Chapter 64 Subaxial Cervical Spine Injuries
Cervical fractures are found in approximately 3% of all trauma patients.1 The subaxial spine accounts for the majority of cervical injuries, making up approximately 65% of fractures and more than 75% of all dislocations.2 Approximately 150,000 cervical spine injuries occur annually in North America. In the same region, there are 11,000 new spinal cord injuries (1 per 25,000 people) annually.3 Trauma in the subaxial cervical spine accounts for almost half of all cervical spine injuries and the largest proportion of new traumatic spinal cord injuries.
Anatomy
Various authors have modeled the cervical spine as either a two-column4,5 or three-column system.6,7 Although both systems have merits, the two-column system probably provides the best understanding of the common injury patterns seen in the lower cervical region. The two-column spine consists of an anterior column and a posterior column. The anterior column contains the anterior longitudinal ligament, intervertebral disc, vertebral body, and posterior longitudinal ligament. The posterior column consists of the posterior bony elements, facet capsules, interspinous and supraspinous ligaments, and ligamentum flavum. The most important stabilizer of the anterior column is the anulus fibrosus, whereas the facet joints are the most important stabilizers of the posterior column.5
The ligamentous structures provide a check to hypermobility during normal motion. For example, the anterior longitudinal ligament and ventral anulus become taut during extension, whereas the posterior column ligamentous structures act as a tension band during flexion. Compressive loads are resisted by the vertebral bodies, intervertebral discs, and facet joints. Pure tensile loads are resisted by the anulus, interspinous ligament, ligamentum flavum, and facet capsules. Flexion is resisted by the interspinous ligaments, facet capsules and facet joints, anterior longitudinal ligament, and posterior anulus. Extension is also resisted by the bony block of the facet joints. Maximal sagittal plane translation occurring under physiologic loads is 2 to 2.7 mm.5 Lower cervical spine injuries can be understood as a failure of the structures designed to resist the forces and moments occurring at the time of the injury. By observing the pattern of bony and ligamentous disruption on imaging studies, the treating physician may generally deduce the force vectors that acted to create the injury pattern and also begin to gain an understanding of the “personality” of the injury, and thus the tendency for displacement under physiologic loads.
Injury Classification
The simplest method of discussing injuries to the cervical spine is to use radiographic descriptions of the injury. Hence, terms such as compression fracture, burst fracture, teardrop fracture, or facet dislocation remain in common usage, although these descriptive terms provide only a broad overview of the injury and do not provide information on injury severity, neurologic status, or treatment options. Mechanistic classifications are useful in promoting an understanding of injury pathomechanics and also assist the surgeon in designing a rational treatment approach, although biomechanical validation of the presumed injury mechanisms is generally lacking. Despite this limitation, these classification schemes are useful in clinical practice and remain the preferred scheme at most trauma centers managing large volumes of cervical trauma.
Although many classification schemes have been proposed, this chapter reviews several schemes that have strong historical significance or practical utility, or are recent additions to the literature, including those proposed by Whitley and Forsyth (1960),8 Allen et al. (1982),9 Harris et al. (1986),10 Anderson et al. (2007),11 and, finally, Vaccaro et al. (2007).3
Whitley and Forsyth8 described a mechanistic classification of cervical spine injuries in 1960 based on a review of 159 patients with cervical fractures. In their scheme, fractures were divided into flexion injuries, extension injuries, combined flexion-extension injuries, burst-type injuries, and direct trauma. The authors further divided flexion and extension injuries into those occurring with and without compression. This classification system retains historical importance for promoting a mechanistic thinking about cervical spine injuries.
White and Panjabi5 devised an early checklist for instability after cervical trauma. They hypothesized that a similar injury mechanism might produce different injury patterns because of the complex multidirectional forces, moments, and positions of the affected joints at the time of trauma. They devised a point-based system for assessing stability in lower cervical spine injury, summarized in Table 64-1. To use their system, radiographic criteria, physical examination, and a stretch test are required. A score of 5 or more points in this system is said to predict spinal instability.12
TABLE 64-1 Diagnosis of Clinical Instability in the Middle and Lower Cervical Spine
| Element | Point |
|---|---|
| Anterior elements destroyed or unable to function | 2 |
| Posterior elements destroyed or unable to function | 2 |
| Positive stretch test | 2 |
| Radiographic criteria | |
| Flexion-extension radiographs | |
| Sagittal plane translation > 3.5 mm | 2 |
| Sagittal plane rotation > 20° | 2 |
| Resting radiographs | |
| Sagittal plane displacement > 3.5 mm | 2 |
| Relative sagittal plane angulation > 11° | 2 |
| Developmentally narrow spinal canal | 1 |
| Abnormal disc narrowing | 1 |
| Spinal cord damage | 2 |
| Nerve root damage | 1 |
| Dangerous loading anticipated | 1 |
A total of five or more points indicates clinical instability.
The stretch test described by White and Panjabi is performed by securing the patient’s head in halter or tong traction with a roller beneath the head to reduce friction. Initial lateral radiographs of the cervical spine with 10 pounds of traction are carefully analyzed to rule out a disruption of the occipitocervical junction. Serial weight is sequentially added in 10-pound increments, performing neurologic testing with each addition of weight. The end point of the test is reached when “instability” is noted on radiographs or when there is a change in neurologic examination, or when the weight limit (65 pounds or one-third body weight) is reached. Instability on the stretch test is defined as distraction of a vertebral interspace by 1.7 mm or greater or a change in segmental alignment of 7.5 degrees or greater compared with the baseline radiographs.12 Although advocated by several authors, this type of test has not become a standard method for analyzing stability in most trauma centers because of its cumbersome nature and concerns regarding iatrogenic neurologic injury.
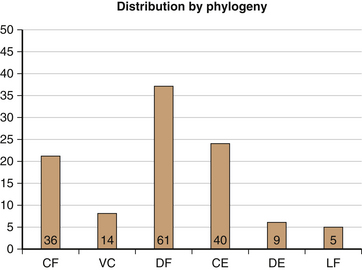
In 1982, Allen et al.9 published a mechanistic classification system that has been widely used in recent years. They based their scheme on the clinical review of 165 patients with indirect lower cervical spine trauma. In this system, subaxial cervical injuries were divided into “phylogenies” based on a common proposed injury mechanism, with an orderly progression of severity ranging from mild to severe. They included six injury phylogenies—compressive flexion, vertical compression, distractive flexion, compressive extension, distractive extension, and lateral flexion (Fig. 64-1). The terms used for each category describe the attitude of the cervical spine at the time of injury and the dominant force vector. The authors acknowledged the presence of minor force vectors that may cause separate or combined injuries. “Rotation” in this system was described as localizing an injury asymmetrically to one side rather than acting as an independent force vector. In general, the risk and severity of neurologic injury were noted to increase with increasing severity stages (Box 64-1).
BOX 64-1 Lower Cervical Spine Trauma Phylogeny Classification System*
1 Compressive Flexion (CF)
CFS1: rounded shape to the anterior superior vertebral body without any posterior ligamentous disruption
CFS2: “beaked” appearance of the anterior vertebral body with loss of anterior height due to compression failure
CFS3: an oblique fracture line traversing from the anterosuperior vertebral body to the inferior end plate
CFS4: up to 3 mm of posterior translation of the posterior vertebral body into the neural canal
CFS5: >3 mm displacement of the posterior aspect of the vertebral body into the neural canal
3 Distractive Flexion (DF)
DFS1: forward subluxation of the upper facet in the motion segment with widening of the space between the spinous processes
DFS2: unilateral facet dislocation demonstrating up to 25% forward subluxation of the vertebral body in the motion segment
DFS3: bilateral facet dislocation with approximately 50% anterior subluxation of the upper vertebra in the motion segment
DFS4: gross anterior displacement of the upper vertebra on the lower vertebra in the motion segment, creating the “floating vertebra”
4 Compressive Extension (CE)
CES1: unilateral vertebral arch fracture (pedicle, facet, and/or lamina) with or without rotational displacement of the vertebral body
CES2: bilateral laminar fractures, often at multiple contiguous levels but without evidence of other soft tissue failure
CES3: bilateral disruption of the articular pillars (pedicle, facet, and/or lamina) without displacement
CES4: partial forward subluxation of the fractured vertebra on the vertebra below
Adapted from Allen BL, Ferguson RL, Lehmann TR, et al: A mechanistic classification of closed indirect fractures and dislocations of the lower cervical spine. Spine (Phila Pa 1976) 7:1–27, 1982.
In 1986, Harris et al.10 proposed a similar classification system that placed injuries into groups related to a predominant causative force vector or combination of force vectors (Box 64-2). Unlike the Allen scheme, Harris et al. included the rotational vectors combined with flexion or extension but did not emphasize the role of distractive forces.
BOX 64-2 Mechanism of Cervical Spine Injuries
From Harris J, Edeiken-Monroe B, Kopaniky D: A practical classification of acute cervical spine injuries. Orthop Clin North Am 17:15–30, 1986.
In 2007, Anderson et al.11 presented the Cervical Spine Injury Severity Score (CSISS), a scheme allowing the observer to grade the degree of osteoligamentous disruption of the injury based on a four-column concept of the cervical spine modified from the work of Louis. The concept is to correlate increasing amounts of osseous separation or ligamentous disruption with a higher degree of instability using an analogue scale, with the goal of identifying patients who would benefit from surgical stabilization. The authors found excellent intraobserver and interobserver reliability when applying their scheme to a cervical trauma population, perhaps owing to the critical analysis of each of the four columns of the cervical spine. When analyzed, the CSISS was noted to perform well for all fracture types and for a spectrum of injuries from relatively minor to grossly unstable.11 Patients with scores greater than 7 points were generally subjected to surgical stabilization, suggesting the system produced consensus regarding the need for operative stabilization.
Vaccaro et al.3 presented a point-based scheme for evaluating subaxial cervical injuries in 2007. The authors reviewed the positive elements of prior classification systems and used the expertise of an experienced group of clinicians in the Spine Trauma Study Group (STSG) to devise a working system known as the Subaxial Injury Classification (SLIC; Table 64-2). The SLIC system applies a severity ranking in three specific areas: (1) a morphologic description of the bony fracture pattern, (2) a rating of the discoligamentous complex, and (3) a rating of the patient’s neurologic status.3 By applying points in each area, the authors were able to produce a severity score that was used to separate treatment into surgical and nonsurgical categories.
TABLE 64-2 Subaxial Cervical Spine Injury Classification System
| Characteristic | Points |
|---|---|
| Morphology | |
| No abnormality | 0 |
| Compression | 1 |
| Burst | 1–2 |
| Distraction (e.g., facet perch, hyperextension) | 3 |
| Rotation/translation (e.g., facet dislocation, unstable teardrop or advanced-stage flexion compression injury) | 4 |
| Discoligamentous Complex | |
| Intact | 0 |
| Indeterminate (e.g., isolated interspinous widening, MRI signal change only) | 1 |
| Disrupted (e.g., widening of disc space, facet perch or dislocation) | 2 |
| Neurologic Status | |
| Intact | 0 |
| Root injury | 1 |
| Complete cord injury | 2 |
| Incomplete cord injury | 3 |
| Continuous cord compression in setting of neurodeficit (neuromodifier) | 1 |
Adapted from Vaccaro A, Hulbert J, Patel P, et al: The subaxial cervical spine injury classification system: a novel approach to recognize the importance of morphology, neurology, and integrity of the disco-ligamentous complex. Spine (Phila Pa 1976) 32:2365–2374, 2007.
Spinal Stability
Spinal stability is one of the most fundamental issues affecting treatment decisions for cervical trauma, yet an absolute method to define stability remains elusive. Many attempts have been made to define instability by various researchers. Spinal stability was defined by White and Panjabi13 as “the ability of the spine under physiologic loads to limit patterns of displacement so as not to damage or irritate the spinal cord or nerve roots and, in addition, to prevent incapacitating deformity or pain due to structural changes.” Although this definition is logical, it is notoriously difficult to apply in clinical practice.13 In contrast, Anderson et al.11 used a continuous scale for grading stability of the bony and ligamentous structures in the CSISS. This approach seems to have good reliability, but the exact point at which an injury becomes unstable still remains imprecise. Allen et al.9 defined instability as “greater than normal range of motion within a motion segment” and viewed each injury pattern as a spectrum. However, clinical judgment and experience on the part of the treating physician remain critical in defining stability.9
Holdsworth4 and others14,15 have emphasized the importance of the posterior ligamentous complex in conferring stability to the spine. In their description, the disruption of the posterior ligamentous complex is the primary determinant of instability. Instability comprises a spectrum, with rare cases of clinically significant instability not being recognizable on initial imaging. Herkowitz and Rothman16 coined the term subacute instability to describe patients with negative initial radiographs and neurologic examinations who were subsequently noted to have unstable cervical injuries on follow-up radiographs. This situation was thought to be due to initial muscle spasm masking the instability. Because of the risk of a missed injury, early removal of cervical immobilization was discouraged. Instead, it was recommended that a patient with a suggestive trauma mechanism and neck pain remain in a secure cervical collar immobilization until the muscle spasm has resolved, at which time clinical and flexion and extension radiographs can be obtained.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree