| 151 | Supraclavicular and Infraclavicular Brachial Plexus Exposure and Procedures |
♦ Preoperative
Operative Planning
- Review imaging (magnetic resonance imaging [MRI] or computed tomography-myelogram for trauma, MRI for tumor, and chest x-ray and MRI brachial plexus [magnetic resonance neurography] and neck for entrapment cases)
- Correlate history, clinical examination, electromyography findings and imaging studies
Equipment
- Microinstruments for nerve repair
- Microbackgrounds
- Leksell rongeurs
- Colored vasoloops around nerves and vessels; doubled umbilical tape or laparotomy pad for clavicle; Penrose drain for passage of nerve grafts
- Ligaclips applied to vasoloops to prevent heavy retraction on nerves
Operating Room Set-up
- Headlight
- Loupes
- Microscope
- Intraoperative electrodiagnostic testing (e.g., nerve action potentials [NAPs], motor evoked potentials [MEPs], somatosensory evoked potentials, electromyograms)
- Underbody Bair Hugger (Arizant Healthcare, Eden Prairie, MN)
- Sequential compressive devices/thromboguards if one leg is not prepped
- Bipolar and Bovie cautery
Anesthetic Issues
- Arterial line for blood pressure monitoring
- Foley catheter
- Large intravenous access, though often limited to a single limb
- Intravenous antibiotics should be given 30 minutes prior to incision and continued for 24 hours postoperatively
- General anesthesia
- Avoid nondepolarizing muscle relaxants and nitrous oxide other than during intubation
- Occasional use of low dose nondepolarizing muscle relaxants during MEP recordings
- Warm room if combined free functioning muscle transfer also being performed
- Avoid nondepolarizing muscle relaxants and nitrous oxide other than during intubation
♦ Intraoperative (Fig. 151.1)
General Principles
- Know anatomy
- Know limitations as a surgeon
- Good lighting
- Broad exposure necessary
- Identify normal anatomy first, and then work toward pathology
- Be prepared
- Team approach
Positioning
- Endotracheal tube and temperature probe to opposite side of operative site and tape above ears
- Patient supine with head resting on a donut
- Neck extended slightly
- Head turned to opposite side of surgery
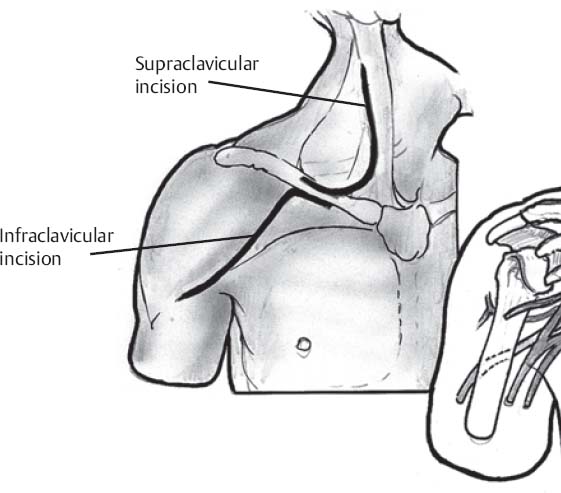
Fig. 151.1 Schematic illustrating an extensive brachial plexus exposure.
- Back of table raised to semi–beach chair position with legs dropped
- Bump between shoulder blades if patient is supine
- If patient is slightly lateral to facilitate exposure to posterior shoulder region for potential posterior approach, place folded blanket under torso
- Operating surgeon stands at the head of the table with one assistant on the same side of the table and one assistant across table
- Ipsilateral hand in stockinette with nonperforating towel clamp clipped to chest (available as necessary)
- Opposite arm tucked
- Mayo stand available for improved access to axilla or arm, or as an extra instrument tray when separate surgical teams are working
- Heels and arms well padded
- Patient secured to operating room bed with safety straps around waist
- Access to both legs for sural nerve grafts (with tourniquets), chest, opposite neck, posterior shoulder, depending on type of exposure(s) and planned procedure(s)
- Bump placed under buttock to aid exposure to same side sural harvest during harvest (placed immediately before sural harvest and removed after wound closure)
- Bump between shoulder blades if patient is supine
Planning of Sterile Scrub and Preparation
- Prep entire arm circumferentially with stockinette
- U-drape around neck and around chest maintaining sterile field
- Cut up Ioban pieces affixed to sterile blue towels around operative site creating sterile field
- Chest prepped to midline and to posterior axillary line
- Legs prepped circumferentially above knees
Approach to Supraclavicular Brachial Plexus (Fig. 151.1)
- Transverse incision in Langer’s line several fingerbreadths above the clavicle spanning from trapezius to sternocleidomastoid muscle; or oblique incision parallel to lateral border of sternocleidomastoid from just below mastoid process to clavicle with a transverse limb laterally at the level of the clavicle to form zigzag; either incision may be incorporated with an infraclavicular (deltopectoral) incision (see below).
- Divide platysma and develop subplatysmal flaps.
- Retract external jugular vein.
- Protect supraclavicular nerves and cervical plexus as possible. Cervical plexus seen in superficial dissection can be traced to C3–C4 origins.
- Mobilize clavicle. Release cleidal head of sternocleidomastoid muscle. Suprascapular vessels need to be ligated. Subclavius muscle may be divided. Osteotomy of the clavicle is rarely necessary. In the rare circumstance where retroclavicular exposure (such as for a large tumor of the divisions is encountered), predrilling, prescrewing, and preplating should be done before the osteotomy, and a low contour reconstructive plate should be utilized. The surgeon should be experienced in fixation or should seek assistance from an orthopedist.
- Identify omohyoid and dissect it proximally and distally. Retract or divide omohyoid; if omohyoid is divided, place tag stitches on both ends, divide muscle at tendon, and retract stitches with tension to aid exposure.
- Dissect fat pad and mobilize laterally.
- Identify phrenic nerve (runs obliquely and is only major nerve to run inferiorly and medially) on anterior scalene and mobilize. Stimulation of phrenic nerve should provide hemidiaphragm contraction.
- Follow phrenic nerve proximally to its C5 contribution and identify upper trunk and C6.
- Then, if needed, obtain proximal exposure of C5 and C6 to foramina.
- Divide or resect anterior scalene. Leksell rongeurs can assist biting away tip of transverse process (careful to avoid vertebral artery). Proximal branches to dorsal scapular nerve (C5). Long thoracic nerve may be seen arising from the posterior surface of the C5–C7 roots before it penetrates the middle scalene; dissection on undersurface of C6 especially is easiest to expose long thoracic nerve.
- Trace upper trunk distally to suprascapular nerve (follows omohyoid posteriorly toward scapula) and anterior and posterior divisions of upper trunk. Retroclavicular dissection will require retraction of mobilized clavicle.
- For exposure of C7–T1, ligate transverse cervical artery typically necessary when identifying middle trunk and C7. C7 and middle trunk are more medial and lie deeper to upper trunk.
- For C8 and T1, palpate, identify, and retract subclavian artery (posterior to scalene anterior) and vein (anterior to scalene anterior). Dissect lower trunk, C8, and T1. Be careful of pleura.
- Then, if needed, obtain proximal exposure of C5 and C6 to foramina.
Spinal Accessory Nerve
- May be identified 1 cm above the point where the great auricular nerve wraps around the sternocleidomastoid (near the posterior cervical lymph nodes) or more distally along the medial border of the trapezius above the clavicle. The proximal location is the typical site of neural injury during lymph node dissections. The distal location is my preferred site to identify the nerve during nerve transfer.
- Spinal accessory nerve can be traced distally and deeply into the trapezius. Long segment of nerve can be exposed if necessary to gain length as neurotizer (long enough to extend several centimeters under clavicle if necessary).
- If used as neurotizer, major proximal branches from spinal accessory nerve should be preserved.
Approach to Infraclavicular Brachial Plexus (Fig. 151.1)
- Surgical incision utilizing deltopectoral (deltoid and pectoralis major) interval
- A portion of clavicular attachment of pectoralis major may be released to facilitate exposure; interval is most easily identified proximally (especially useful in revision surgery).
- Preserve cephalic vein (usually mobilized and retracted laterally).
- Deepening dissection in deltopectoral approach exposes pectoralis minor and clavipectoral fascia.
- Pectoralis minor (arising from coracoid and inserting into 3rd, 4th, and 5th ribs) mobilized using blunt finger dissection, divided at tendon. Tagged stitch in pectoralis minor facilitates retraction of it and subsequent reapproximation at closure. Cords are situated beneath the pectoralis minor (named for their location to the axillary artery at the level of the coracoid).
- Fat pad above brachial plexus mobilized and retracted
- Release of the proximal 1 to 2 cm of the pectoralis major tendon is often done.
- Infraclavicular plexus dissection relatively easy when there is no scarring, exceedingly difficult when revision surgery (previous vascular repair, etc.). When scarring is problematic, release of the pectoralis major insertion from the humerus may be necessary. A cuff of tendon should be maintained and tagged prior to release. The neurovascular elements can be identified distally in more normal tissue planes. The pectoralis major tendon should be repaired at the end of the operation.
- Authors’ preference: identify lateral cord first (and its branches), then axillary artery, medial cord and its branches, and finally posterior cord and its branches.
- Lateral cord
- Lateral pectoral nerve may be seen
- Terminal branches of lateral cord then identified
- Musculocutaneous nerve is protected; proximal branch to coracobrachialis identified and mobilized. Be aware of many variations of musculocutane-ous nerve.
- Lateral cord contribution to median nerve (“sensory root” and motor to median innervated forearm and wrist muscles)
- Axillary artery (the “bouncing nerve”)–mobilized in red vasoloop
- Thoracoacromial artery (useful for free muscles) may be identified just medial to pectoralis minor
- Axillary vein typically not specifically mobilized
- Medial cord
- Medial brachial cutaneous (smaller) and medial antebrachial cutaneous (larger) nerves may be seen. Medial pectoral nerve (to sternocostal head of pectoralis major and pectoralis minor) also may be identified; associated with lateral thoracic artery; joins with lateral pectoral distally.
- Terminal branches of medial cord then identified
- Ulnar nerve
- Medial cord contribution to median nerve (“motor root” to median innervated hand muscles)
- Identifying the “Mayo ‘M’”–two roots of median nerve encircle axillary artery and bring plexus elements anterior to the artery
- Posterior cord
- Thoracodorsal nerve (to latissimus dorsi muscle) and subscapular nerves may be seen
- Terminal branches of posterior cord then identified
- Axillary nerve–accompanied by posterior humeral circumflex artery through quadrangular space
- Radial nerve–exits axilla posteriorly via triangular space:
- May need anterior and posterior exposures to see axillary and radial nerves
- Occasionally, a limited axillary approach can be performed to resect benign tumors (extrinsic or intrinsic) in the vicinity of terminal branches of the brachial plexus. Do not let cosmesis limit exposure or compromise outcomes.
- May need anterior and posterior exposures to see axillary and radial nerves
- Lateral cord
Medial Exposure of Nerve Branches in Proximal Arm
- Medial longitudinal incision in proximal arm to point near axillary line
- Medial antebrachial cutaneous nerve, median nerve (deep to brachial artery), ulnar nerve, and musculocutaneous nerves (between biceps and coracobrachialis) can be identified quickly all within several centimeters of each other.
- Median nerve is the largest nerve in the field.
- No branches from the median or ulnar nerve arise at this level.
- Musculocutaneous nerve can be traced to biceps, brachialis, and lateral antebrachial cutaneous nerve. Brachialis branch can often be traced proximally to a common takeoff with the biceps branch. This group of fascicles can then be traced proximally above the axillary line, still separate from the lateral antebrachial cutaneous fascicular group.
- Radial nerve and major branches to the triceps (especially to long head) can also be identified easily within the proximal portion of this exposure, posterior to the humerus just above the triceps.
- Hemostasis
- If a drain is placed, it should be positioned away from nerve repairs.
- Divided muscles/tendons (such as the omohyoid, pectoralis minor, and pectoralis major muscles) should be reapproximated. The divided pectoralis minor and pectoralis major (when necessary) should be repaired using heavy nonabsorbable sutures.
- Chest x-ray should be obtained intraoperatively in concern for pneumothorax (such as after intercostal nerve harvesting).
- Wounds should be closed in anatomic layers.
- Subcuticular suture with Steri-Strips
- Dry sterile dressing
- Shoulder immobilizer is utilized in cases of nerve repair/reconstruction.
♦ Postoperative
- Immobilizer for 3 weeks (following nerve repair/reconstruction)
- Physical therapy and range-of-motion activities may be initiated for hand even while patient is in immobilizer; for other joints after period of immobilization
- Long-term follow-up with clinical and electromyography testing is necessary.
- Sensory and motor re-education may be helpful during recovery.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue








