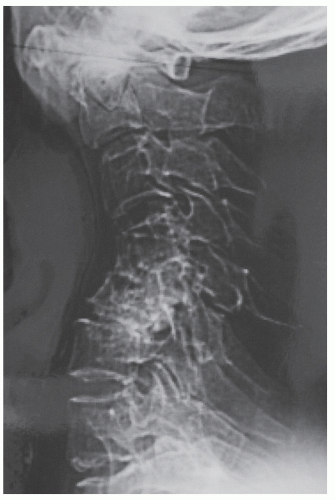 Figure 62.2. A patient with RA and subaxial kyphotic deformity. Collapse of the C4 vertebral body with dorsal subluxation at C4-C5 is evident. The patient also has ventral atlantoaxial subluxation. |
TABLE 62.1 Ranawat Criteria for Pain and Neurologic Assessment | |||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||
Attempts to grade neurologic deficits in patients with RA have been hampered due to dysfunction associated with the disease itself. At present, the neurologic grading system devised by Ranawat et al. (22) (Table 62.1) is widely used but is too broad to be really useful. Patients are categorized as unimpaired (class I), minimally impaired (class II), or catastrophic (class III), providing insufficient stratification. Several functional assessments are also available, such as the Nurick grading scale, Zeidman and Ducker (24) modification of the Nurick grading scale, the myelopathy disability index, and the scoring system created by the Japanese Orthopaedic Association, but grading systems for evaluating neurologic impairment in patients with RA are currently inadequate.
DIAGNOSTIC IMAGING
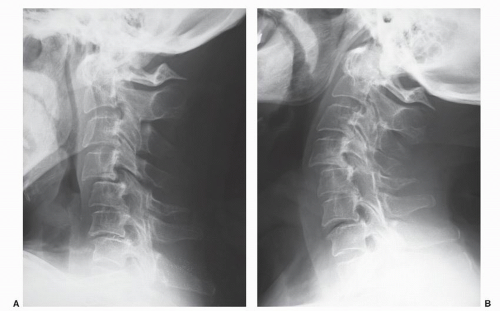
Plain radiography is the starting point for imaging evaluation of subaxial cervical involvement. This modality should ideally be one of the routine screening items for patients with RA to identify cervical involvement before symptom onset. Characteristic radiographic features in the subaxial cervical spine are narrowing of the disk space without osteophyte formation, erosion of the vertebral end plates, erosion or fusion of the facet joints, erosion and/or atrophy of the spinous processes, and subluxation. A neutral lateral radiograph alone is inadequate to detect either atlantoaxial subluxation or SAS, as ventral or dorsal subluxation is sometimes reduced in a neutral position. Dynamic lateral radiographs including both flexion and extension positions are essential to determine the presence or absence of subluxation and the degree of instability (Fig. 62.3 and 62.3). In
general, vertebral displacement of 3 mm or more is considered abnormal. The incidence of SAS using this criterion in patients with RA is reportedly about 20% (18,21). Measuring angular and translational movements at the SAS level by dynamic lateral radiography is important for understanding dynamic compressive factor affecting the spinal cord.
general, vertebral displacement of 3 mm or more is considered abnormal. The incidence of SAS using this criterion in patients with RA is reportedly about 20% (18,21). Measuring angular and translational movements at the SAS level by dynamic lateral radiography is important for understanding dynamic compressive factor affecting the spinal cord.
As plain radiographs cannot evaluate soft tissues such as intervertebral disks, ligaments, and neural elements, additional radiologic evaluations are required. Magnetic resonance imaging (MRI) is currently the most valuable technique to clarify the status of the spinal cord and surrounding structures (Fig. 62.3). MRI is performed in a
neutral supine position in daily clinical practice. However, Reijnierse et al. (30) stated that MRI in flexion has added value in evaluating the cervical spine of patients with RA. They showed significant narrowing of the subarachnoid space, which may be indicative of the development of neurologic dysfunction, at the atlantoaxial and subaxial level below C2 on flexion views. Contrast-enhanced T1-weighted MRI can discriminate between joint effusion and various forms of pannus in patients with RA (31). Pannus formation is primarily observed around the odontoid process in the rheumatoid cervical spine, although pannus formation in the subaxial spine has been reported (32).
neutral supine position in daily clinical practice. However, Reijnierse et al. (30) stated that MRI in flexion has added value in evaluating the cervical spine of patients with RA. They showed significant narrowing of the subarachnoid space, which may be indicative of the development of neurologic dysfunction, at the atlantoaxial and subaxial level below C2 on flexion views. Contrast-enhanced T1-weighted MRI can discriminate between joint effusion and various forms of pannus in patients with RA (31). Pannus formation is primarily observed around the odontoid process in the rheumatoid cervical spine, although pannus formation in the subaxial spine has been reported (32).
Myelography and computed tomography (CT) remain important diagnostic tools for evaluation. The dynamic status of the spinal cord is easily evaluated using myelography. Multiplanar reconstruction CT has recently become available, providing further useful information about three-dimensional bony abnormalities, such as erosive changes of the facet joints and vertebral bodies (Fig. 62.3).
RISK FACTORS FOR DEVELPOMENT OF SUBAXIAL SUBLUXATION AND MYELOPATHY
Factors associated with the development of SAS include the duration and severity of RA. Several longitudinal studies have shown that the prevalence of SAS increases with longer duration of disease (16, 17, 18, 19 and 20). In addition, SAS is more frequently associated with a more severe degree of RA, particularly in patients with mutilans deformities of the hands and feet (18, 19 and 20). Fujiwara et al. (19) noted that occurrence of SAS correlated closely with higher serum levels of C-reactive protein, a greater number of joints showing radiographic erosion, a greater degree of hand involvement (decreased carpal height ratio), and disease subset based on serum C1q levels and number of joints with erosion. In that study, mean serum levels of C-reactive protein, number of joints with erosion, and carpal height ratio in patients with SAS were 3.7, 50.8, and 0.36 mg/dL, respectively. Incidences of SAS in each disease subset were 0% for least erosive disease, 12% with more erosive disease, and 39% in mutilating disease.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree